
Preventing the need for revision surgery after penile plication reconstruction of Peyronie’s deformities
Introduction
Peyronie’s disease (PD) is an acquired fibrotic penile deformity resulting in significant sexual dysfunction and psychosocial distress for both the patient and their partner (1,2). Although a myriad of nonoperative treatments have been proposed for PD, only intralesional collagenase clostridium has been FDA-approved for treatment of mild to moderate deformities (3,4). Surgical correction remains the gold standard for definitive treatment of patients with persistent bothersome curvature due to high efficacy and low morbidity (5).
Penile plication (PP) has become an increasingly popular surgical treatment for PD given its high success rate and lower risk of complications including loss of penile sensation and erectile dysfunction (ED). Surgical case logs among certifying urologists reported to The American Board of Urology reflect a 313% increase in PP from 2004–2013 (6). PP has been shown to be safe and effective for a wide variety of PD patients, with favorable long-term outcomes regardless of severity (7-12). Although revision rates appear to be low after PP, risk factors for PP failure include (I) poor initial response to intracavernosal injection (ICI), (II) inadequate numbers of corrective sutures, and (III) a lack of sutures at the proximal end of the penile shaft (5). Herein we present our updated experience with PP after implementing corrective measures to reduce failures.
Methods
After obtaining institutional review board approval, we conducted a retrospective review of all patients who underwent PP for PD by a single surgeon at our tertiary center between 2009 and 2018. Only patients with a minimum follow-up of six months were included. Patients with stable, bothersome penile curvature for at least six months were candidates for PP. Our minimally invasive PP technique was updated in 2016, and all patients were stratified into two groups for analysis—prior technique and current technique.
At initial evaluation, a comprehensive medical and sexual history was performed, including duration and progression of symptoms, history of trauma, erectile function, and history of prior treatments or procedures. Patients’ penile curvature and severity were determined by patient auto-photograph. Patients with ED were liberally prescribed oral phosphodiesterase-5 inhibitors to confirm adequate rigidity for penetration before PP. Men with refractory ED received concomitant penile prosthesis with PP and these patients were excluded from this analysis. Patients with an hourglass deformity were offered extratunical grafting with bovine pericardium in addition to PP (13).
Surgical technique
After induction of general anesthesia, an artificial erection is induced with ICI of 20 µg of alprostadil. If poor initial erectile response is noted, additional intracorporal saline injections are administered to achieve a sufficient erection for evaluation. Maximum degree of curvature is measured by consensus of the surgical team and photographs of the erect penis are taken from the lateral and inferior perspectives. Stretched penile length (SPL) was determined by compressing the suprapubic fat pad and measuring the dorsal distance between the pubic symphysis and the penile tip while on maximal stretch before and after plication after ICI.
Our minimally invasive surgical technique for multiple parallel PP without degloving has previously been described (7-12). PP is performed through a 2.5–3 cm longitudinal incision along the proximal or mid-shaft directly opposite the predominant direction of curvature. After the initial dissection is carried through the Dartos and Buck’s fascia, Senn or vein retractors are used to further expose the tunica albuginea. Beginning proximally, the tunica albuginea is then repeatedly corrected with multiple short inverting plication sutures of 2-0 Ethibond (Ethicon Inc., Somerville, NJ, USA). Each suture spans a total of 15 to 20 mm, while progressively retracting the incision distally over areas of greatest convexity. The patient is re-examined during proximal shaft manual corporal compression after each suture; additional sutures are placed until adequate correction of the deformity is achieved.
The incision is closed in 3 layers—Buck’s and Dartos fascia are closed in 2 layers using 2-0 and 4-0 Monocryl (Ethicon Inc.), and skin is closed in subcuticular fashion with 4-0 Monocryl and Dermabond (Ethicon Inc.). SPL measurements are repeated and a lightly compressive Coban (3M Company, Maplewood, MN, USA) dressing is applied. A penile ring block is performed using 0.25% bupivacaine. All patients are discharged on the same day and are asked to abstain from sexual activity until the day prior to their follow-up visit in 4 to 6 weeks for wound evaluation and assessment of deformity correction and sexual function.
