The epidemiology of renal trauma
Introduction
Renal trauma persists as a cause of significant morbidity and mortality at trauma centers across the globe despite the kidney’s relatively protected site within the retroperitoneum. This article reviews the modern epidemiology of renal trauma including the demographics of the affected patients, common mechanisms of blunt and penetrating injury, differences in adult and pediatric patients, and the distribution of injury severity. Non-operative and minimally invasive management techniques for both blunt and penetrating renal trauma have become standard of care over the past decades. With this increase, the use of angioembolization as a method of nonoperative care has increased, thus we will examine its use to manage renal trauma.
Methods
PubMed was accessed by the authors (BV, LL) in order to conduct a systematic review of published articles investigating renal trauma. “Kidney” and “Wounds and Injuries” were the Medical Subject Headings utilized to conduct a review of all articles in the past ten years (date of PubMed search: 3/22/2014). A total of 4,503 articles were identified. The following filters were applied after article identification: last ten years, full text available, English language, and humans. This reduced the number of manuscripts to 605. Manuscripts that accrued data from multi-center, single center, and national/regional databases were included. We excluded case reports and articles that did not include a majority (≥50%) of patient data years that fell within the past ten years (January 2003-March 2014). No studies were excluded a priori for weakness of study design or data quality.
We identified manuscripts from identical hospitals, so as to avoid data oversampling. Four duplicate series from identical hospitals were identified from the past ten years (1-8), and a decision was made regarding the most appropriate manuscript for our present study (1,3,5,7).
Each study was included in the final systematic review if the following a priori criteria were met: renal injuries stratified by American Association for the Surgery of Trauma (AAST) injury grade, patient number, study years, description of renal injury management, statement of blunt and/or penetrating injury, and statement of adult or pediatric study population. We were also interested in injury mechanism, concomitant injuries, age, sex, and renal-injury mortality; however, this data was not universally provided. As such, we abstracted the particular data when possible.
Regarding injury management, we were interested in open surgical and nonoperative management. Open surgical management was classified as any open surgicalintervention involving the injured kidney. Nonoperative management was stratified by observation and minimally invasive therapy. Minimally invasive therapy was defined as any of the following: diagnostic angiography, angioembolization, endoscopic ureteral stent, percutaneous nephrostomy, and perinephric drain. Some patients required multiple types of minimally invasive therapy; therefore, the total nonoperative procedures sometimes exceed the total patient number.
For the purposes of this study, nonoperative care was defined as the absence of an open surgical procedure. Observation was defined as the absence of any procedure. Minimally invasive therapy consisted of ureteral stent placement, perinephric drain placement, nephrostomy tube placement, diagnostic angiography, and angioembolization. Results were noted as “unknown” when we were unable to clearly discern the true number. We also attempted to define the success of immediate surgery when possible. If the data was not clear or absent, then we recorded the total number of open surgical procedures as “Open Total Surgery”.
Results
Of the 605 articles from the past decade that met our search criteria, a total of 15 adult and 5 pediatric articles were identified (Table 1). Nine adult (60%) and four pediatric (80%) manuscripts were focused solely on blunt trauma. Only two adult and zero pediatric manuscripts that met our a priori criteria focused solely uponpenetrating trauma, while the remaining manuscripts were a mixture of blunt and penetrating trauma.

Full table
Demographics
Renal trauma afflicts predominantly young males. A review of the 15 adult renal trauma articles includes 10,935 patients, 72% are male with a mean age of 30.8 years. The mean age of penetrating renal trauma patients is 28.0 and 88% are male. Of the 520 renal trauma patients reviewed in the pediatric literature, the mean age of renal trauma patients is 9.3 years with 67% of patients being male (Table 1).
Mechanisms
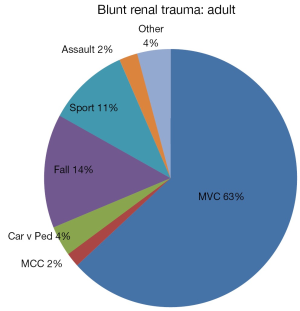
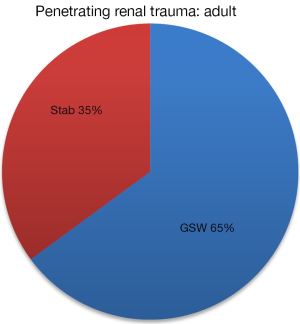
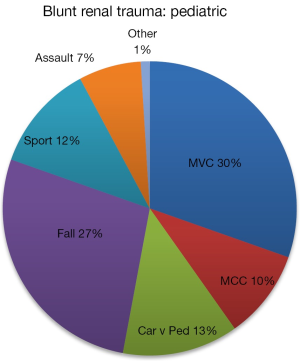
Mechanisms of blunt and penetrating trauma in adults and children were examined. A total of 9,119 adult blunt renal injuries were reviewed. In the adult renal trauma population, blunt renal injury is caused primarily by motor vehicle collisions (63%), followed by falls (43%), sports (11%) and pedestrian accidents (4%) (Figure 1). Of the 1,793 penetrating renal injuries in our series, firearms (65%) were more common than stab wounds (35%) (Figure 2). While the mechanisms of pediatric blunt renal injury are similar to the adult population, the distribution differs. A total of 458 pediatric blunt renal injuries were reviewed. The highest proportion of blunt pediatric renal injury is motor vehicle collisions (30%), while falls (27%) and pedestrian accidents (13%) were much more common in the pediatric population (Figure 3).
