How to evaluate sexual health in cancer patients: development of the EORTC sexual health questionnaire for cancer patients
Introduction
An individual’s sexual response can be affected in a number of ways that involves the physical, psychological, interpersonal, and behavioural aspects of a person. The most common sexual problems for people who have cancer are loss of desire for sexual activity in both men and women, problems achieving and maintaining an erection in men, and pain with intercourse in women (1). Unlike many other physiological side effects of cancer treatment, sexual problems do not tend to resolve within the first year or two of disease-free survival (2-5) rather, they may remain constant and fairly severe or even continue to increase. Long-term effects of different treatment on sexual functioning have been studied in cervical cancer survivors (6,7). Existing research has mainly focused on women who have breast or gynecologic cancer and men who have prostate cancer (8). Less is known about how other types of cancers affect sexual health. Although it is unclear how much sexual problems influence a survivor’s rating of overall health-related quality of life, these problems are clearly bothersome to many patients and interfere with a return to normal post-treatment life. In 2014, the National Cancer Institute at the National Institutes of Health published data on some form of sexual dysfunction occurring in 40-100% of persons diagnosed with cancer (1,9-13). Sexual dysfunction is less broadly defined than sexuality and is characterized by dysfunction of one of the four phases of the sexual response cycle, or pain during intercourse (14,15). The World Health Organization (WHO) defines sexuality as a central aspect of being human throughout life and encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy and reproduction. Comparatively, sexual health is defined as a state of physical, emotional, mental and social well-being relating to sexuality, and is not merely the absence of disease, dysfunction or infirmity (16). Cancer and cancer therapies are frequently associated with changes in sexual health. However, there is a lack of consensus regarding valid outcome measures for assessing sexual functioning in cancer patients (12,17). There is no single self-report measure that can be recommended for cancer clinical trials (18,19) on the basis of a broader definition of sexual health. Several modules for various cancer sites (e.g., breast, gynecologic, prostate) were developed by the European Organisation for Research and Treatment of Cancer Quality of Life Group (EORTC-QLG) which include a limited number of sexual functioning items. The U.S. National Institutes of Health PROMIS® Network has already developed a self-report measure of sexual function and satisfaction for cancer populations (20). However, the existing questionnaires do not cover the whole range of sexual health. Currently, there is no comprehensive instrument that assesses aspects of sexual health in a broader sense.
The aim of the study is to develop a comprehensive EORTC questionnaire to assess sexual health of male and female cancer patients and for cancer survivors. We describe the development of the sexual health questionnaire according to the EORTC guidelines (21).
Materials and methods
According to the EORTC guidelines (21) the development of an EORTC questionnaire is typically organised in four phases. The first phases comprise a literature search following interviews with patients and health care professionals (HCPs) (phase 1) and the operationalization into items (phase 2).
Literature search and interviews
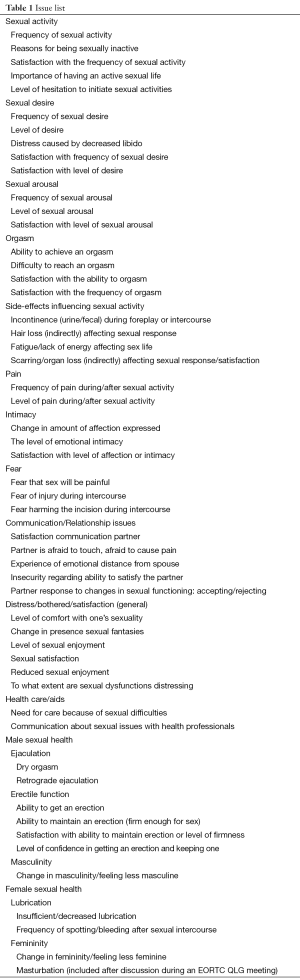
The literature search is focused on sexual health in cancer patients with a search strategy which was kept broad. The following combinations of keywords were used to identify papers in PubMed covering the period January 1993 to January 2012: ‘neoplasms[mesh]’ or ‘neoplas*[tw]’ or ‘tumor[tw]’ or ‘tumors[tw]’ or ‘tumou*[tw]’ or ‘cancer*[tw]’ or ‘carcinom*[tw]’ or ‘oncolog*[tw]’ and ‘sexuality[mesh]’ or ‘sexual function or sexual function[all fields]’ or ‘sexual function[tiab]’ or ‘sexual dysfunction’ or ‘sexual dysfunction [all fields]’ or ‘sexual dysfunction[tiab]’. Articles focusing on sexuality that conceptually exceeds issues relating to sexual function, sexual activity or sexual response cycle in cancer patients and/or cancer survivors were selected through title and abstract screening. For inclusion, original research articles had to be full reports in English and published in peer-reviewed journals. Qualitative and quantitative studies are included in the review. Additionally, an evaluation of measures related to sexuality in cancer patients was conducted (Den Oudsten et al., unpublished data). Issues which resulted from the literature search were summarized in an issue list. The same list was then presented to patients and HCPs recruited by collaborators within the EORTC Quality of Life Group for feedback on appropriateness of content and breadth of coverage on a four-point Likert scale. The following demographic data from the HCPs were asked: professional background, cancer sites they were most familiar with, duration of being involved in the care of patients with cancer, sex and country. A case report form including the most important clinical data related to disease and therapy was given to patients. The list of issues was translated into several languages. Members and collaborators of the EORTC-QLG spread out the questionnaire to other HCP specialists in oncology such as psycho-oncologists, radiotherapist or gynaecologists in more than 20 institutions in different countries (Table 1).
