
Complications and clinical management of ultrasound-guided renal allograft biopsies
Introduction
Ultrasound-guided percutaneous renal transplantation (Puncture biopsy) plays an essential role in the etiological diagnosis of acute/chronic renal injury after kidney transplantation. At present, routine pathological biopsies of transplanted kidneys have been carried out in China, and some of them are often programmed puncture biopsy. The international standard of Banff has reached the 2017 version, and the standardization of pathological diagnosis of renal allograft biopsies tissue can significantly increase the maneuverability and necessity of renal allograft biopsies.
Methods
General information and indications
From January 2006 to October 2018, ultrasound-guided renal allograft biopsies were performed in patients with abnormal renal transplantation function. Indications: through the follow-up of the patients, it was found that the patients had acute renal dysfunction, chronic renal dysfunction, albuminuria and microscopic hematuria (abnormal red blood cells), perioperative anuria, oliguria, and acute renal dysfunction.
Instruments and methods
Instruments
The Hitachi EUB-2000 ultrasonic instrument was selected, and the frequency of the probe was 3.5 MHz. BARD automatic biopsy gun and matching 16G or 18G side slot cutting needle or BARD disposable biopsy gun (model MC1816) were selected for biopsy and puncture, and the ejection distance was 1.5 to 2.2 cm.
The flow of puncture
Patients needed to stop using antiplatelet aggregation drugs and make routine preoperative preparations one week before puncture. At the same time, it was necessary to test the blood routine and blood coagulation function of the patients. Under the guidance of ultrasound, the oblique needle was inserted into the needle to avoid the internal organs, ilium blood vessels, hilar area of the kidney, and large blood vessels in the kidney and bladder. When the puncture needle reached the capsule of the transplanted organ, the ultrasonic CDFI state would avoid the vascular area of the interlobar artery, quickly pulled out the needle and pressed the puncture point after launching the automatic biopsy needle, and took out the puncture specimen. The conventional puncture was usually performed with 1 to 2 needles, not more than 3 needles. After the operation, the patients needed to be injected white eyebrow snake venom hemocoagulase intravenously and be pressed the puncture point with sandbags. After the puncture, it was necessary to observe the vital signs of the patient and whether the postoperative gauze of the patient is bleeding. The patient needs to stay in bed for 6 hours if the patient did not have naked eye hematuria after 12 hours to get out of bed, but the patient must avoid strenuous exercise within 1 month.
The criteria for evaluation
The successful pathological tissue criteria were as follows: there were at least 15 glomeruli in the tissue, and the pathological tissue needed to be interpreted by an experienced pathologist according to the Banff standard (1,2).
Statistical method
All the data were statistically processed by SPSS software, the measurement data were expressed as mean ± standard deviation, and the counting data were used.
Results
General situation
A total of 487 patients underwent renal allograft biopsies for various reasons. Of these 487 patients, there were 353 males and 134 females. The average age of the patients was 39.4±12.1. The average number of needles per puncture was 1.52±0.68. Under the light microscope, the number of glomeruli per specimen was 15.24±2.26, and the successful sampling rate was 98.8%. Only six samples were unable to make a definite pathological diagnosis because the number of glomeruli or renal vessels was not up to the standard.
The evaluation of the number of punctured glomeruli
In the early stage of renal allograft biopsies, it is necessary to use 18G puncture needle to puncture 1 tissue. After the pathologist evaluates the number of glomeruli, if the pathologist thinks that the number of glomeruli does not meet the diagnostic requirements, it is necessary to gradually increase the number of puncture tissues and replace larger puncture needles. Compared with the other three combinations in Table 1, the number of glomeruli punctured with 16G puncture needle was significantly higher than that of the other three combinations in Table 1. The data was statistically different (P<0.05).

Full table
Complication (please see Table 2 for details)
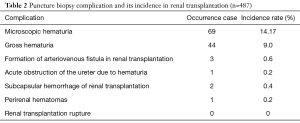
Full table
In this group, 69 patients developed microscopic hematuria symptoms, and the incidence rate was 14.17%, without special treatment. Forty-four patients had gross hematuria, with an incidence rate of 9.0%. There were three patients with an intrarenal arteriovenous fistula, with an incidence rate of 0.6%. Only one patient developed blood clots in renal pelvis, ureter, and bladder, with an incidence of 0.2%. There were two patients with subcapsular hemorrhage in renal transplantation, with a rate of 0.4%. One patient developed symptoms of perirenal hematomas, with a rate of 0.2%. Moreover, no patient developed symptoms of renal transplantation rupture.
