Supine percutaneous nephrolithotomy: tips and tricks
Percutaneous nephrolithotomy (PCNL) was first described by Fernström and Johansson in 1976 in prone position (1). Since then, this surgical approach has become the gold standard for treatment of large stones and it has evolved over time resulting in decrease in invasiveness and morbidity and improvements in ergonomics and outcomes. Originally, PCNL was performed in the prone position due to concerns that other positions increased risk of inadvertent colon injury during percutaneous puncture of the kidney. At the time the original PCNLs were performed, intravenous pyelography was the standard imaging modality for stone disease and current modern cross-sectional imaging techniques such as ultrasound or computerized tomography (CT) were not commonly used—thus, the surgeons who performed early PCNL did not have the knowledge of peri-renal anatomy which is readily available to the modern urologist.
In 1987, Valdivia Uría postulated that PCNL could be performed in the supine decubitus position and using pre-operative CT scans for patient evaluation, demonstrated similar outcomes and complications for PCNL performed in the supine position with potential advantages in terms of ergonomics and the administration of anesthesia (2,3). In addition, subsequent studies of the relationship of peri-renal organs to the kidney using CT have demonstrated that the risk of colon perforation, the complication which drove early PCNL to be performed in the prone position, is actually less risk in the supine position, with the incidence of retro-renal colon position in supine versus prone position being 1.9% versus 10% respectively (4), definitely fading the idea of higher risk of puncturing the colon in supine than in prone. Though prone position remains the dominant position for PCNL, the use of supine PCNL is increasing—20% of all PCNLs entered into the Global PCNL study of the Clinical Research Office of the Endourological Society were performed in the supine position (5). Herein we review several approaches to percutaneous renal access in the supine position, with a focus on variations in patient positioning and puncture technique.
Evolution of patient positioning from Valdivia to Valdivia-Galdakao to Giusti positions
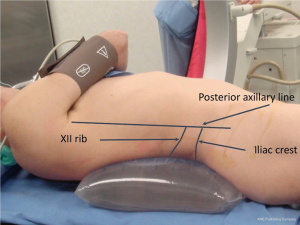
In general, after positioning the patient, it is important to mark the inferior edge of the 12th rib, the iliac crest and the posterior axillary line on the patients’ skin in order for the surgeon to maintain his or her orientation after the patients are draped.
In our practice, we commonly position the patient 6 cm away from the radiopaque edge of the operating table so that the fluoroscopic evaluation of the kidney and puncture tract are not impaired by the radio-opaque portion of the operating bed. In some centers, newer radiolucent carbon tables adapted specifically for endourological procedures lack this radio-opaque edge and allow for the patients to be positioned closer to the edge of the bed—this may be advantageous in terms of maneuverability of the nephroscope and decreased incidence of collision between the nephroscope and the bed when the nephroscope is used at wider angles. Finally, the ideal table should be able to maneuver caudally so the C-arm can be used to evaluate the entire genitourinary tract. If the bed does not meet this requirement in its standard configuration, one solution is to use the bed in reverse position or to add a Mayo table to hold patients’ feet.
The original description of supine PCNL by Valdivia included the placement of a 3-liter saline back beneath the patient’s flank to improve exposure to the area where the percutaneous puncture is performed (2) (Figure 1). Over the last decade different variations in positioning have been described, lateral (6), complete supine (7) and modified supine positions (8-10).
The most commonly used position is the Galdakao-modified Valdivia position (8) which is an evolution of the Valdivia’s supine position. In this position, the patient’s legs are placed in a modified lithotomy position with both legs in stirrups in order to facilitate simultaneous percutaneous antegrade access and ureteroscopic and also retrograde transurethral access to the urinary system.
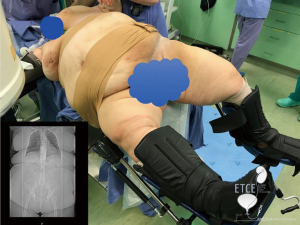
We have recently created a new modification to the Galdakao-Valdivia position, in order to overcome potential limitations in terms of nephroscope maneuverability resulting from the nephroscope pushing against the stirrup support (11), especially when trying to reach the upper pole from a lower pole access. These new modifications are termed “Giusti’s position” and are shown in Figure 2: the patient is placed at the lateral edge of the table and the flank is gently elevated by means of a small bolster to obtain a mild rotation with an angle not exceeding 15–20°. The ipsilateral arm is placed lying over the thorax avoiding any stretch of the brachial plexus in order to allow for cephalad free tilting of C-arm during puncture. The leg of PCNL side is left straight on half of the operating bed without the stirrup and a single stirrup is placed to support the contralateral leg so there is substantial room for a second surgeon to perform retrograde transurethral ureteroscopy simultaneously.
