
Estimates of over-time trends in incidence and mortality of prostate cancer from 1990 to 2030
Introduction
Prostate cancer, a common urologic malignant tumor, has become one of the most significant reasons for male health problems (1), and contributes to increased mortality. Due to changes in current population habits, customs and age structure, the number of elder men with prostate cancer has rapidly increased (2), and cancer-related deaths have also grown substantially. Besides, the risk factors of prostate cancer are various containing modifiable behavioral, metabolic, and environmental factors.
Owing to cancer incidence and death rate variety, the interest in prostate cancer-related burdens reached unprecedented heights (3,4). For different regions, suitable health policies for prostate cancer, containing cancer control and implementation plans, are relatively rare and the difficulty in policies making must be the absence of necessary data. This study therefore aims to describe the global burden of prostate cancer from 1990 to 2016 by age, region, and sociodemographic index (SDI) (a summary indicator of income per capita, educational attainment, and fertility), and afterwards project the fluctuation tendency for age-standardized morbidity and death rate to 2030 worldwide. Understanding these factors is necessary for detecting prostate cancer etiologies and their trends over time, without which targeted prevention strategies are impossible to design and evaluate, and promote strategic investments into research and clinical resources. At present, there are many researches on the burden of prostate cancer, but almost are based on the summary and analysis of the existing data, and few studies combined with the prediction of future morbidity and mortality trends. The practical significance of this kind of research should also be given enough attention.
Herein, we estimated the incidence, mortality trends in 195 countries and regions of prostate cancer from 1990 to 2016, and then, predicted the future trends, to 2030.
Methods
Data collection
In this study, researchers in our research team collected existing data from Global Burden of Disease data base (GBD) (ghdx.healthdata.org) by logging in and download the relevant data.
Data analysis
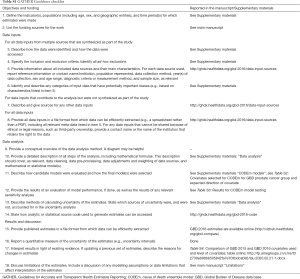
Previous papers have reported the common data analysis method and malignant tumor estimation model (5-11). Herein we present methods pertaining to the cancer outcomes for the incidence, mortality, trends, and predictions of prostate cancer from 2016 through 2030. In study process, we observed the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) (12).
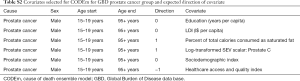
The detailed approach also complies with the GATHER guidelines, and the percent change is −0.98% (95% UI, −2.71% to 0.95%) before and after Cod Correct (level 3) by prostate cancer for all ages, 2016. In Supplementary materials (Tables S1-S9 and table online: http://fp.amegroups.cn/cms/f32730eb90bb505842fa7e703bdcab92/tau.2020.02.21-1.docx), the method and result of estimation are contained to help explain the work process (13,14). As in each prior study, the entire time series was re-estimated, and the results presented in this study supersede prior prostate cancer studies. Prostate cancers was defined in the International Classification of Diseases (ICD) were categorized into 4 cancer groups including C61-C61.9, Z12.5, Z80.42, Z85.46 in ICD-10 by incidence and 4 cancer groups containing C61-C61.9, D07.5, D29.1, D40.0 in also ICD-10 by mortality. For the collected data, we estimated national disease burden for 195 countries and territories. The incidence and death rates are reported per 100,000 person-years. The general world population is standardized by the calculation of age-standardized rates (1). 95% uncertainty intervals (UIs) are used for all estimates.