The relationship between complication and puncture times and the size of the puncture needle
Through the analysis of the relationship between complication and the use of different types of puncture needles and puncture times, it was seen that there was no statistical difference in the incidence of complication between 16G and 18G, puncture of 1 or 2 tissues, P>0.05 (Table 3).
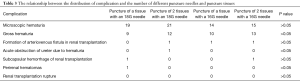
Full table
On the processing of complication
Microscopic hematuria
The patients with Microscopic hematuria were not treated with special treatment.
Gross hematuria
For the patients with Gross hematuria, they needed to prolong the bed rest time and sandbag compression time to 8 to 10 hours, and were observed the urine color and urine volume of the patients, and then removed the sandbag when the urine color gradually lightens, and they needed to stay in bed for 2 hours. Among them, one patient’s Gross hematuria symptoms increasingly aggravated, and there was still no urine after 3 hours. Color Doppler ultrasound showed that the patient had the symptoms of upper calyceal, ureter, and bladder blood clots, which needed surgical treatment. The rest of the patients had reduced hematuria and average urine volume and could get out of bed the next day after biopsies.
Formation of arteriovenous fistula in renal transplantation
Three patients underwent color Doppler ultrasound after Puncture biopsy. Color Doppler ultrasound showed that there was arteriovenous fistula in the transplanted kidney, but there was no special treatment. Through observation, the patient’s serum creatinine was stable.
Acute obstruction of the ureter due to hematuria
One patient had hematuria symptoms, and the patient still had no urine after 3 hours. Color ultrasound examination of the transplanted kidney showed that the patient had blood clots in the upper calyx, ureter, and bladder. At this time, considering that the patient had acute obstruction of the transplanted kidney and ureter, and the serum creatinine increased to 500 µmol/L, the patient was given alkalized urine and still had no urine. Cystoscopy on the second day showed that there were a large number of blood clots in the bladder. After the blood clots were washed out, there was no blood clot in the ureter opening of the transplanted kidney, and the reddish urine was ejected out of the ureter. After inserting the non-stent into the patient and indwelling the three-lumen catheterization tube for continuous bladder irrigation, the urine volume of the patients increased significantly, and the serum creatinine decreased to the preoperative level of renal allograft biopsies.
Subcapsular hemorrhage of renal transplantation
There were two patients with subcapsular hemorrhage of renal transplantation. The clinical manifestations were hematuria and urine deficiency, obvious pain in renal transplantation area, an increase of serum creatinine, and a decrease of hemoglobin. The patient underwent emergency renal transplantation exploration, and the subcapsular hemorrhage of the transplanted kidney could be seen during the operation, and the hematoma oppressed the transplanted organ and cleared the subcapsular hematoma. During the procedure, the morphology of the transplanted kidney recovered and the abdomen was closed after indwelling the drainage tube. After surgery, the urine volume of the patients increased significantly, and the serum creatinine decreased to the baseline level before puncture.
Perirenal hematomas
One patient developed perirenal hematomas, whose clinical manifestations were a pain in the graft area, decrease in hemoglobin, and no significant reduction in urine volume. The patient was treated with hemostatic drugs, and there was no significant increase in hematomas. The patient was treated conservatively and regularly reexamined by color Doppler ultrasound to indicate the absorption of hematomas.
Discussion
Kidney transplantation is the best treatment for patients with end-stage renal disease. How to improve the long-term survival rate of patients after transplantation has always been the most concerned issue for clinicians. Patients may have many problems after kidney transplantation, such as acute rejection, chronic rejection, CNI drug toxicity, recurrence of glomerulonephritis, or new glomerulonephritis, which may eventually lead to renal failure. Early and accurate diagnosis is a prerequisite for treatment, and the pathological diagnosis of renal allograft biopsies is the gold standard.
Successful puncture of qualified renal transplantation specimens is a prerequisite for pathological diagnosis. In this study, 487 cases of renal allograft biopsies were analyzed, and it was found that the success rate was 98.7%, which was consistent with the report (3,4). The number of punctured glomeruli increased with the use of thicker puncture needles, and the number of punctures increased, and the number of glomeruli obtained with 16G puncture needle was the highest, but this did not mean that complication would increase significantly. It also showed that the use of 16G puncture needle puncture of two tissues could provide better tissue specimens for pathological diagnosis, which was also consistent with the report (5).