Injury severity
Of the 10,935 renal trauma patients, the distribution of renal injuries was: grade 1 (26%), grade 2 (28%), grade 3 (20%), grade 4 (19%) and grade 5 (7%). Of note, several of the articles reviewed were limited to only high grade renal injuries thus impairing any conclusions. A study of 3,247,955 injuries from the National Trauma Data Bank (NTDB) is more representative of the distribution of renal injuries seen at all trauma center levels, though with some over representation of level 1 trauma centers. The distribution of renal injuries in this study is the following: grade 1 (28%), grade 2 (30%), grade 3 (20%), grade 4 (15%) and grade 5 (7%).
The ISS is a scoring system derived from the abbreviated injury scale. ISS scores range from 0-75 (0 best to 75 not survivable). The score correlates to injury, with minor injury represented by a score of <9, moderate injury by a score of 9-14, severe injury by a score of 15-24, and critical injury by a score of ≥25. We noted that blunt and penetrating renal trauma is associated with overall moderate to severe trauma, as the mean ISS in our selected manuscripts is 22.5. This number is likely related to the large percentage of concomitant injuries, as renal trauma rarely occurs in isolation. The average length of hospital stay across the studies was 13.2 days.
The percentage of pediatric renal injuries included a higher percentage of high grade injuries; however, the number of publications is less than in the adult setting. The distribution of pediatric renal injuries is as follows: grade 1 (3%), grade 2 (2%), grade 3 (6%), grade 4 (68%), grade 5 (21%). Unfortunately, a large population study is not available. Only Hale and colleagues (9) reported the ISS and found a mean ISS of 21. Similar to the adult population, the average length of stay was 11.9 days.
Trends in management
Nonoperative care is the predominate form of management in adults and pediatric patients. Among manuscripts that include all AAST grades of renal injury, the median percent of nonoperative care for adult blunt renal injury is 94.8%. The median nephrectomy rate among manuscripts that included all grades of renal injury was low at 5.4%.
Diagnostic
Superselective angioembolization was not uniformly pursued in all of our identified manuscripts, as main renal artery embolization was occasionally performed. For example, main renal artery embolization was primarily utilized in lieu of open nephrectomy in one series for blunt main renal artery avulsions and blunt AAST grade 5 renal injuries (7/10 patients) (7). Overall 213 diagnostic embolization procedures were performed across eight manuscripts (Table 2). Sixty percent of cases proceeded to angioembolization. Twenty adjunctive procedures were necessary which included repeat angioembolization (10), nephrectomy (8), and perinephric drain placement (3) (Table 2).
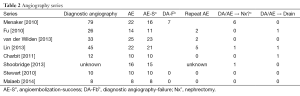
Full table
Discussion
Our review of literature from the past decade reveals that adult renal trauma continues to be an injury of younger, male patients. Renal trauma most commonly occurs in the setting of moderate to severe injuries, as injury severity scores ranged from 17-28.3 among the select manuscripts we reviewed. Renal trauma is also highly associated with concomitant injuries, as the association was 86% in a large national database study that included blunt and penetrating renal injuries (10). A total of 84% of the adult renal injuries and 89% of the pediatric renal injuries reviewed in this study were the result of blunt trauma. More than 50% of these were the result of motor vehicle collisions, underscoring the continued need for road safety. Children are three times as likely as adults of being the victims of pedestrian accidents.
Our review also confirmed what most urologists and trauma surgeons already know—nonoperative therapy has become standard of care. Unless the patient is hemodynamically unstable from their renal injury, nonoperative care should be considered for all grades of blunt and penetrating renal injury. We noted a consistent trend in which nonoperative care was more commonly used over open surgical care. Our review found that 94% of renal trauma care was nonoperative. Despite small patient numbers in the pediatric manuscripts, nonoperative care was more heavily used, with less than 3% of patients requiring nephrectomy (9,11-13).
In an effort to reduce unnecessary surgical interventions, superselective renal angioembolization has become an increasingly popular form of nonoperative management. Superselective renal angioembolization has further advanced the field of renal trauma by allowing select treatment of the injured portion kidney in lieu of total renal loss by main renal artery embolization or unfortunate nephrectomy that can occur following renal exploration (14,15). There can be negative consequences from non-judicious use of diagnostic angiography and the associated intravenous dye contrast load, as other intravenous contrast radiographic studies are often performed to evaluate associated trauma. Recently, an effort has been made to identify computed tomography findings that reliably predict the need for angioembolization following diagnostic angiography. Perirenal hematoma rim distance, intravascular contrast extravasation, and medial hematoma are examples that can predict whether diagnostic angiography with subsequent angioembolization should be pursued. When these specific radiographic findings have been combined with the need for red blood cell transfusion (≥2 U RBC), the positive predictive value has approached an 80-100% (16,17).
