Varicocele and its effect on testosterone: implications for the adolescent
Introduction
The treatment of adolescent varicoceles is controversial and emotional. What parent wants to risk future infertility of their son through inaction? The fear of a progressive disease process weighs heavily on the minds of the parents and the patient. Every year the young boy embarrassingly sees a doctor because he has an abnormality of one of his male organs. Yet, the consequences of inaction are not clear. Indeed, the exact deleterious effects of varicocele on testicular function are unclear.
To date there are many unanswered questions despite over a hundred years of debate. What is the exact pathophysiology? Why are some patients affected and others not? What causes the pain? Why are some men infertile with small varicoceles and others with huge varicoceles fertile? Does the size matter? How can a unilateral varicocele cause bilateral dysfunction? How should a varicocele be determined, by physical exam or ultrasound? What is the best way to perform the ultrasound? Do varicoceles cause atrophy? What is the best way to measure atrophy? Does repair reverse the atrophy? What is the best way to measure future infertility; a semen analysis, a testicular volume, varicocele size, or testicular size discrepancy? How do the adult data relate to the pediatric population? All these questions are important yet most remain unanswered.
Whereas in the infertile male a semen analysis is easily obtained with well-established norms, the same cannot be said of the adolescent. Fertility potential is not easily measured in the adult let alone the adolescent; as a result ipsilateral testicular hypotrophy/atrophy is commonly used as a surrogate indication. Other indications for intervention include testicular pain or embarrassing fullness or swelling. In the adult the main indications for intervention are infertility and abnormal semen analysis, both unavailable in most teens. Varicoceles have been linked to hypogonadism in the adult male. Yet a hormonal profile has not been considered standard in the assessment of the adolescent varicocele. The purpose of this review is to examine the association of varicoceles and hypogonadism and the potential benefit of repair of adolescent varicoceles on the hypogonadism.
Historical information
The varicocele and its association with testicular damage, “in as much as its (the testicle’s) nutrition was defective,” was described by Celsus in 24 AD (1). The correction of varicoceles has been reported in the scientific literature for over 100 years (2-5). The potential impact of the varicocele on fertility was first described by Hotchkiss in 1944. Tulloch reported his results of high inguinal varicocele ligation on 30 men (5 bilateral), describing normalization of sperm counts and pregnancy in two azoospermic men and improvement in sperm counts in 87% of the group overall (6). As controversial as treatment in adults has turned out to be, historically, this has been even more of a problem in teens. As early as 1944, Hotchkiss suggested that earlier repair might be important but was uncertain about the indications:
“the surgical correction of a varicocele is probably only effective as a prophylactic measure against damage which might ensue with passing years. It is unlikely that the operation has other than cosmetic value in long-standing cases with small soft testes”.
Indications for surgery
Varicoceles are common. In a large 1995 large observational series of 9,034 men presenting for infertility, varicoceles were found in 25.4% of men with abnormal semen, compared with 11.7% of men with normal semen. Infertile men with varicoceles were found to have decreased testicular volume, impaired sperm quality, and decline of Leydig cell secretion. Despite these findings in this infertile population, spontaneous pregnancy rates were identical in men with or without varicoceles (7). A Cochrane review of controlled series also demonstrated only slight benefit from adult varicocele repair (8).
According to 2008 ASRM guidelines, the indications for surgical intervention in the infertile adult male include a varicocele that is palpable on physical examination of the scrotum, known infertility, “normal” female fertility, and abnormal semen parameters or sperm function tests. The repair of varicoceles considered “subclinical” or in men with normal seminal parameters was not recommended.
In a recent survey of 131 pediatric urologists, varicocelectomy was most commonly performed for decreased ipsilateral testicular size (96%), testicular pain (79%), and altered semen analysis parameters (39%) with only 4% considering androgen status in their decision to treat (9). In a recent meta-analysis, varicoceles in youth appeared to negatively affect sperm density, motility, and morphology and treatment appeared to result in moderate improvement of sperm density and mild improvement in sperm motility but again androgen status was not mentioned (10). Few pediatric studies on varicoceles evaluate androgen status although early studies suggest that as many as 30% of adolescents with unilateral varicoceles may have an abnormal testicular response to exogenously administered gonadotropic releasing hormone (11).