Pros and cons of supine position
Pros
Improvements in anesthetic management
Supine position for PCNL certainly offers some advantages over prone PCNL in terms of anesthesiologist management including the following: improved access to the patient for cardiovascular and pulmonary management, especially during an emergency situation, less risk of injury to central and peripheral nervous system (e.g., vascular, peripheral nerve and cervical spine injuries, tracheal compression and ocular damage) which are more commonly associated with prolonged prone anesthesia, and less risk of thromboembolism due to the lack of inferior vena cava compression (12), and improved ventilator-associated parameters for obese patients (13). Finally, fluid absorption is also reduced in the supine position (14); this is particularly important in patients with compromised cardiovascular status (15) as well as those at risk for systemic infection due to struvite or non-struvite stones colonized with bacteria.
Specific to issues with patient ventilation, the movement of patients from the supine position to the prone position after intubation in patients undergoing prone PCNL increases the risk of single-lung ventilation should the endotracheal tube be displaced while the patient is repositioned. Supine PCNL eliminates the risk of this pulmonary complication. Moreover, there is no need for extra anaesthesiologic equipment such as reinforced endotracheal tubes, stabilizing helmet, specialized paddings which may add additional cost to the procedure (16,17).
Improvements in patient positioning and shorter operative time
Supine PCNL results in decreased workload for operating room (OR) personnel because there is no need to reposition the patient after ureteral catheter placement as is the case for standard prone PCNL. For supine PCNL a single draping and position is used throughout the entire procedure. This advantage is even more evident in obese patients (18) (Figure 3). The lack of need for repositioning the patient after induction of general anesthesia or after placement of ureteral catheter result in a shorter overall operative time for supine PCNL compared with prone PCNL which has been demonstrated in several reports (19,20).
Decreased intrarenal pressures
In supine position, the angle of the renal sheath typically is parallel to the floor or angled downward facing the floor. This is the opposite of the orientation of the renal sheath during prone PCNL, where the sheath is angled upwards towards the ceiling (i.e., away from the floor). Angulation of the renal sheath during supine PCNL therefore results in in increased drainage of fluids and stone fragments from the kidney. This continued spontaneous evacuation of fluid from the renal pelvis in the supine position could potentially lead to decreased renal pelvis pressures and theoretically lower infectious risk after PCNL (21). One disadvantage of the sheath angle in supine position is that the collecting system may be more difficult to distend and this may require greater amounts of fluid irrigation to perform adequate endoscopic evaluation of the collecting system.
Decreased radiation exposure and improved ergonomics of fluoroscopy
Radiological exposure to the surgeon is reduced during supine PCNL because the surgeons’ hands are not directly under the X-ray beam. This is in contrast to prone PCNL, where there is significantly greater risk that the surgeon’s hands are inside the radiation field when performing standard prone access techniques of triangulated or bull’s eye guided puncture. Nevertheless, no comparison data have been published yet. Another advantage of supine position, is that due to the more lateral skin position for renal puncture in the supine position, there is typically the C-arm can be moved freely to evaluate the entire kidney during surgery without risk of “bumping into the nephroscope” or “displacing the nephroscope” which may occur more frequently in the prone position. Finally, in addition, the surgeon can work comfortably sitting down avoiding back stress due to prolonged uncomfortable standing with patients in the supine position, which is not possible when performing prone PCNL.