We acknowledge that there are limitations with our systematic review. First, we restricted our search to articles that were electronically available at our hospital and readily admit that we have subsequently missed additional articles. The articles we included each had specific primary aims that we retrospectively fit into our study aim. As such, there was missing data across the selected manuscripts that limited our ability to answer certain epidemiologic questions. For example, few manuscripts provided the percent of concomitant injuries and mechanism of injury. Despite these limits, we have attempted to answer our questions with available data and feel that the answers generated are pertinent.
Another unfortunate limitation is that it was not clear in some articles which patients underwent immediate operative intervention versus operative intervention following failed nonoperative care. In these circumstances, we opted to list all operative procedures irrespective of time event. Further, regarding nonoperative care, most manuscripts listed minimally invasive procedures performed but did not distinguish if they were done in the same patients or differing patients (i.e., a patient that underwent ureteral stent placement followed by perinephric drain for progressing urinoma). This has certainly led to misclassification in our ability to fully understand how many patients are affected by failure of observation or initial therapeutic care. Despite these limitations, we do feel that our review of the past decade does provide a glympse of how renal trauma care presents and is being managed in the modern era. With increased attention being given to the boundaries of nonoperative care, we would argue that equal attention be paid to a clear description of the associated demographics and subsequent management.
Conclusions
Renal trauma persists as a cause of morbidity, however rates of renal loss may be declining due to minimally invasive management techniques. The mechanism of injury continues to be overwhelmingly due to blunt trauma from motor vehicle collisions in a majority youthful, male population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shoobridge JJ, Bultitude MF, Koukounaras J, et al. Predicting surgical exploration in renal trauma: assessment and modification of an established nomogram. J Trauma Acute Care Surg 2013;75:819-23. [PubMed]
- McGuire J, Bultitude MF, Davis P, et al. Predictors of outcome for blunt high grade renal injury treated with conservative intent. J Urol 2011;185:187-91. [PubMed]
- Malaeb B, Figler B, Wessells H, et al. Should blunt segmental vascular renal injuries be considered an American Association for the Surgery of Trauma Grade 4 renal injury? J Trauma Acute Care Surg 2014;76:484-7. [PubMed]
- Figler BD, Malaeb BS, Voelzke B, et al. External validation of a substratification of the American Association for the Surgery of Trauma renal injury scale for grade 4 injuries. J Am Coll Surg 2013;217:924-8. [PubMed]
- Moolman C, Navsaria PH, Lazarus J, et al. Nonoperative management of penetrating kidney injuries: a prospective audit. J Urol 2012;188:169-73. [PubMed]
- Navsaria PH, Nicol AJ. Selective nonoperative management of kidney gunshot injuries. World J Surg 2009;33:553-7. [PubMed]
- Stewart AF, Brewer ME Jr, Daley BJ, et al. Intermediate-term follow-up of patients treated with percutaneous embolization for grade 5 blunt renal trauma. J Trauma 2010;69:468-70. [PubMed]
- Brewer ME Jr, Strnad BT, Daley BJ, et al. Percutaneous embolization for the management of grade 5 renal trauma in hemodynamically unstable patients: initial experience. J Urol 2009;181:1737-41. [PubMed]
- Hale N, Brown A. Mechanistic relationship of all-terrain vehicles and pediatric renal trauma. Urology 2013;81:160-2. [PubMed]
- McClung CD, Hotaling JM, Wang J, et al. Contemporary trends in the immediate surgical management of renal trauma using a national database. J Trauma Acute Care Surg 2013;75:602-6. [PubMed]
- Fitzgerald CL, Tran P, Burnell J, et al. Instituting a conservative management protocol for pediatric blunt renal trauma: evaluation of a prospectively maintained patient registry. J Urol 2011;185:1058-64. [PubMed]
- Mohamed AZ, Morsi HA, Ziada AM, et al. Management of major blunt pediatric renal trauma: single-center experience. J Pediatr Urol 2010;6:301-5. [PubMed]
- Tsui A, Lazarus J, Sebastian van As AB. Non-operative management of renal trauma in very young children: experiences from a dedicated South African paediatric trauma unit. Injury 2012;43:1476-81. [PubMed]
- Hotaling JM, Sorensen MD, Smith TG 3rd, et al. Analysis of diagnostic angiography and angioembolization in the acute management of renal trauma using a national data set. J Urol 2011;185:1316-20. [PubMed]
- Chatziioannou A, Brountzos E, Primetis E, et al. Effects of superselective embolization for renal vascular injuries on renal parenchyma and function. Eur J Vasc Endovasc Surg 2004;28:201-6. [PubMed]
- Lin WC, Lin CH, Chen JH, et al. Computed tomographic imaging in determining the need of embolization for high-grade blunt renal injury. J Trauma Acute Care Surg 2013;74:230-5. [PubMed]
- Charbit J, Manzanera J, Millet I, et al. What are the specific computed tomography scan criteria that can predict or exclude the need for renal angioembolization after high-grade renal trauma in a conservative management strategy? J Trauma 2011;70:1219-27. [PubMed]