Does tunica anatomy matter in penile implant?
Introduction
The erectile rigidity of the human penis depends on sinusoids of the corpora cavernosa (CC) which function as a hydraulic system (1). It seems that the human CC are destined to encounter erectile dysfunction (ED), a kind of inability either to attain or maintain rigid erection for satisfactory intercourse (2,3). Interestingly the penis of every quadriceps is free of rigidity problem because it unexceptionally owns a rigid bone. It seems that human benefits nothing from penile evolution which advances os penis (a rigid body) to human CC (hydraulic system) if rigidity speaks volume (4,5). Not surprisingly pursuits for penile rigidity appear eternally endless in human history. The development of penile implant may be a good example. An implanted penis may mitigate rigidity problem, unfortunately it may risk the single penis at the expense of compromising tissue integrity once the CC is implanted.
Although the introduction of phosphor-di-esterase-5 inhibitors has significantly changed the therapeutic modalities in ED since 1998 (6), penile implantation is still the final viable solution to many patients with refractory erectile problem because it has been the best option to achieve reliable penile rigidity thus far (7). However, many candidates hesitate to this treatment because it is not natural and they are afraid of some unavoidable situations such as prosthesis loss, sinusoidal damage, revision surgery requirement, etc. Penile extrusion is one of the major concerns (8-10).
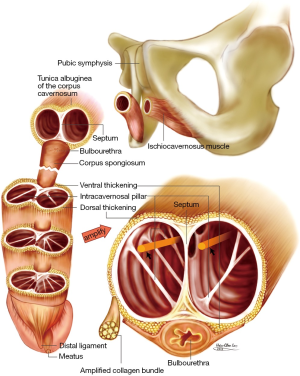
Modern intracavernous prosthesis has been available since 1950 (11). Both cylinders are the major components in each types of prosthesis including inflatable, semirigid and mechanical ones. The tunica albuginea (TA) is the envelop of the cylinders which preclude the penile shaft from too supple to provide sufficient rigidity for fulfilling intromission. The bi-layer structure of the TA was not elucidated as late as 1991 in the team of Lue (12). It was depicted as a 360° complete inner circular layer and a 300° incomplete outer longitudinal coat which varied much either the strength or thickness at specific anatomical locations (13). In particularly, there is an exclusive inner layer in between the 5 and 7 o’clock positions of the CC, the border between the CC and the corpus spongiosum. This region is vulnerable to prosthesis extrusion due to a paucity of the tuck outer longitudinal layer (14). Thus the attending surgeon may have no idea of this. We subsequently regarded this new found TA as a blueprint and derived a manual dexterity of handling the Hegar’s dilatator medial-dorsally toward the distal ligament of glans penis during corporal dilatation in penile implant surgery. Herein we analyze our clinical outcome before and after this change in 1991.
Patients and methods
From March 1987 to March 1991 while the TA was regarded as a circumferential single layer, 21 organically ED men, aged from 27 to 77, received penile prosthesis implantation and were allocated to conventional group. From August 1992 to March 2013 while the TA was known as a bi-layered structure with a 360° complete inner circular layer and a 300° incomplete outer longitudinal coat (Figure 1), 196 organically ED males, aged from 35 to 83, underwent penile implant and were categorized to advanced group.
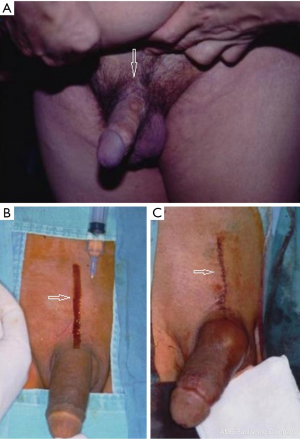
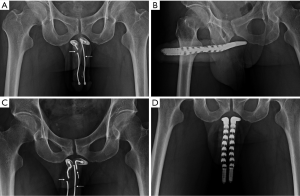
As a rule a circumferential approach was standard for semirigid, mechanical prothesis such as AMS600, AMS650, AMS Dynaflex, Duraphase (Figure 2A), Mentor malleable, Mentor acuform; a penoscrotal incision was used for implanting AMS ambicor and an extend pubic approach (Figure 2B,C) was specifically used for performing AMS700 CX implantation.
