Cystine nephrolithiasis
Introduction
Cystinuria is a hereditary, heterogeneous disorder affecting the proximal tubule’s cystine and dibasic amino acid transporter. It is one of the first inborn errors of metabolism recognized by Sir Archibald Garrod in 1908 (1). In contrast to the normal, near-complete reabsorption of cystine and the dibasic amino acids ornithine, arginine and lysine, (mnemonic: COAL), these amino acids are not reabsorbed and reach high concentrations in the urine of affected individuals. Only the abnormal excretion of cystine causes a clinical problem as it has low solubility in acidic and neutral urine and may lead to the formation of cystine crystals and stones in the urinary tract. Urinary stones may result clinically in hematuria, urinary obstruction and renal failure. Loss of ornithine, arginine and lysine does not cause any known phenotypic traits. Although cystinuria is one of the classic inborn errors of metabolism and has been described in several species, the disease is phenotypically heterogeneous, and its molecular basis is only imperfectly understood.
Physiology and pathophysiology of cystine transport
The luminal cystine transporter functions as an exchanger, transporting cystine and cationic amino acids (0, +) along their electrochemical gradient into the proximal tubular epithelial cells in exchange for intracellular neutral amino acids, in a Na+-independent manner (2). The cystine transporter, one of the heteromeric amino acid transporters (HATs), is a heterodimer of the heavy subunit known as rBAT, a type II membrane N-glycoprotein encoded by SLC3A1, and the eukaryotic light subunit b0,+AT, a highly hydrophobic molecule encoded by SLC7A9 (3). The two proteins are joined by a disulfide link. The co-expression of both subunits b0,+AT and rBAT is essential for the functional expression of the whole system, named b0,+, in the apical plasma membrane. The heavy subunit is needed to localize the transporter to the apical membrane, while the light subunit comprises the catalytic, transporting component (4).
Genetics of cystinuria
Two genes have been implicated in cystinuria: SLC3A1 which contains 10 exons and encodes rBAT (5) and SLC7A9 which contains 13 exons and encodes b0,+AT (6). In large screening studies, more than 130 pathogenic variants in SLC3A1 and nearly 100 mutations in SLC7A9 have been reported. The observed variants cover the whole spectrum of mutations, ranging from nonsense, missense, splicing, and frame shift mutations to whole- and multi-exon imbalances. Mutations in SLC3A1 are associated with an autosomal recessive mode of inheritance, whereas SLC7A9 variants result in an incomplete dominant inheritance, meaning that a heterozygous patient is occasionally affected by stone disease (7). However, most patients have two mutated alleles. It is also possible that the stone-forming tendency of patients with cystinuria has a genetic component beyond mutation in both of the known genes and may include other yet-unidentified modifier genes.
Classification
In the past, cystinuria was divided into three subtypes according to the amount of cystine excreted by the obligate heterozygous parents of the affected children (phenotypic classification). The parents of type I patients excreted normal amounts of cystine, while the heterozygous parents of types II and III (non-type I) had abnormal excretion of cystine, indicating that the disease is transmitted in a dominant mode with incomplete penetrance (8).
In the International Cystinuria Consortium (ICC), which included patients from Europe and Israel, it was recognized that there was a poor genotype-phenotype correlation. Although type I was largely caused by mutations in SLC3A1, a small proportion of these patients had two mutated SLC7A9 alleles (9). In contrast almost all cases of non-type I cystinuria were caused by mutations in SLC7A9, with the exception of a few cases with a complex, in-frame duplication of SLC3A1. Cases previously termed types II and III based on clinical testing were genetically indistinguishable. The result was a new classification, currently in use, based on genetic data. Type A is due to mutations in both alleles SLC3A1 (genotype AA) and type B disease is due to mutations in both alleles SLC7A9 (genotype BB) (10). Rare cases of digenic inheritance (type AB) have also been described, but individuals with this pattern do not produce stones. Other digenic stone formers were shown to have ABB or AAB patterns. Considering that in many studies the detection rates for mutations in SLC3A1 or SLC7A9 do not reach 100%, and due to the complex nature of renal amino acid transport, the role of further genes and modifying factors in the etiology of cystinuria has been postulated.
In clinical practice, genotyping of affected patients is not currently necessary as it scarcely influences the prognosis and therapy of the disease. While about 94% of people homozygous for SLC3A1 or SLC7A9 mutations will develop kidney stones in their lives, the age of onset of kidney stone formation is difficult to predict and shows a broad intrafamilial variability (9). The urinary excretion pattern in heterozygote SLC7A9 mutation carriers is variable and does not allow prediction of the clinical course; most will not have stones. The majority of SLC3A1 heterozygotes do not exhibit an abnormal amino aciduria phenotype (11).