Statistical methods
Perioperative data was compared between the prior PD technique and current technique groups using the Chi-square and independent sample t-tests for categorical and continuous variables, respectively. Statistical significance was considered at P<0.05 and reported P values are two-sided. All analyses were performed with SPSS®, version 25.0 (IBM Corp., Armonk, NY, USA).
Results
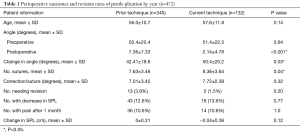
Of 472 PP patients who met inclusion criteria, 340 (72%) were in the early cohort [2007–2015], compared to 132 (28%) who had the current updated technique (Table 1). The revision rate decreased by more than half after the changes were implemented (3.8% vs. 1.5%). All patients cited persistent curvature as the reason for requiring revision surgery, while 3 out of the 13 revisions in the previous cohort listed palpable sutures as an additional reason. Mean preoperative angle of curvature was similar between the two groups (50.4 vs. 51.4 degrees, P=0.64), while the average residual postoperative degree was smaller in the current group (7.36 vs. 2.14 degrees, P<0.001). Median time to revision was much shorter in the previous cohort (5.6 months, IQR 3.67–22.5) than in the current (21.8 months, IQR 20.8–22.9). Fewer sutures were used in the previous cohort (7.63 vs. 8.38, P=0.04). After revision, all cases were functionally straight, with a mean postoperative curvature of 4 degrees at a median follow-up of 10.6 months (IQR 2.08–20.7).
Full table
Decrease in SPL was reported in 13.3% of patients overall (12.6% in the previous cohort vs. 13.6% in the current, P=0.77), and pain at the 1-month postoperative visit was found in 10.6% of patients in both cohorts. Three patients in the previous cohort with persistent pain required release of plication sutures with resolution of discomfort, while none in the current cohort required this procedure.
Discussion
The present study provides a large, single-institution experience of 472 patients undergoing PP and demonstrates the high efficacy and safety of the procedure for even the most severe deformities. Our revision rate of 1.5% in the current cohort compares favorably to previous plication studies, which range from 2.8–7.7% (5,9,14-17). To our knowledge, no other study has analyzed specific causes of plication failure and assessed whether improved outcomes could be achieved after targeting these causes. Our experience supports that the following three modifications to our technique in 2016 resulted in a lower revision rate (Figure 1): (I) using supplemental intracorporal saline injections for poor initial erectile response to ICI, (II) utilizing more corrective sutures and (III) placement of plication sutures beginning more proximally.
One third of patients with PD report some degree of concomitant ED, and placement of concomitant IPP has proven effective for those with severe refractory ED (11,18). Patients with mild to moderate ED may manifest insufficient erections after initial intraoperative ICI. We found previously that 71% of patients for whom plication initially failed had a poor response to intraoperative ICI, suggesting that additional saline injections may help unmask the patient’s true penile deformity and allow adequate correction (5).
Our previous study noted a tendency toward too few sutures placed along the proximal base of the penis in patients who needed revision surgery (5). Our overall experience with PP suggests that (I) more sutures are usually needed for adequate correction of curvature than what Gholami and Lue first described in 2002 with the initial 16-dot procedure, and (II) the number of sutures should correlate with severity of curvature (12,15). After adjusting our procedure by placing sutures more proximally, the current cohort received significantly more sutures than the previous one, resulting in a lower residual postoperative curvature. The patients in our current cohort who needed revision likely experienced alteration of their penile plaque rather than under-correction during initial plication, as evidenced by a much longer time to revision compared to the previous cohort (21.8 vs. 5.6 months).
Our experience suggests that Peyronie’s deformities often span the entire length of the penile shaft, and a wide distribution of multiple parallel sutures are needed to ensure definitive treatment. Placing higher numbers of shorter plicating sutures reduces tension on each individual corrective suture, thus achieving a “suspension bridge” straightening effect which we believe enhances correction and reduces pain in the postoperative period. We recommend using braided nonabsorbable sutures since previous studies have reported a high failure rate of 28.9% when absorbable sutures were used (19).
This is a retrospective, single surgeon study with its inherent biases. A relatively shorter follow-up time may explain the lower revision rate in the current cohort, but a higher average volume of cases per year in the current cohort supports the validity of our data (58.3 vs. 40.6). Given the rarity of plication failure, our sample size of reoperative cases was small. However, this study is among the largest ever reported and the first to critically analyze correctible causes of plication failure.