Full table
For the final decision which issues on sexual health are definitely important for cancer patients, mean scores for relevance and priority ratings were defined according to the EORTC-QLG guidelines (21) using the following criteria: (I) mean score for HCPs <2 versus ≥2; and (II) mean score for patients <2 versus ≥2; (III) priority should have been rated by more than 30% of the HCPs; and (IV) >30% of patients as highly relevant to be included. Issues that met three or four of these criteria were kept in the list. Issues that met less than three criteria were deleted, unless the interviews provided strong arguments for retaining them. Additional new issues were included if they were mentioned by a considerable number of patients or HCPs. Based on the remaining issues the items for the provisional questionnaire were developed.
Operationalization into items
The process of translation is formally conducted according to the EORTC QLG Translation guidelines with a rigorous forward-backward procedure (18) supported by native speakers. The underlying English issues will be operationalised into items first. If items already have been used in another validated EORTC questionnaire they normally are included in their original wording. Questions are phrased in a way that they fit into the 4-point answering format of the EORTC ranging from “not at all” to “very much”. A time frame of 4 weeks is chosen as suggested in the EORTC guidelines (21). A standardized introduction was modified for the issue of sexual health.
Phase 3 is the pilot-testing of the final item list and is actually under construction. A validation of the questionnaire will be done in phase 4.
Results
Results of the literature search
Many generic and cancer-specific sexual health issues have been identified in the literature review. A total of 4,518 articles were screened of which 3,461 articles were excluded because they did not focus on cancer patients and/or did not report sexuality as an outcome measure. Another 924 articles were excluded because they were literature reviews or presented only domain scores or were on sexual activity and sexual response cycle only. Finally, 65 articles were included in the systematic review. Apart from the frequency of sexual activity, sexual dysfunction and overall levels of satisfaction with sexual functioning, a number of issues were identified: sex-related guilt, anxiety, embarrassment, future prospects, quality of the relationship with the partner, changed feelings of sexual attractiveness, partner’s response to the changed situation, and the effectiveness and side effects of (medical) sex aids. These topics were used as underlying issues for the provisional sexual health questionnaire.
Issues concerning sexual attractiveness were restricted to quantitative studies only. Many questionnaires for measuring different aspects of sexual health were found in the reviewed literature, but cancer-specific instruments were underrepresented. Sexual functioning was often assessed as part of (health-related) quality of life. Frequencies and sexual satisfaction were commonly assessed with a single item only. Qualitative designs to assess sexual functioning were used in 20 studies. The detailed results of the literature review are described elsewhere (Den Oudsten et al., unpublished data). Issues identified by the literature search were first checked for clinical relevance. A shortened list of 53 issues was then reviewed by a great number of patients (n=107) and HCPs (n=83).