Prevalence, clincal features and presentation
The prevalence of cystinuria has been estimated to vary from 1:2,500 in a Libyan-Jewish population to 1:100,000 in Swedes (12). Screening tests for cystinuria in Japan identified 6 patients among 110,000 students. None of these showed stone formation after 7 years of follow-up (13). The relative rarity of this condition accounts for the paucity of data involving large series.
The median age of onset of stones was 12 years in a cohort of over 200 patients (14). For unclear reasons, males appear to be more severely affected than females. Substantial variability existed in the age of onset of stones, as 40% of patients had their first stone between 11 and 20 years, while 14% of females, and 28% of males formed calculi before the age of 3 (15). In a database of 224 patients from 150 families there were no clinical differences in urinary amino acid excretion patterns between cystinuria type A and B (10). Stone formation did not correlate with amino acid urinary excretion, suggesting the importance of other modifiers of stone formation such as fluid intake, diet and modifier genes.
Like non-cystine stone formers, cystinuria presents with symptoms related to stone formation, such as renal colic and hematuria. However, people with cystinuria were almost 5 times as likely to have undergone a nephrectomy, sometimes presenting with a non-functioning kidney containing a large staghorn calculus (16). Cystinuria is associated with reduced glomerular filtration rates (GFR). In the ICC data, GFR was reduced in 17% of those patients. Factors which might contribute to reduce GFR include the need for multiple urological procedures such as extracorporeal shock-wave lithotripsy, intranephronal crystal formation and repeated episodes of urinary tract obstruction.
Diagnosis
Cystinuria is diagnosed among patients with nephrolithiasis and one or more of the following findings:
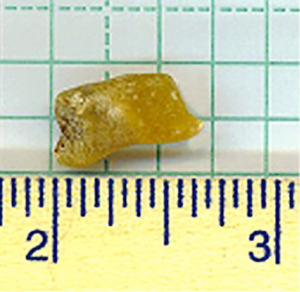
- Stone analysis showing cystine (Figure 1 depicts a large, typical, yellow cystine stone passed spontaneously);
- Positive family history of cystinuria;
- Positive laboratory screening of urine with sodium nitroprusside;
- Identification of pathognomonic hexagonal cystine crystals on urinalysis (seen on initial urinalysis in about 25% of patients);
- Cystinuria should also be suspected in patients with large branched (staghorn) calculi, filling the collecting system and requiring surgical management.
Laboratory studies
Quantitative testing of urinary cystine excretion should follow the diagnosis of cystinuria. Sodium nitroprusside detects more than 75 mg/L, while normal cystine excretion is 30 mg/day (0.13 mmol/day). Patients with cystinuria generally excrete more than 400 mg/day (1.7 mmol/day). However, the accuracy of cystine testing by most labs is imperfect. Among the problems is that these tests depend on cystine solubility, and can under certain circumstances lead to misleading results. Cystine is relatively insoluble at urine pH below 6.5, remaining in non-measurable, crystalline form. The result is artifactually low values if urine samples are not alkalinized after voiding before measurement of cystine (17). Another problem is that cystine assays do not distinguish cystine from soluble thiol drug-cysteine complexes. In patients taking tiopronin or d-penicillamine, thiol-cysteine bonds can be broken by sample preparation, releasing cysteine which recombines with itself to form the insoluble dimer cystine. The result is inaccurate measurement in patients taking thiol drugs and inability to judge drug efficacy.
These problems led to the development of a solid-phase assay which is reliable in the presence of thiol drugs (18). Cystine crystals are added to a patient’s urine and after incubation for 48 h, the remaining crystals are collected. In supersaturated urine, cystine precipitates onto the added crystals, so the solid phase grows and is greater than that which was added; the urine is said to have a ‘negative cystine capacity’. If urine is undersaturated, it can dissolve the added cystine crystals; such urine has a ‘positive cystine capacity’ (19). Whether the assay predicts stone-forming activity has not yet been established but is a topic of study by the Rare Kidney Stone Consortium (20).
Pathology
Biopsies of renal papillae have been performed on well characterized cystine stone formers (21). Histopathological findings varied from normal in some participants, to plugging, dilatation and injury of ducts of Bellini. Inner medullary collecting ducts were also affected. The large plugs of crystals in ducts of Bellini were always composed of cystine, whereas in the inner medulla and thin loop of Henle, deposits were invariably composed of calcium phosphate in the form of hydroxyapatite. Whether treatment with potassium citrate for urinary alkalinization was responsible for these hydroxyapatite precipitates is not clear. An alternative explanation is that these crystals are the result of the relatively alkaline urine pH often observed in patients with cystinuria.