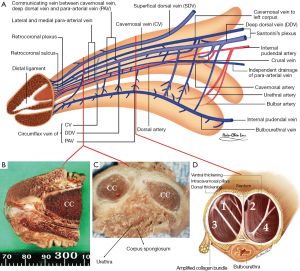
After the neurovascular bundle was protected, corporotomy was made on the CC (Figure 3A). Manual dexterity of handling the Hegar’s dilator was the major difference in those patients between the conventional and advanced group. During corporal dilatation, the tip of Hegar’s dilator was categorically directed medial-dorsally toward the distal ligament to avoid direct pressure on the region between the 5 and 7 o’clock position where the TA was composed of merely inner circular layer (Figure 3B,C). The intracavernosal pillars were kept lateral to both cylinders which have to be in the medial-dorsal positions, rooms one and two rather than rooms three and four (Figure 3D). After prosthesis was tailored to fit the CC, the corporotomy incision was closed with 6-0 nylon continuously with exact apposition of the TA and subsequently with interrupted sutures at each 2.5-cm interval for enhancement. The tubing system was fashioned and then the overlying fascia layers and skin were closed with 5-0 chromic suture layer by layer. The pain level was assessed with a 100-mm visual analog scale (VAS) at 2, 4, 8, 12 and 24 hours post surgery.
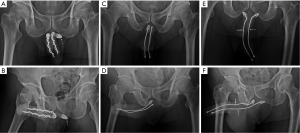
The model of prosthesis was recorded. Follow-up of patients including prosthesis survival, revision or end of patients’ life till August 2013. An anterior-posterior view of pelvis was undergone whenever patient revisited for either re-check or close observation. Proximal migration occurred merely in patients with semirigid prosthesis implant in 2 and 15 men to conventional and advanced group respectively (P=0.04) (Figure 4). Furthermore the prosthesis loss and revision surgery were analyzed and made when required (Figure 5). Six males concerning the penile length underwent penile elongation uneventfully (Figure 2A). Statistically student’s t-test or chi-squared test was either applied whenever necessary.
Results
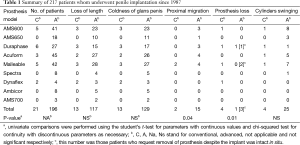
General data of the 217 patients are summarized in Table 1. To the conventional and advanced group, the number of inflatable and rigid type prosthesis used were 2, 19 and 15, 181 respectively, whereas the prosthesis loss was encountered in 50.0% (1/2), 15.8% (3/19) and 0.0% (0/15), 0.6% (1/181) respectively. Among them three men requested prosthesis removal and was excluded from statistical analysis. And the prosthesis survival time were 5.1-6.3 (5.7) years, 1.3-26.4 (15.2) years and 6.1-16.2 (11.2) years, 0.4-20.6 (15.3) years to the conventional and advanced group respectively. Statistical significance was noted on prosthesis loss (P=0.01) and proximal migration (P=0.04) in groups while the Mentor acuform stood out in prosthesis survival. Overall loss of penile length and coldness of glans penis were frequently complained by patients, 61.9% (13/21), 59.7% (117/196) and 61.9% (13/21), 65.8% (129/196) to the conventional and advanced group respectively regardless of prosthesis model. Cylinders swinging in the CC was common, which was relevant with the semirigid models and was 19.0% (4/21), 12.8% (25/196) to the conventional and advanced group respectively. One diabetic patient (4.8%) had prosthesis extrusion due to infection. The score of VAS varied from 11 to 45 mm with an average of 20.3±11.1 mm.
Full table
Discussion
Penile implant has been rising although a temporary weaning down at the early beginning in the era of medical treatment of ED. It is exemplified in the states that the number of patients undergoing a penile prosthesis increased from 17,540 in 2000 to 22,420 in 2009 (7), implying this surgical intervention remains a viable solution. It is a common surgery in the ED professional field. Thereafter it may be regarded as an easy surgery. It may deserve re-evaluation because many complications are still to be improved. Biomedical engineering improves the prosthesis coat, envelope, as well as the inner materials, interior design. Thus current ED males enjoy the advantages from biomedicine. However, the architecture of its envelope-to-be—TA was not underpinned in surgeons’ mind until 1992. Does improvement result from this elucidation? Further study is warranted.
The loss of length and glans coldness appears unavoidable. Fortunately many patients do not care much once the rigidity difficulty is mitigated. However, some males concern much on the condition that one’s preoperative erectile length is no longer than 10 cm. Penile enhancement may benefit this situation (15,16). This management is proved to be a viable option because a postoperative retraction of the penile shaft could be immune owning starched CC existing. We are looking for larger sample.