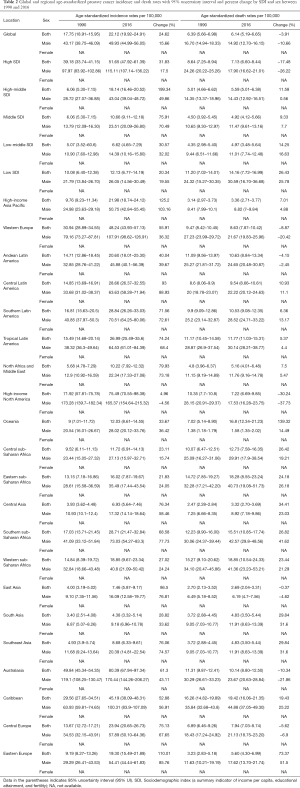
Full table
Full table

Full table

Full table

Full table

Full table

Full table
Full table

Full table
The present estimation process starts with cancer mortality. Prostate cancer death rates contain vital registration systems (85% of data in 2016), cancer registries (15% of data in 2016). Compared with 2015, the data increased respectively from 10,356 to 16,247 (57% increase) and 2,351 to 2,826 (20% increase), total change increasing 50%. For the absence of prostate cancer death data, previous study reported the estimation model which presents multiplying incidence with a separately modeled mortality-to-incidence ratio (MIR) to imitate real mortality. These mortality estimates are added to mortality data from the other sources and are used in a cause of death ensemble model (CODEm) (6). Simultaneously, we tested this model by real data and the test result was located in Supplementary materials. Covariates with the causal connection is used to estimate the prostate cancer data and we compared the GBD 2015 and GBD 2016 covariates, as well as displayed the covariates level. The prostate cancer incidence estimations are calculated by dividing MIR and prostate cancer specific mortality. Furthermore, we estimated the contribution of population ageing, population growth, and change in age-specific rates on the change in incident cases between 2006 and 2016. SDI is a summary indicator of income per capita, educational attainment, and fertility, and has been shown to correlate well with health outcomes and the SDI was grouped by geography, based on 2016 values. Data was analyzed by R software (x64 version 3.5.1), SAS (version 9.3) and SPSS (version 22.0).
Results
Over-time trends in incidence cases of prostate cancer from 1990 to 2016
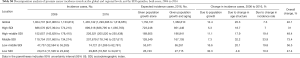
There were 1,435,742 (95% UI, 1,293,395–1,618,655) incident cases of prostate cancer in 2016 (Table 1), and it was 2.5-fold to new diagnoses [579,456 (95% UI, 521,564–616,107)] in 1990 at a global scale. In regions, the largest incidence cases appeared in high-income North America, followed by Western Europe, East Asia and high-income Asia Pacific, while Central sub-Saharan Africa was the region with fewest cases. The odds of developing prostate cancer were 1 in 16, ranging from 1 in 56 in low-middle SDI countries to 1 in 7 in high SDI countries (Supplementary materials). The increasing incidence rates, together with an aging and growing population, have led to a 160% increase in prostate cancer cases since 1990. Overall, 20% of this increase can be attributed to a change of population age structure, 12% to a change of the population size, and 7% to a change of the age-specific incidence rates (Supplementary materials). New diagnoses in men aged 70 years or older increased by more than three-fold from 1990 to 2016 [253,961 (95% UI, 176,952–327,260) to 795,593 (95% UI, 622,258–1,111,133)], accounting for 55.9% of incident prostate cancer cases in 1990 and 55.1% of incident cases in 2016.

Full table
Over-time trends in mortality of prostate cancer from 1990 to 2016
Prostate cancer was the leading cause of cancer death in 24 countries, ranking eighth globally, 6th in developed countries, and 12th in developing countries. There was a 2.0-fold increase in deaths [191,687 (95% UI, 168,885–209,254) to 380,916 (95% UI, 320,808–412,868)] (Table 1) in global level. Among regions, Western Europe, high-income North America, East Asia had the three most death cases in 2016 (Table 1), but compared with incidence cases changes, high-income North America and Western Europe deaths increase range was relatively slight. The death cases increased almost all SDI countries and the largest changes reported in middle SDI about 61% (Table 1). The high SDI have the greatest number of death cases followed by middle SDI, high-middle SDI, low-middle SDI and low SDI (Table 1). Deaths from prostate cancer among men aged 70 years and older nearly doubled from 1990 [120,450 (95% UI, 87,865–155,845), 76.7% of all prostate cancer deaths], to 2016 [236,884 (95% UI, 184,562–320,346), 80.9% of all prostate cancer deaths] at the global level.