The most severe complication in this group was acute ureter obstruction caused by subcapsular hematomas, perirenal hematomas, and hematuria. However, all of these diseases were cured by surgery, and none of the patients underwent nephrectomy because of the transplanted kidney Puncture biopsy complications. The incidence of significant complication was low, which was consistent with the literature (3,6). This also showed that ultrasound-guided renal allograft biopsies were safe, hematuria was directly related to puncture through the renal pelvis. However, subcapsular or perirenal hematomas were associated with the penetration of the interlobar artery and arcuate artery and effective compression, but not to the number of puncture needles and puncture times. It suggested that when using ultrasound guidance, we should pay attention to making use of the advantages of ultrasound and using CDFI mode. The puncture area should avoid the apparent arterial area, which could reduce the occurrence of complication such as bleeding. It was reported that the use of renal transplantation cortical tangent could significantly reduce the incidence of hematuria complication, from 3.8% to 1% (7,8). The frequency of central gross hematuria was 9%, which was consistent with previous reports, so we could consider learning to use renal transplantation cortical tangents to locate to achieve the purpose of reducing gross hematuria complication. It is reported that the incidence of intrarenal arteriovenous fistulas is 11% (9), compared with 0.6% in our study, which was inconsistent with the report. It is also reported that bleeding and other complication were associated with the use of aspirin (3). Our patients stopped using antiplatelet aggregation drugs one week before puncture biopsy, which reduced the incidence of bleeding and other complication.
In a word, ultrasound-guided renal allograft biopsies not only has a high qualified rate of pathological specimens but also has a very low incidence of complication; it is a safe and effective clinical measure. Furthermore, biopsies can provide meaningful pathological information for the clinic. We believe that the standardized puncture process is that patients need to stop using anticoagulants one week before puncture and do an excellent job of preoperative blood routine and blood coagulation function test. In the process of puncture, color Doppler ultrasound needs to be used to guide puncture, and hemostatic should be used during the operation, and reasonable compression and observation should be carried out. Patients need complete bed rest after the puncture, which can reduce the complications of renal transplant puncture biopsy and thus increase the safety of biopsy.
Acknowledgments
Funding: This work was supported by the Science and Technology Planning Project of Guangdong Province, China (grant number 2015B020226002).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee of the Second Affiliated Hospital of Guangzhou Medical University and the approval number was 2014074. All patients gave written informed consent before participation. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Racusen LC, Solez K, Colvin RB, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int 1999;55:713-23. [Crossref] [PubMed]
- Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant 2008;8:753-60. [Crossref] [PubMed]
- Baffour FI, Hickson LJ, Stegall MD, et al. Effects of aspirin therapy on ultrasound-guided renal allograft biopsy bleeding complications. J Vasc Interv Radiol 2017;28:188-94. [Crossref] [PubMed]
- Morgan TA, Chandran S, Burger IM, et al. Complications of ultrasound-guided renal transplant biopsies. Am J Transplant 2016;16:1298-305. [Crossref] [PubMed]
- Nicholson ML, Wheatley TJ, Doughman TM, et al. A prospective randomized trial of three different sizes of core-cutting needle for renal transplant biopsy. Kidney Int 2000;58:390-5. [Crossref] [PubMed]
- Furness PN, Philpott CM, Chorbadjian MT, et al. Protocol biopsy of the stable renal transplant: a multicenter study of methods and complication rates. Transplantation 2003;76:969-73. [Crossref] [PubMed]
- Patel MD, Phillips CJ, Young SW, et al. US-guided renal transplant biopsy: efficacy of a cortical tangential approach. Radiology 2010;256:290-6. [Crossref] [PubMed]
- Redfield RR, McCune KR, Rao A, et al. Nature, timing, and severity of complications from ultrasound-guided percutaneous renal transplant biopsy. Transpl Int 2016;29:167-72. [Crossref] [PubMed]
- Baffour FI, Hickson LJ, Stegall MD, et al. Effects of aspirin therapy on ultrasound-guided renal allograft biopsy bleeding complications. J Vasc Interv Radiol 2017;28:188-94. [Crossref] [PubMed]