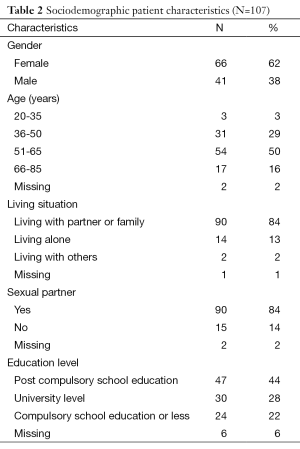
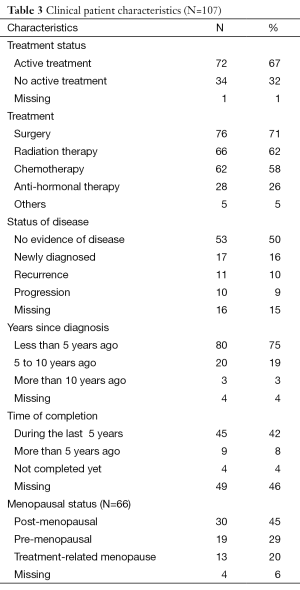
Characteristics of patients and HCPs
Most of the patients had breast cancer (n=43; 40%), followed by colorectal (n=17; 16%), and head and neck cancer (n=14; 13%). All over the group cancer sites were well-balanced. The majority of patients were treated with surgery followed by radiation therapy and chemotherapy, and were under active treatment when they were interviewed. Half of the patients had no evidence of disease (n=53; 50%); a smaller number was newly diagnosed (n=17; 16%) or had a recurrent disease (n=11; 10%). A progression was stated for 10 patients. About a half had completed their treatment within the last 5 years, 8% more than 5 years ago and the others have not completed yet or did not provide any information on that. There were more female than male patients interviewed with a mean of 55 years (±11). The majority was living with a partner or family and had a sexual partner and was well-educated (Tables 2,3).
Full table
Full table
Various experts from different disciplines, mainly employed as medical doctors (n=53; 64%), psycho-oncologists (n=16; 21%) or nurses (n=3), reviewed the issue list. Gender was equally distributed and their clinical experiences mostly ranged from 10 to 20 years. Most of the HCPs were familiar with gynecologic cancer (n=29; 26%), followed by colorectal/gastrointestinal (n=21; 19%), breast (n=18; 16%), prostate/testicular (n=9; 8%) and other cancer sites (e.g., head and neck or lung cancer) (n=33; 31%).
Interview results
Most of the issues on satisfaction as well as the importance of having an active sexual life were rated as highly important in the sexual health questionnaire by both patients and HCPs. There were several issues referring to satisfaction (e.g., satisfaction with the level of affection or intimacy, satisfaction with the frequency of sexual activity, satisfaction with the communication with the partner and sexual satisfaction). No specific issues for female patients were rated as highly important. Male patients additionally rated their level of confidence in getting an erection and keeping one as very important. These issues met all four criteria on relevance and priority. Issues on sexual arousal, orgasm-related issues and general issues on sexual enjoyment were also rather important for female and male patients and HCPs.
A very low relevance and priority had the issues on hair loss, masturbation and sexual desire (frequency, level). Also issues about fear harming the incision during intercourse, retrograde ejaculation and changes in sexual fantasies did not fulfill the criteria to be further included.
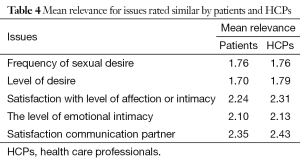
When considering the mean relevance only, all presented issues except five were more often rated as highly relevant for cancer patients by HCPs than by patients. There seems to be a similar relevance for sexual desire (frequency, level), satisfaction (with level of affection or intimacy and with the communication with the partner) and the level of emotional intimacy. All other issues were rated more relevant to be included in the questionnaire for HCPs, not for patients.
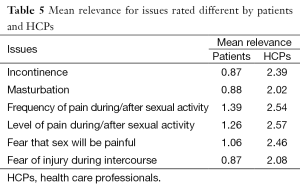
The greatest differences in the estimated relevance (>1.10) were found for issues on incontinence, masturbation, pain and fear, always rated higher by the interviewed HCPs (>1.0). Comparable results were found for issues for male sexual health (ejaculation) and issues on masculinity/femininity (Tables 4,5).
Full table
Full table
Priority for inclusion was assessed in the same way for most of the 53 issues from the list. Only level of emotional intimacy and change in amount of affection expressed was much more higher prioritised by patients than by HCPs. Although many issues on body-related changes were less relevant for patients on average, they thought that these topics should be included in such a questionnaire of sexual health for cancer patients anyway (e.g., incontinence).
Highest differences in the evaluated issues, identified for relevance and priority, were found for frequency of pain (during/after sexual activity), incontinence, fear that sex will be painful, and for communication about sexual issues with HCPs. While the interviewed HCPs found those issues more important to integrate in the sexual health questionnaire, patients found them less relevant.