Renal stone disease is often considered to be a mechanical problem with nephronal obstruction by cystine crystals the primary driver of renal injury. This microscopic obstruction could cause upstream cell injury and interstitial reaction, glomerular loss, and cortical fibrosis. However, crystal nephropathies have recently been recognized to cause significant intra-renal inflammation that can cause acute kidney injury (22). For example, inflammation and tissue remodeling have been seen as the result of calcium oxalate crystals. Activation of the NLRP3 inflammasome leads to secretion of the pro-inflammatory cytokine IL-1β (23). Whether cystine is capable of stimulating these inflammatory pathways has not yet been determined.
Management
Treatment is focused on reducing the absolute amount of cystine in the urine and increasing the solubility of cystine. Initial conservative measures should be attempted in all patients focusing on decreasing cystine concentration and supersaturation by increasing fluid intake and pH; and decreasing the cystine excretion and production by limiting sodium and protein intake. If these measures fail, cystine-binding thiol drugs are considered (24).
Increasing oral fluid intake
Increasing oral fluid intake to increase urine volume is an essential measure for all types of nephrolithiasis, including cystinuria. The goal is to reduce urine cystine supersaturation to less than 1.0 at a urine pH above 7.0. Patients with cystinuria often need to drink 3-4 L per day to achieve a urine cystine concentration of less than 243 mg/L (1 mmol/L) and thus decrease the concentration of urinary cystine below the level of saturation (19). Fluid intake throughout the day, at night, and augmented with higher ambient temperatures or exercise, should all be stressed. Given the barriers to achieve such a high fluid intake, especially the subsequent need to void frequently, prescription of an antidiuretic hormone (ADH) antagonist was proposed (25). In these two reported cases, tolvaptan 15 mg once daily was used for 5 days. By provoking thirst, urine dilution was achieved with no significant side effects. However the drug is extremely costly and currently has a black box warning associated with it due to hepatotoxicity seen in treatment of polycystic kidney disease (26). We do not consider prescription of vasopressin antagonists a reasonable method of increasing urine volume.
Urinary alkalinization
Cystine solubility increases with increasing pH, best achieved with oral administration of potassium citrate (27). A starting dose of 20 meq twice daily might or might not be sufficient with increases based on periodic pH testing. Hyperkalemia is unusual unless GFR is reduced. Taking the supplements after meals reduces the risk of dyspepsia. Potassium bicarbonate might have fewer adverse gastric effects for some patients. Sodium citrate or sodium bicarbonate may also be appropriate but are second line choices as increased urinary sodium excretion leads to increased cystine excretion.
Although acetazolamide has been recommended to increase urinary pH, it was not shown to be superior to citrate and the associated metabolic acidosis with presumed risk to bone mineral density make it less than an ideal method to raise urine pH (28).
Dietary manipulation
Although the tubular reabsorption of cystine in the proximal tubule occurs via a sodium-independent transporter, cystine excretion can be reduced by decreasing dietary sodium (19,29). The physiology of this effect is not known. We therefore recommend restricting salt intake to about 2 g per day. Reduction of animal protein intake to 1 g/kg body weight may be useful as well for two reasons. First, reduction of intake of cystine and its precursor methionine is associated with reduction in cystine excretion (30). In addition, as animal protein is an important source of protons in the Western diet, reducing protein intake leads to an increase in urine pH and should lead to a reduction in the amount of citrate required to achieve urinary alkalinization to pH greater than 7 (31). Despite the evidence that protein and salt restriction lead to less cystine excretion, there are no long-term studies demonstrating that these prescriptions reduce formation of cystine stones.
Cystine-binding thiol drugs
In patients who are refractory to increased fluid intake, urinary alkalinization and dietary restriction of protein and salt, CBTDs are recommended. The two in use currently are D-penicillamine and alpha-mercaptopropionylglycine, or tiopronin. These drugs work by reducing the disulfide bond of cystine, producing mixed disulfides with cysteine that are more soluble than cystine. The solubility of the cysteine-penicillamine complex, for example, is 50-fold higher than of cystine (32).
The incidence of adverse effects such as allergy is slightly lower with tiopronin, making it our usual first-line agent. D-penicillamine is reserved for people with adverse events related to tiopronin and for those who have taken it for a long time without problems. Adverse events can be limited if one starts with low doses. Monitoring of liver enzymes, complete blood count, and urinary protein excretion should be performed at 4-6-month intervals. The angiotensin converting enzyme inhibitor captopril also contains a thiol group and can increase solubility of cystine in vitro. However urinary excretion of captopril may not be adequate to cause meaningful changes in cystine solubility (19). A recent in vitro study found that increasing urine pH was associated with increased thiol drug efficacy in a clinically relevant time frame (33). Using CBTDs without alkali would not be recommended based on this non-clinical study.