Incidence of varicoceles and hypotrophy/atrophy in adolescents
Varicoceles appear during adolescence as the testes enlarge and usually present as scrotal swelling and rarely pain (12-14). In a prospective study of 1,072 Danish boys, Oster reported a 16.2% incidence of varicoceles in boys aged 10-19 years of age (15). Varicoceles are associated with hypotrophy/atrophy in many studies. In one series of 30 symptomatic boys average age 14.4, 77% demonstrated ipsilateral hypotrophy and the author recommended surgical correction (16). Hypotrophy/atrophy is, as noted above, an indication for surgery and there are many series reporting “catch-up growth” after successful repair. In a non-randomized surgical series of 40 pubertal boys, mean age 14.5, with grade 2 and 3 varicoceles, 24 underwent surgery and 16 were observed (by the choice of the parents). The surgical group demonstrated more testicular atrophy at baseline (68% vs. 50%). Of the 16 corrected boys with pre-operative atrophy 56% resolved their atrophy vs. none in the observational group. In those tested, all seminal parameters (concentration, motility and morphology) showed statistically significant improvement in the surgical vs. the observed group. Furthermore, whereas 5/16 boys that were observed without atrophy at presentation developed atrophy, none in the surgical group developed atrophy. Sperm concentrations almost doubled in the treatment group (51 vs. 26 million/mL).
Normal testosterone levels in children
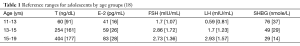
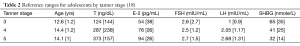
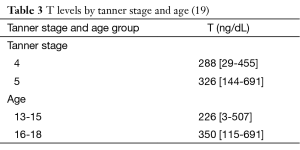
Male fertility is dependent on spermatogenesis and T is crucial in maintenance of spermatogenesis. The reader is encouraged to read a recent comprehensive review on the role of androgens on spermatogenesis (17). Despite the importance of T in fertility, there is a paucity of publications on the impact of varicoceles on the T production in children or adolescents. Normal reference ranges of T and other fertility hormones for children and adolescents are subject to the variability of the pituitary—gonadal axis in the prepubertal and pubertal male. T levels increase in the first 6 months of life in male infants as a response to pituitary stimulation. T then remains low for children until puberty when the T concentration in boys starts to increase. In 2013, Konforte prospectively examined sex hormones in a healthy cohort of children from birth to age 18, as part of the CALIPER study (Canadian Library Initiative for Pediatric Reference Ranges). The intent was to stratify normal reference ranges of all fertility hormones (T, E2, FSH, LH, SHBG, Prolactin), by age and Tanner groups for both males and females. The data provided in the appendix allow an extrapolation of mean values of sex hormone values by age groups and “self-reported” Tanner stages (Tables 1,2). Only 23% and 58% of Tanner 4 and 5 and only 30% and 60% of boys 13 to 5 and 15 to 19 respectively would be considered eugonadal by adult endocrine guidelines (T >350 ng/dL) (18). In a smaller study on discarded blood samples in children undergoing elective non-endocrine related surgery, Kulle derived similar hormone levels in Tanner 4 and 5 adolescents and ages 13 to 18 (Table 3) (19). These baseline values are all what would be considered the lower range of normal for adults and as a baseline, these normal values for adolescents give pause to the concept of measuring the androgen axis in teens with varicocele. In one study of teens with varicocele, T levels at presentation were on the low side (less than 300 ng/dL) but were unfortunately not measured post- operatively (20). Indeed, there are no prospective studies examining T levels in pubertal boys before and after varicocele repair.
Experimental evidence linking hypogonadism to varicoceles
Venous backflow with elevation of testicular temperature, increased spermatic vein pressure, accumulation of adrenal waste products and autoimmunity have been hypothesized to create a toxic environment to both Sertoli and Leydig cells (21). In the rat, ram, monkey, and man, the presence of a varicocele results in an increase in the intra-testicular temperature and hydrostatic pressure of both testes (22-25).