Item development
On the basis of the results a provisional item list was established (“EORTC SHQ-Cxx”), supported by the translation coordinator of the EORTC Quality of Life Department. Issues fulfilling all four criteria on relevance and priority were automatically included. Issues within the categories of sexual desire, sexual arousal and pain were combined each. Issues implying norms, such as frequencies or content-related redundancy were not included. Negative wording or ambiguity was additional reasons for exclusion. The reduced list of 22 items with an additional question on reasons for not being sexually active was reviewed by two independent native English speakers before starting the translations process. At least three languages representing an English-speaking country, a country from Northern and Southern Europe were invited for preparation of pilot-testing, which is the next step in the EORTC procedure to develop a validated EORTC questionnaire.
Discussion
The results of the literature search were considered for the development of the issue list which was presented to patients and HCPs. Interview results were then analysed and item development process was done before continuing with pretesting.
Studies on sexuality in oncology patients which were found in the literature search predominantly focused on issues of activity, experiences of sexual dysfunction, and satisfaction with sexual functioning. The literature review identified themes beyond these aspects and provided interesting results on current instruments used for measuring sexual health. No questionnaire currently exists that focuses on physical, psychological, and social aspects of sexuality for cancer survivors. Based on the available interview results most important issues to fill this gap were identified: satisfaction and the importance of having an active sexual life such as the level of confidence in getting an erection and keeping one for male patients. Different evaluations by HCPs and patients were found for most of the issues. Pain, incontinence, fear and communication about sexual issues with HCPs were issues which were highly relevant for HCPs but not for patients. Less research exists, in which possible reasons have been identified. Body image can change during different phases of cancer treatment. As shown in a review article by Cororve Gingeret et al. 2014 (22) patients are found to be most concerned about body image in the immediate postoperative period and soon after completing other forms of treatment (23). In a study with 225 Canadian cancer patients, 44% used the Internet to learn more about their condition and 14% wished their medical teams had provided them with links, but did not independently search for medically relevant information about their condition. While education level was correlated with web based information seeking, age was not (24). Why fear as an issue was less important for our interviewed patients than for professionals would be interesting to further investigate.
Strength of the study is the fact that the development of the sexual health questionnaire is based on current literature, patient and HCP interviews from many different countries according to the EORTC guidelines (21). The literature review systematically examined sexual health issues in cancer beyond general ratings of sexual activity, symptoms, and sexual dysfunction. As other literature reviews (25-28) have described patients’ sexual activities, types of sexual dysfunction and generic levels of sexual satisfaction, this review uniquely took as its focus sexual health issues for all cancer patients and survivors. Including interviews of more than 100 patients with different cancer sites and many professionals from different disciplines also increases the quality of the development process. The provisional module will then be pre-tested in various languages to identify and solve potential problems with wording. For pilot-testing patients from many different countries and cultures are foreseen (phase 3) after the translation process was finished and ethical approval was done. Also the translations into several languages and the cross cultural distributions for developing the questions follow a standardized procedure (18). The questions are designed for male and female patients with different cancer sites during all stages of their disease.
It is suggested that future studies broaden their focus to encompass sexual health related topics (body image, self-esteem, relationship functioning and communication) rated as important in cancer survivors which is not evident yet. But these issues should be addressed in clinical trials to get information on a possible impact for clinical practice. The instrument will be designed as a ‘stand-alone’ sexual health measure that can be used in clinical trials as well as in clinical studies. The results of trials which use the sexual health questionnaire adequately can improve sexual health care.
Acknowledgements
We thank all patients and collaborators who were taking part in the whole development process.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethical committee (ID: EK 25-273 ex 12/13) and patient consent was obtained.
References
- Schover LR, Montague DK, Lakin MM. Sexual problems. In: DeVita VT Jr, Hellman S, Rosenberg SA. eds. Cancer: Principles and Practice of Oncology. 5th ed. Philadelphia, PA: Lippincott-Raven Publishers, 1997:2857-72.