Over-time trends in age-standardized incidence rate (ASIR) of prostate cancer from 1990 to 2016
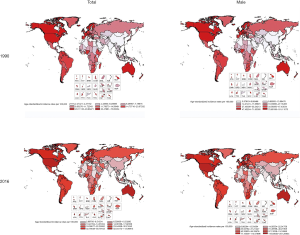
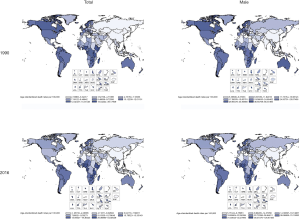
Globally, incidence and death rates raise considerably between 1990 and 2016, with the steep rise in ASIR of prostate cancer in men (1). According to the data, the global ASIR increased from 17.75 per 100,000 persons (95% UI, 18.91–15.95) in 1990 to 22.12 per 100,000 persons (95% UI, 19.92–24.91) in 2016. The change increases about 24.62% (Figure 1 and Table 2). In region level, average annual percent change in ASIR for prostate cancer by geography and gender showed the districts of obvious increase including most Asia, Russia, Africa and south America. For some classification, America in both sexes had an average annual percent change with range from 0 to 1, and in male the range changed from −1 to 0. When we observed China, the range both beyond 2 whether in both sexes or male. The acutely change is in high-middle SDI countries reaching 199%, and for others the increase also appeared obviously (Figure 1 and Table 2).
Full table
Over-time trends in age-standardized death rate (ASDR) of prostate cancer from 1990 to 2016
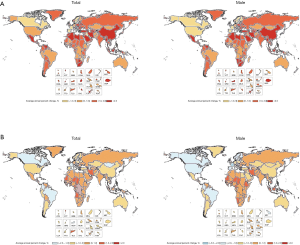
The global change of ASDR of prostate cancer has declined slightly, but in many regions, it still shows a trend of growth (Figure 2 and Table 2), for example: high-income Asia Pacific, central Latin America, southern Latin America, Tropical Latin America and so on (Figure 2 and Table 2). The most obvious decline has been found in high-income North America and acute increase observed in Oceania (Figure 2 and Table 2). Furthermore, the average annual percent change in ASDR for prostate cancer by geography and gender indicated the Russia, Africa and the Middle East change range was almost from 0 to 1 (Figure 3). For America, in both sexes the change ranges from −1 to 0 as well as in only male the range from −3 to −2, and for China, it also was same in both sexes and male from −1 to 0 (Figure 3).
Projections of prostate cancer incidence and mortality from 2017 to 2030
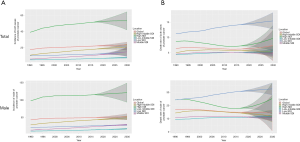
This study also forecast the trends in the incidence and mortality of prostate cancer from 2017 to 2030. Globally, the trend in prostate cancer incidence rate is increasing substantially (Figure 4). By SDI sub-types, the highest incidence rate of prostate cancer will occur with the greatest frequency in high SDI countries over the next years, followed by high-middle SDI countries, low SDI countries, middle SDI countries, and low-middle SDI countries (Figure 4). However, trends in prostate cancer deaths will slightly decrease from 2017 to 2030 worldwide (Figure 4). The highest death rates will occur in low SDI countries, followed by high SDI countries, high-middle SDI countries, and low-middle SDI countries (Figure 4). Trends in incident rates and deaths by sexes are listed in Figure 4. However, enough attention should also be paid to other trends in 95% UI because the real trend of change is likely to be in it, and may even be different from the fluctuation described above.
Discussion
On the global level, consistent growth tendency happened in both incident and death cases from 1990 to 2016. However, the incidence and mortality numbers of prostate cancer, in different ages, SDI countries and regions, reveal obvious differences. For instance, in low SDI countries, the patient numbers are significantly small when compared with other countries, especially, high SDI with the higher average life expectancy. Among urologic cancers worldwide, prostate cancer had continuously the largest growth in incident cases both in all SDI countries and in most regions from 1990 to 2016. As prostate cancer is more common in older men, the increase in population and age is bound to increase the incidence and death cases and increase the burden of prostate cancer.
However, the estimates presented in this study reveal remarkable differences in trends of incidence and death rates in prostate cancer. Analyzing time trends in prostate cancer, this study found a higher ASIR (change 24.62%) and a relatively lower ASDR (change −3.91%) through 1990 to 2016 on a worldwide scale. Enough diagnosis and treatment measures contribute to the less adverse cancer outcome. However, these services need adequate health care expenditures (15). Therefore, for these changes, the key factor is more and more health investment and government funding. Surely, the advancing treatment means and residents’ health awareness are also important reasons.