In an elegant investigation on the effect of experimentally induced varicoceles in adult Sprague Dawley rats, Rajfer et al. demonstrated the detrimental effect of a unilaterally induced varicocele on intratesticular T and the inhibition of two of the enzymes responsible for the production of T, 17,20-desmolase and 17 α-hydroxylase. Interestingly, despite the the fact that the experimental procedure was unilateral, the enzymatic activity and intratesticular T levels were reduced in both testes (26).
Human studies have shown that increased testicular temperature is closely associated with increased Leydig cell apoptosis (21), increased cytoplasmic vacuolization and Leydig cell atrophy (27).
Does varicocele repair increase T levels?
Hypogonadism may very well impact the adolescent, both during and well beyond his procreative years. Some of the potential complications of hypogonadism include metabolic syndrome, sexual dysfunction, reductions in bone mineral density and reduced overall well-being. Although no data are available on T levels before and after varicocele repair in adolescents, there are studies of this in adults. In 1995 Schlegel published a retrospective analysis of pre-operative and post-operative T measurements in 53 men with clinical varicoceles undergoing repair. A statistically significant increase in T levels was seen as early as one month from the repair, mean values increasing from 319 to 409 ng/dL. Sixty-six percent of the men had grade I-II varicoceles and counter-intuitively, the biggest changes in T were seen in the men with the lower grades of varicocele. Although, pre-operative T levels were not affected by the grade of the varicocele, the post-op increase in T was inversely related to the starting T. Yet not all men with subnormal T levels improved after repair. Six of 18 men (33%) with pre-operative subnormal T levels decreased after the repair (28).
In 2011, Goldstein published a series of 110 infertile men with clinical varicoceles in whom pre- and post-operative T measurements were available. Mean follow-up was 10 months. When patients were stratified by pre-operative T of less than or more than 400 ng/dL, without stratification by age, men with the lower T had significant increases (mean 309 to 431 ng/dL, P<0.001) while those higher baseline T trended to a lower level (498 to 463, P<0.29). Overall, 60% of men had improvement in their T and total motile sperm count regardless of their starting T level (29).
Not all studies have shown the improvement seen in the previous two studies. In a recent meta-analysis of 125 current published trials, only nine were felt to be acceptable for review. Though T levels increased post-operatively in all, only three trials showed a statistically significant increase. Taken all these studies together, the authors concluded that serum T was significantly higher than pre-operative levels after varicocele repair. Overall, the mean increase in T was 98 ng/dL. A prospective randomized trial is clearly needed to answer the question fully.
Conclusions
The surgical treatment of the adolescent varicocele is controversial and debated. The indications for surgery have been primarily testicular hypotrophy/atrophy but also include varicocele size, pain and abnormal semen analyses (if old enough). The recent adult literature suggests that hypogonadism may also be an indication for repair in adults and it seems that this should be studied in adolescents. Consideration should be given to measuring T levels in adolescents with a varicocele. Prospective, long term, randomized trials are needed to help elucidate the benefit of varicocele repair on hypogonadal adolescent males.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Celsus AC. Cornelius Celsus. Venezia, Philippus Pencius f[UNKNOWN ENTITY &udie;]r Benedictus Fontana, 1497.
- Duncan J. Clinical Observations on the Subcutaneous Ligature of Varix and Varicocele. Br Med J 1881;2:37-8. [PubMed]
- Ogston A. II. The Operation for Varicocele. Ann Surg 1886;4:120-3. [PubMed]
- Robson AW. Treatment of Varicocele by Excision. Br Med J 1886;1:389-90. [PubMed]
- Keetley CB. The Cure of Varicocele. Ann Surg 1888;8:205-7. [PubMed]
- Tulloch WS. Varicocele in subfertility; results of treatment. Br Med J 1955;2:356-8. [PubMed]
- The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. World Health Organization. Fertil Steril 1992;57:1289-93. [PubMed]
- Kroese AC, de Lange NM, Collins J, et al. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev 2012;10:CD000479. [PubMed]
- Pastuszak AW, Kumar V, Shah A, et al. Diagnostic and management approaches to pediatric and adolescent varicocele: a survey of pediatric urologists. Urology 2014;84:450-5. [PubMed]
- Nork JJ, Berger JH, Crain DS, et al. Youth varicocele and varicocele treatment: a meta-analysis of semen outcomes. Fertil Steril 2014;102:381-387.e6.