Although it seems occur in semirigid prosthesis, a proximal migration of implanted cylinders is one of the challenging issue in this study. Anatomy-based surgery prevents vulnerability of cylinder loss from distal CC and also enhances the prosthesis survival. A proximal migration appears uncommon in particularly once an implant male enjoy sex with female up position despite the patient is well informed preoperatively. A softer cylinder should be preferred if inflatable prosthesis is free from this issue. Could a further design sole this issue?
In this series, three males requested prosthesis removal despite the prosthesis was in good shape. Two older patients presented the reason that they prevented the disclosure of the implant to younger generation when deceased. A 57-year-old man, however, complained that the space occupying of implanted cylinder prevent the urethra from smooth patency in early 80s. Subsequently we advise to use as smaller cylinder as possible. It may contribute to many males presenting cylinder swinging within the CC. In our long term observation this may not be harmful. We therefore hesitate to agree the implant policy that a larger cylinder ought to be use (17).
The intracavernosal pillar originates from the inner circular layer of the TA and distribute from 2 o’clock or 10 o’clock to 6 o’clock positions. It acts much similar a strut in an aircraft wing and are fundamental to the structural integrity. During dilatation of the CC in preparing space for housing a prosthesis cylinder, it together with sinusoids may suffer from damage if a Hegar’s dilator tamps the CC fully. We therefore keep the dilatation as little as possible. The direction of the dilator is directed a little medially and dorsally to the distal ligament which is stout and strong.
In conclusion, we presented our experience of using this techniques in penile implant based on newfound anatomy. It offers an encouraging outcome although further evidences are still to be supplied.
Acknowledgements
We would like to thank Daniel Freeman for his English editing, along with Ms Hsiu-Chen Lu, Nicola Chen their preparations of illustration and photos for this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: It is an extension of the clinical application of an approved institutional review board of China Medical University and all patients received informed consent.
References
- Hsu GL, Hsieh CH, Wen HS, et al. Formulas for determining the dimensions of venous graft required for penile curvature correction. Int J Androl 2006;29:515-20. [PubMed]
- Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am 2005;32:379-95. v. [PubMed]
- Kaminetsky J. Epidemiology and pathophysiology of male sexual dysfunction. Int J Impot Res 2008;20:S3-10. [PubMed]
- Hsieh CH, Liu SP, Hsu GL, et al. Advances in understanding of mammalian penile evolution, human penile anatomy and human erection physiology: clinical implications for physicians and surgeons. Med Sci Monit 2012;18:RA118-25. [PubMed]
- Hsu GL, Lin CW, Hsieh CH, et al. Distal ligament in human glans: a comparative study of penile architecture. J Androl 2005;26:624-8. [PubMed]
- FDA approves oral therapy for erectile dysfunction. Am J Health Syst Pharm 1998;55:981-4. [PubMed]
- Montague DK. Penile prosthesis implantation in the era of medical treatment for erectile dysfunction. Urol Clin North Am 2011;38:217-25. [PubMed]
- Wilson SK, Delk JR, Salem EA, et al. Long-term survival of inflatable penile prostheses: single surgical group experience with 2,384 first-time implants spanning two decades. J Sex Med 2007;4:1074-9. [PubMed]
- Kaufman JJ, Lindner A, Raz S. Complications of penile prosthesis surgery for impotence. J Urol 1982;128:1192-4. [PubMed]
- Montague DK. Experience with semirigid rod and inflatable penile prostheses. J Urol 1983;129:967-8. [PubMed]
- Goodwin WE, Scott WW. Phalloplasty. J Urol 1952;68:903-8. [PubMed]
- Hinman F Jr. Penis and male urethra. In: Atlas of urological anatomy. WB Saunders. Philadephia, 1993.
- Hsu GL, Brock GB, Martinez-Pineiro L, et al. The three-dimensional structure of the tunica albuginea: anatomical and ultra-structural levels. Int J Impot Res 1992;4:117-29.
- Hsu GL, Brock G, Martínez-Piñeiro L, et al. Anatomy and strength of the tunica albuginea: its relevance to penile prosthesis extrusion. J Urol 1994;151:1205-8. [PubMed]
- Kwak TI, Oh M, Kim JJ, et al. The effects of penile girth enhancement using injectable hyaluronic acid gel, a filler. J Sex Med 2011;8:3407-13. [PubMed]
- Hsu GL, Chen HS, Hsieh CH, et al. Clinical experience of a refined penile venous stripping surgery procedure for patients with erectile dysfunction: is it a viable option? J Androl 2010;31:271-80. [PubMed]
- Benson RC Jr, Barrett DM, Patterson DE. The Jonas prosthesis--technical considerations and results. J Urol 1983;130:920-2. [PubMed]