Population growth and average life expectancy rise could be used to explain the question that prostate cancer incidence substantially increase (16). However, the contribution of population ageing vs population growth to changes in incident cases differs substantially based on socioeconomic development. This leads to very different compositions of prostate cancer incidence reason in each country with different development level. Simultaneously, every disease, especially cancer, has a certain incidence probability. If some factors can increase the incidence probability of this disease in the population, it is called risk factor. By controlling these risk factors, the incidence of the disease in the population can be reduced. For example, fat, older age, family history, geographic location, ethnic origin, lack of exercise, environmental factors, dietary habits (dietary fat or specific fatty foods), tobacco smoking have all been suggested as contributing to the development of prostate cancer (17-21). In addition, exogenous factors such as patterns of sexual behavior, alcohol consumption, exposure to ultraviolet radiation, chronic inflammation (22), and occupational exposure can contribute to the development of prostate cancer. Conversely, based on the limited available evidence, reducing saturated dietary fats, for example eating more fish and less red meat and dairy products, more cruciferous vegetables (such as cabbage), and increasing the intake of soy, vitamin E, and selenium, may reduce the risk of prostate cancer (23). Prostate-specific antigen (PSA) screening has increased the number of screen-detected prostate cancer cases, although this “gold standard” method has also led to more questions.
Likewise, multiple factors can affect prostate cancer mortality rates together, such as high body mass index (BMI), smoking and alcohol consumption. Diabetes, heart disease, and severe malnutrition also have significantly influence in mortality of prostate cancer. At the same time, late findings make the prostate cancer that commonly have been advanced prostate cancer more difficult to treat, and also will progress the increase in mortality. The main reasons for late discovery are insufficient medical resources, weak health awareness and imperfect policies. Simultaneously, improved treatment, including radical prostatectomy, radiation therapy (24), and hormone therapy (25), appear to be reasonable explanations for the declining mortality trends in prostate cancer. In addition, increased detection of early stage prostate cancer as a result of the PSA test can reduce mortality by 20% (26,27). However, from our clinical observations, more prostate cancer patients have died of metabolic diseases, cardiovascular diseases, accidents, and psychological disease, problems for which there is lack of concern but play crucial roles in prostate cancer mortality. Future studies will further explore these issues.
Based on the collection data, we forecast the future fluctuations for ASIR and ASDR used to reflect the incidence and death rate separately. These change trends are from the calculation by using statistics method and professional tool, and at the same time, the operators have a wealth of statistical knowledge and practical experience. The prediction results of each region are quite different, and the fluctuation of incidence and mortality is not exactly the same. The change reason may be related to economic development, but the further explanation is not completely clear and needs further study.
Preventing cancer occurrence and reducing adverse cancer-relate outcome are challenging goals and will require commitments from all levels of society. Efforts to improve global urologic, medical oncology, and radiation oncology workforces are needed to prepare for the increasing number of prostate cancer patients worldwide and to prevent widening disparities in cancer outcomes. Simultaneously, improving the existing surgical workforce, promoting temporary task shifting, increasing the profile of surgery within public health through research and advocacy, and integrating surgical services with existing policies and initiatives such as the Millennium Development Goals and the Sustainable Development Goals have been cited as potential priority action areas. Moreover, the time trends as presented herein help highlight aspects of prostate cancer epidemiology that can guide intervention programs and advance research into cancer determinants and outcomes. Trends in cancer incidence will especially assist with resource allocation planning as a window into the future, which is sine qua non to inform health policy.
As far as we know, this is the first and unique research to analyze and estimate the trends in prostate cancer incidence and death rates from 1990 to 2030. Prior study researched incidence and mortality trends only on a country or only global level by analyzing the current data. Compared with it, our research contained existing data and projection with specific subgroup including age, region and SDI. This study also has some limitations. The data until 2016 is hysteresis and the projection range with only until 2030 may be not enough to instruct the control of disease.