Conclusions
Plication failure may be caused by a poor initial erectile response to ICI, which masks the severity of deformity and results in an inadequate number of sutures placed. Ensuring adequate rigidity with additional injections and focusing corrective sutures in a proximal location can help prevent the need for revision surgery.
Acknowledgments
None.
Footnote
Conflicts of Interest: Dr. Allen F. Morey receives honoraria for being a guest lecturer/meeting participant for Boston Scientific and Coloplast Corp. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of The University of Texas Southwestern Medical Center at Dallas (ID #112010-125).
References
- Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease: a review. J Sex Med 2013;10:653-60. [Crossref] [PubMed]
- Davis SN, Ferrar S, Sadikaj G, et al. Female Partners of Men With Peyronie's Disease Have Impaired Sexual Function, Satisfaction, and Mood, While Degree of Sexual Interference Is Associated With Worse Outcomes. J Sex Med 2016;13:1095-103. [Crossref] [PubMed]
- Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol 2013;190:199-207. [Crossref] [PubMed]
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie’s Disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- Cordon BH, Sundaram V, Hofer MD, et al. Penile Plication as Salvage Strategy for Refractory Peyronie’s Disease Deformities. Urol Pract 2017;4:149-54. [Crossref]
- Oberlin DT, Liu JS, Hofer MD, et al. An Analysis of Case Logs From American Urologists in the Treatment of Peyronie's Disease. Urology 2016;87:205-9. [Crossref] [PubMed]
- Dugi DD 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int 2010;105:1440-4. [Crossref] [PubMed]
- Adibi M, Hudak SJ, Morey AF. Penile Plication Without Degloving Enables Effective Correction of Complex Peyronie's Deformities. Urology 2012;79:831-5. [Crossref] [PubMed]
- Hudak SJ, Morey AF, Adibi M, et al. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol 2013;189:1019-24. [Crossref] [PubMed]
- Chung PH, Tausch TJ, Simhan J, et al. Dorsal plication without degloving is safe and effective for correcting ventral penile deformities. Urology 2014;84:1228-33. [Crossref] [PubMed]
- Chung PH, Francis Scott J, Morey AF. High Patient Satisfaction of Inflatable Penile Prosthesis Insertion with Synchronous Penile Plication for Erectile Dysfunction and Peyronie's Disease. J Sex Med 2014;11:1593-8. [Crossref] [PubMed]
- Reddy RS, McKibben MJ, Fuchs JS, et al. Plication for Severe Peyronie's Deformities Has Similar Long-Term Outcomes to Milder Cases. J Sex Med 2018;15:1498-505. [Crossref] [PubMed]
- Reed-Maldonado AB, Alwaal A, Lue TF. The extra-tunical grafting procedure for Peyronie's disease hourglass and indent deformities. Transl Androl Urol 2018;7:S1-6. [Crossref] [PubMed]
- Kadirov R, Coskun B, Kaygisiz O, et al. Penile Plication With or Without Degloving of the Penis Results in Similar Outcomes. Sex Med 2017;5:e142-7. [Crossref] [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 Patients. J Urol 2002;167:2066-9. [Crossref] [PubMed]
- Papagiannopoulos D, Yura E, Levine L. Examining Postoperative Outcomes after Employing a Surgical Algorithm for Management of Peyronie's Disease: A Single-Institution Retrospective Review. J Sex Med 2015;12:1474-80. [Crossref] [PubMed]
- Papagiannopoulos D, Phelps J, Yura E, et al. Surgical outcomes from limiting the use of nonabsorbable suture in tunica albuginea plication for Peyronie's disease. Int J Impot Res 2017;29:258-61. [Crossref] [PubMed]
- Bilgutay AN, Pastuszak AW. Peyronie's disease: a review of etiology, diagnosis, and management. Curr Sex Health Rep 2015;7:117-31. [Crossref] [PubMed]
- Hsieh JT, Liu SP, Chen Y, et al. Correction of Congenital Penile Curvature Using Modified Tunical Plication with Absorbable Sutures: The Long-Term Outcome and Patient Satisfaction. Eur Urol 2007;52:261-6. [Crossref] [PubMed]