Prospects for new drugs
Atomic force microscopy (AFM) is a technique that allows study of crystal growth. Computer modeling led to selection of molecules that are candidates for inhibition of cystine crystallization, with AFM used to confirm (34). Cystine crystal growth was significantly inhibited at low concentrations by L-cystine dimethylester (CDME), a structural analog of cystine that probably provides steric inhibition of cystine crystal growth. We extended this work by demonstrating that CDME can be given to knock-out mice with cystinuria and effectively limits cystine stone formation (35). Toxicity was not apparent. Despite the encouraging findings, toxicity remains of concern as CDME has been used to produce an animal model of cystinosis, a disorder in which intracellular lysosomal cystine accumulation occurs (36).
Another promising strategy for the treatment of cystinuria might be chaperone therapy, which is useful for some diseases caused by mutations that lead to misfolded proteins (37). A pharmacological chaperone may stabilize an already folded protein against proteolytic degradation or thermal denaturation. This process accelerates the escape of mutated proteins from the endoplasmic reticulum associated protein degradation pathway, increasing the level of residual protein activity (38,39). As several mutations affecting the rBAT protein cause protein misfolding, chaperone therapy could be an attractive treatment strategy for patients with cystinuria in the future.
Acknowledgements
D.S.G. gratefully acknowledges support of the Rare Kidney Stone Consortium (U54KD083908), a part of NIH Rare Diseases Clinical Research Network (RDCRN), funded by the NIDDK and the NIH Office of Rare Diseases Research (ORDR).
Conflicts of Interest: D.S.G. has received honoraria for lectures from Mission Pharmacal, served as a consultant for Astra Zeneca and is an owner of the Ravine Group. The other authors have no conflicts of interest to declare.
References
- Garrod A. The Croonian lectures on inborn errors of metabolism. Lancet 1908;172:1-7.
- Verrey F, Singer D, Ramadan T, et al. Kidney amino acid transport. Pflugers Arch 2009;458:53-60. [PubMed]
- Fotiadis D, Kanai Y, Palacín M. The SLC3 and SLC7 families of amino acid transporters. Mol Aspects Med 2013;34:139-58. [PubMed]
- Chillarón J, Font-Llitjós M, Fort J, et al. Pathophysiology and treatment of cystinuria. Nat Rev Nephrol 2010;6:424-34. [PubMed]
- Calonge MJ, Gasparini P, Chillarón J, et al. Cystinuria caused by mutations in rBAT, a gene involved in the transport of cystine. Nat Genet 1994;6:420-5. [PubMed]
- Feliubadaló L, Font M, Purroy J, et al. Non-type I cystinuria caused by mutations in SLC7A9, encoding a subunit (bo,+AT) of rBAT. Nat Genet 1999;23:52-7. [PubMed]
- Goodyer P, Boutros M, Rozen R. The molecular basis of cystinuria: an update. Exp Nephrol 2000;8:123-7. [PubMed]
- Rosenberg LE, Downing S, Durant JL, et al. Cystinuria: biochemical evidence for three genetically distinct diseases. J Clin Invest 1966;45:365-71. [PubMed]
- Font-Llitjós M, Jiménez-Vidal M, Bisceglia L, et al. New insights into cystinuria: 40 new mutations, genotype-phenotype correlation, and digenic inheritance causing partial phenotype. J Med Genet 2005;42:58-68. [PubMed]
- Dello Strologo L, Pras E, Pontesilli C, et al. Comparison between SLC3A1 and SLC7A9 cystinuria patients and carriers: a need for a new classification. J Am Soc Nephrol 2002;13:2547-53. [PubMed]
- Eggermann T, Venghaus A, Zerres K. Cystinuria: an inborn cause of urolithiasis. Orphanet J Rare Dis 2012;7:19. [PubMed]
- Goodyer PR, Clow C, Reade T, et al. Prospective analysis and classification of patients with cystinuria identified in a newborn screening program. J Pediatr 1993;122:568-72. [PubMed]
- Ito H, Murakami M, Miyauchi T, et al. The incidence of cystinuria in Japan. J Urol 1983;129:1012-4. [PubMed]