- Kass EJ, Freitas JE, Salisz JA, et al. Pituitary gonadal dysfunction in adolescents with varicocele. Urology 1993;42:179-81. [PubMed]
- Verstoppen GR, Steeno OP. Varicocele and the pathogenesis of the associated subfertility a review of the various theories. II: Results of surgery. Andrologia 1977;9:293-305. [PubMed]
- Verstoppen GR, Steeno OP. Varicocele and the pathogenesis of the associated subfertility. A review of the various theories. I: Varicocelogenesis. Andrologia 1977;9:133-40. [PubMed]
- Verstoppen GR, Steeno OP. Varicocele and the pathogenesis of the associated subfertility. A review of the various theories. III: Theories concerning the deleterious effects of varicocele on fertility. Andrologia 1978;10:85-102. [PubMed]
- Oster J. Varicocele in children and adolescents. An investigation of the incidence among Danish school children. Scand J Urol Nephrol 1971;5:27-32. [PubMed]
- Lyon RP, Marshall S, Scott MP. Varicocele in childhood and adolescence: implication in adulthood infertility? Urology 1982;19:641-4. [PubMed]
- Smith LB, Walker WH. The regulation of spermatogenesis by androgens. Semin Cell Dev Biol 2014;30:2-13. [PubMed]
- Konforte D, Shea JL, Kyriakopoulou L, et al. Complex biological pattern of fertility hormones in children and adolescents: a study of healthy children from the CALIPER cohort and establishment of pediatric reference intervals. Clin Chem 2013;59:1215-27. [PubMed]
- Kulle AE, Riepe FG, Melchior D, et al. A novel ultrapressure liquid chromatography tandem mass spectrometry method for the simultaneous determination of androstenedione, testosterone, and dihydrotestosterone in pediatric blood samples: age- and sex-specific reference data. J Clin Endocrinol Metab 2010;95:2399-409. [PubMed]
- Okuyama A, Nakamura M, Namiki M, et al. Surgical repair of varicocele at puberty: preventive treatment for fertility improvement. J Urol 1988;139:562-4. [PubMed]
- Shiraishi K, Takihara H, Matsuyama H. Elevated scrotal temperature, but not varicocele grade, reflects testicular oxidative stress-mediated apoptosis. World J Urol 2010;28:359-64. [PubMed]
- Gomes WR, Butler WR, Johnson AD. Effect of elevated ambient temperature on testis and blood levels and in vitro biosynthesis of testosterone in the ram. J Anim Sci 1971;33:804-7. [PubMed]
- Green KF, Turner TT, Howards SS. Varicocele: reversal of the testicular blood flow and temperature effects by varicocele repair. J Urol 1984;131:1208-11. [PubMed]
- Fussell EN, Lewis RW, Roberts JA, et al. Early ultrastructural findings in experimentally produced varicocele in the monkey testis. J Androl 1981;2:111-19.
- Harrison RM, Lewis RW, Roberts JA. Testicular blood flow and fluid dynamics in monkeys with surgically induced varicoceles. J Androl 1983;4:256-60. [PubMed]
- Rajfer J, Turner TT, Rivera F, et al. Inhibition of testicular testosterone biosynthesis following experimental varicocele in rats. Biol Reprod 1987;36:933-7. [PubMed]
- Sirvent JJ, Bernat R, Navarro MA, et al. Leydig cell in idiopathic varicocele. Eur Urol 1990;17:257-61. [PubMed]
- Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol 1995;154:1752-5. [PubMed]
- Hsiao W, Rosoff JS, Pale JR, et al. Older age is associated with similar improvements in semen parameters and testosterone after subinguinal microsurgical varicocelectomy. J Urol 2011;185:620-5. [PubMed]