Conclusions
After a detail analysis of time trend of collection data and projection about the prostate cancer incidence and death rate to 2030, the outcome shows that the incidence has substantially increased in the setting of population expansion and the change in age structure, while death rate has declined slightly for multiple factors. For different ages, regions and SDI countries, the detail results exhibit apparent difference. Our study combined with the specific national situation can help to formulate more suitable and efficient policies, adjust health care decision and innovate screening guideline by analyzing current data and predicting future.
Acknowledgments
Funding: This study was funded by China Postdoctoral Science Foundation Grant (No. 2019M660060), Natural Science Foundation of Tianjin (No. 19JCYBJC26900), The Science & Technology Development Fund of Tianjin Education Commission for Higher Education (No. 2018KJ050), Traditional Chinese medicine combined with Western medicine research project (No. 2019137), Youth Fund of the Second Hospital Tianjin Medical University (No. 2018ydey07), Tianjin Technical Expert Project and Hospital Innovation & Management Research Project of Tianjin Medical University (No. 2019YG08). We also thank the Global Burden of Disease Study for collection of the GBD data.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau.2020.02.21). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Akinyemiju TF, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2018;4:1553-68. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68:7-30. [Crossref] [PubMed]
- Znaor A, Lortet-Tieulent J, Laversanne M, et al. International variations and trends in renal cell carcinoma incidence and mortality. Eur Urol 2015;67:519-30. [Crossref] [PubMed]
- Center MM, Jemal A, Lortet-Tieulent J, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol 2012;61:1079-92. [Crossref] [PubMed]
- Fitzmaurice C, Allen C, Barber RM, et al. Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524-48. [Crossref] [PubMed]
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1151-210.
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1260-344.
- Fitzmaurice C, Dicker D, Pain A, et al. The global burden of cancer 2013. JAMA Oncol 2015;1:505-27. Erratum in: Errors in Author Names. [JAMA Oncol 2015]. [Crossref] [PubMed]
- Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks in countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287-323. [Crossref] [PubMed]
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800. [Crossref] [PubMed]
- Stevens GA, Alkema L, Black RE, et al. GATHER Working Group. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. PLoS Med 2016;13:e1002056. [Crossref] [PubMed]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1211-59.
- GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1345-422.
- Coleman MP, Quaresma M, Berrino F, et al. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol 2008;9:730-56. [Crossref] [PubMed]
- GBD 2016 Mortality Collaborators. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1084-150.
- Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008;371:569-78. [Crossref] [PubMed]
- Leslie SW, Soon-Sutton TL, Sajjad H, et al. Prostate Cancer. StatPearls [Internet], 2018.
- Kwabi-Addo B, Wang S, Chung W, et al. Identification of differentially methylated genes in normal prostate tissues from african american and caucasian men. Clin Cancer Res 2010;16:3539-47. [Crossref] [PubMed]
- Venkateswaran V, Klotz LH. Diet and prostate cancer: mechanisms of action and implications for chemoprevention. Nat Rev Urol 2010;7:442-53. [Crossref] [PubMed]
- Keogh JWL, McLeod RD. Body composition, physical fitness, functional performance, quality of life, and fatigue benefits of exercise for prostate cancer patients: A systematic review. J Pain Symptom Manage 2012;43:96-110. [Crossref] [PubMed]
- Leitzmann MF, Rohrmann S. Risk factors for the onset of prostatic cancer: age, location, and behavioral correlates. Clin Epidemiol 2012;4:1-11. [Crossref] [PubMed]
- Klein EA, Thompson IM Jr, Tangen CM, et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 2011;306:1549-56. [Crossref] [PubMed]
- Peschel RE, Colberg JW. Surgery, brachytherapy, and external-beam radiotherapy for early prostate cancer. Lancet Oncol 2003;4:233-41. [Crossref] [PubMed]
- Collin SM, Martin RM, Metcalfe C, et al. Prostate-cancer mortality in the USA and UK in 1975–2004: an ecological study. Lancet Oncol 2008;9:445-52. [Crossref] [PubMed]
- Andriole GL, Crawford ED, Grubb RL 3rd, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 2009;360:1310-9. [Crossref] [PubMed]
- Schröder FH, Hugosson J, Roobol MJ, et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014;384:2027-35. [Crossref] [PubMed]