- Lambert EH, Asplin JR, Herrell SD, et al. Analysis of 24-hour urine parameters as it relates to age of onset of cystine stone formation. J Endourol 2010;24:1179-82. [PubMed]
- Harnevik L, Fjellstedt E, Molbaek A, et al. Mutation analysis of SLC7A9 in cystinuria patients in Sweden. Genet Test 2003;7:13-20. [PubMed]
- Assimos DG, Leslie SW, Ng C, et al. The impact of cystinuria on renal function. J Urol 2002;168:27-30. [PubMed]
- Nakagawa Y, Asplin JR, Goldfarb DS, et al. Clinical use of cystine supersaturation measurements. J Urol 2000;164:1481-5. [PubMed]
- Coe FL, Clark C, Parks JH, et al. Solid phase assay of urine cystine supersaturation in the presence of cystine binding drugs. J Urol 2001;166:688-93. [PubMed]
- Goldfarb DS, Coe FL, Asplin JR. Urinary cystine excretion and capacity in patients with cystinuria. Kidney Int 2006;69:1041-7. [PubMed]
- Sumorok N, Goldfarb DS. Update on cystinuria. Curr Opin Nephrol Hypertens 2013;22:427-31. [PubMed]
- Evan AP, Coe FL, Lingeman JE, et al. Renal crystal deposits and histopathology in patients with cystine stones. Kidney Int 2006;69:2227-35. [PubMed]
- Mulay SR, Evan A, Anders HJ. Molecular mechanisms of crystal-related kidney inflammation and injury. Implications for cholesterol embolism, crystalline nephropathies and kidney stone disease. Nephrol Dial Transplant 2014;29:507-14. [PubMed]
- Mulay SR, Kulkarni OP, Rupanagudi KV, et al. Calcium oxalate crystals induce renal inflammation by NLRP3-mediated IL-1β secretion. J Clin Invest 2013;123:236-46. [PubMed]
- Mattoo A, Goldfarb DS. Cystinuria. Semin Nephrol 2008;28:181-91. [PubMed]
- de Boer H, Roelofsen A, Janssens PM. Antidiuretic hormone antagonist to reduce cystine stone formation. Ann Intern Med 2012;157:459-60. [PubMed]
- Torres VE, Chapman AB, Devuyst O, et al. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med 2012;367:2407-18. [PubMed]
- Fjellstedt E, Denneberg T, Jeppsson JO, et al. A comparison of the effects of potassium citrate and sodium bicarbonate in the alkalinization of urine in homozygous cystinuria. Urol Res 2001;29:295-302. [PubMed]
- Sterrett SP, Penniston KL, Wolf JS Jr, et al. Acetazolamide is an effective adjunct for urinary alkalization in patients with uric acid and cystine stone formation recalcitrant to potassium citrate. Urology 2008;72:278-81. [PubMed]
- Jaeger P, Portmann L, Saunders A, et al. Anticystinuric effects of glutamine and of dietary sodium restriction. N Engl J Med 1986;315:1120-3. [PubMed]
- Rodman JS, Blackburn P, Williams JJ, et al. The effect of dietary protein on cystine excretion in patients with cystinuria. Clin Nephrol 1984;22:273-8. [PubMed]
- Meschi T, Maggiore U, Fiaccadori E, et al. The effect of fruits and vegetables on urinary stone risk factors. Kidney Int 2004;66:2402-10. [PubMed]
- Lotz M, Bartter FC. Stone dissolution with D-penicillamine in cystinuria. Br Med J 1965;2:1408-9. [PubMed]
- Asplin DM, Asplin JR. The Interaction of thiol drugs and urine pH in the treatment of cystinuria. J Urol 2013;189:2147-51. [PubMed]
- Rimer JD, An Z, Zhu Z, et al. Crystal growth inhibitors for the prevention of L-cystine kidney stones through molecular design. Science 2010;330:337-41. [PubMed]
- Sahota A, Parihar JS, Yang M, et al. Novel cystine ester mimics for the treatment of cystinuria-induced urolithiasis in a knockout mouse model. In press Urology 2014.
- Wilmer MJ, Willems PH, Verkaart S, et al. Cystine dimethylester model of cystinosis: still reliable? Pediatr Res 2007;62:151-5. [PubMed]
- Ringe D, Petsko GA. What are pharmacological chaperones and why are they interesting? J Biol 2009;8:80. [PubMed]
- Fan JQ, Ishii S. Active-site-specific chaperone therapy for Fabry disease. Yin and Yang of enzyme inhibitors. FEBS J 2007;274:4962-71. [PubMed]
- Bartoccioni P, Rius M, Zorzano A, et al. Distinct classes of trafficking rBAT mutants cause the type I cystinuria phenotype. Hum Mol Genet 2008;17:1845-54. [PubMed]