- Broeckel JA, Thors CL, Jacobsen PB, et al. Sexual functioning in long-term breast cancer survivors treated with adjuvant chemotherapy. Breast Cancer Res Treat 2002;75:241-8. [PubMed]
- Fosså SD, Woehre H, Kurth KH, et al. Influence of urological morbidity on quality of life in patients with prostate cancer. Eur Urol 1997;31:3-8. [PubMed]
- Ganz PA, Rowland JH, Desmond K, et al. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol 1998;16:501-14. [PubMed]
- Smith DS, Carvalhal GF, Schneider K, et al. Quality-of-life outcomes for men with prostate carcinoma detected by screening. Cancer 2000;88:1454-63. [PubMed]
- Frumovitz M, Sun CC, Schover LR, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol 2005;23:7428-36. [PubMed]
- Greimel ER, Winter R, Kapp KS, Haas J. Quality of life and sexual functioning after cervical cancer treatment: a long-term follow-up study. Psychooncology 2009;18:476-82. [PubMed]
- McClelland SI. Measuring sexual quality of life: Ten recommendations for health psychologists. In: Baum A, Revenson TA, Singer J. eds. Handbook of Health Psychology. New York: Taylor & Francis, 2012;247-69.
- National Institutes of Health. The prevalence and types of sexual dysfunction in people with cancer 2013 [cited 2014 June 6]. Available online: http://www.cancer.gov/cancertopics/pdq/supportivecare/sexuality/HealthProfessional/page1
- Andersen BL. Quality of life for women with gynecologic cancer. Curr Opin Obstet Gynecol 1995;7:69-76. [PubMed]
- Arai Y, Kawakita M, Okada Y, et al. Sexuality and fertility in long-term survivors of testicular cancer. J Clin Oncol 1997;15:1444-8. [PubMed]
- Derogatis LR, Kourlesis SM. An approach to evaluation of sexual problems in the cancer patient. CA Cancer J Clin 1981;31:46-50. [PubMed]
- Ganz PA, Desmond KA, Leedham B, et al. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst 2002;94:39-49. [PubMed]
- Masters WH. The sexual response cycle of the huma female. I. Gross anatomic considerations. West J Surg Obstet Gynecol 1960;68:57-72. [PubMed]
- Masters WH, Johnson VE. The human female: anatomy of sexual response. Minn Med 1960;43:31-6. [PubMed]
- WHO. Sexual health - a new focus for WHO. Progress in Reproductive health Research. Progress No 67, 2004.
- Burnett AL, Aus G, Canby-Hagino ED, et al. Erectile function outcome reporting after clinically localized prostate cancer treatment. J Urol 2007;178:597-601. [PubMed]
- Koller M, Aaronson NK, Blazeby J, et al. Translation procedures for standardised quality of life questionnaires: The European Organisation for Research and Treatment of Cancer (EORTC) approach. Eur J Cancer 2007;43:1810-20. [PubMed]
- Jeffery DD, Tzeng JP, Keefe FJ, et al. Initial report of the cancer Patient-Reported Outcomes Measurement Information System (PROMIS) sexual function committee: review of sexual function measures and domains used in oncology. Cancer 2009;115:1142-53. [PubMed]
- Flynn KE, Lin L, Cyranowski JM, et al. Development of the NIH PROMIS ® Sexual Function and Satisfaction measures in patients with cancer. J Sex Med 2013;10 Suppl 1:43-52. [PubMed]
- Johnson C, Aaronson N, Blazeby JM, et al. EORTC Quality of Life Group: guidelines for developing questionnaire modules. 4th edition. Brussels: EORTC Publications, 2011.
- Cororve Gingeret M, Teo I, Epner DE. Managing body image difficulties of adult cancer patients. Cancer 2014;120:633-41. [PubMed]
- Fobair P, Stewart SL, Chang S, et al. Body image and sexual problems in young women with breast cancer. Psychooncology 2006;15:579-94. [PubMed]
- Katz JE, Roberge D, Coulombe G. The cancer patient’s use and appreciation of the internet and other modern means of communication. Technol Cancer Res Treat 2014;13:477-84. [PubMed]
- Abbott-Anderson K, Kwekkeboom KL. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol Oncol 2012;124:477-89. [PubMed]
- Matthew AG, Goldman A, Trachtenberg J, et al. Sexual dysfunction after radical prostatectomy: prevalence, treatments, restricted use of treatments and distress. J Urol 2005;174:2105-10. [PubMed]
- Neises M. Sexuality and sexual dysfunction in gynecological psychooncology. Onkologie 2002;25:571-4. [PubMed]
- Flynn KE, Lin L, Cyranowski JM, et al. Development of the NIH PROMIS ® Sexual Function and Satisfaction measures in patients with cancer. J Sex Med 2013;10:43-52. [PubMed]