Easier endoscopic combined intrarenal surgery (ECIRS) or simultaneous bilateral endoscopic surgery (SBES)
The supine position, either in traditional Valdivia-Galdakao or in Giusti-modified Valdivia position, can facilitate simultaneous manipulation antegrade and retrograde transurethral approaches to complex stone disease. ECIRS-supine PCNL with the addition of retrograde transurethral flexible ureteroscopy (fURS) was popularized by Scoffone in order to maintain high stone free rates of PCNL while decreasing the need for additional punctures to render patients stone free (22). ECIRS was firstly described by Grasso et al. back in 1993 in prone position (23), but, the lack of ergonomics of prone decubitus (i.e., the difficulty of prone retrograde ureteroscopy for patients undergoing prone PCNL) prevented the dissemination of this integrated. On the other hand, retrograde ureteroscopy at the time of PCNL is easily accomplished in the supine position and ECIRS is commonly performed by those who perform supine PCNL. Furthermore, supine PCNL and ECIRS may facilitate “endovision technique” or ureteroscopic-guided puncture during which puncture of the targeted calyx can be monitored ureteroscopically in order to confirm proper placement of the needle through the renal papilla.
Single-session bilateral PCNL has been shown to be safe and feasible in the supine position. While one may argue that in the case of single-session bilateral PCNL the advantage of supine position (over prone position) in terms of operative time is outweighed by the necessity of changing position and draping between one side and the other, while in prone there is no need for that (24). However, Proietti et al. showed that the total operative time (120±45.4 minutes) for single-session bilateral PCNL was comparable to those reported in the literature for prone BPCNL (25).
Recent publications have described the newest frontier in percutaneous stone surgery—SBES combining supine PCNL and fURS in tandem fashion at the same time—that is, one surgeon performs supine PCNL while simultaneously another surgeon performs a contralateral fURS (26). This novel technique was recently shown to be safe and feasible in a pilot study and has theoretical advantages of decreasing operative and anesthetic times in patients with bilateral nephrolithiasis.
Improved endoscopic access to the upper pole from lower pole puncture tract
Another aspect of PCNL that favors the supine position is that upper calyx endoscopic approachability through the lower calyx puncture tract is significantly higher in supine than in prone PCNL. This is possibly due to a thinner body wall, a thinner muscular layer, a lower muscle-to-fat thickness ratio generating and a wider angle between the lower and upper calyx axes afforded by the supine position. Sofer et al. demonstrated that it is possible to reach the upper calyx from the lower calyx puncture in 80% of cases for supine PCNL compared with only 20% of cases of prone PCNL (27) (Figure 4). We feel that this is an important advantage of supine PCNL—access to the lower pole, renal pelvis, and upper pole can more effectively be accomplished through a lower pole puncture tract, which may, in turn decrease the need for upper calyx puncture and reduce the risks of thoracic complications associated with upper pole puncture in the prone position (28).
Cons
Mobility of the kidney
One the most important drawbacks of supine position is the mobility of the kidney that is generally greater in the supine position than the prone position (Figure 5). In some patients, especially the those with BMI <25 kg/m2, the mobility of the kidney is noticeable during percutaneous puncture and subsequent dilation. This mobility is seen to a far lesser extent in the prone position where the kidney is fixed by the weight and rigidity of the posterior abdominal wall against the operating table.
Some tricks to stabilize the kidney and therefore limit this mobility during supine puncture are as follows:
- Apply abdominal compression with the surgeon’s or assistant’s hand during puncture;
- Place the guidewire in a “through-and-through” fashion (i.e., pass the guidewire into the bladder, then retrieve this with a cystoscope so there is through-and-through access);
- Place a ureteral access sheath in a retrograde fashion;
- Decreased the caliber of the renal access sheath—the smaller sheaths (such as mini PCNL) appear to create less renal mobility during placement than the larger bore renal sheaths.
Longer percutaneous tract
In the supine position, percutaneous puncture comes from a more lateral position on the patient’s flank than in prone position—this may increase the tract length in patients undergoing supine PCNL when compared with prone PCNL. In contrast, during prone PCNL, tract length is generally shorter. This may also be due, in part to the fact that the anterior abdominal wall is more pliable than the posterior abdominal wall. The more compliant anterior abdominal wall transmits pressure of the bed to the kidneys in the prone position, limiting the mobility of the kidneys and shortening the percutaneous tract (29,30).
That being said, the point at which the renal access sheath enters the kidney acts as a fulcrum. The farther this fulcrum is from the skin (e.g., longer access tract) the less maneuverable the distal end of the sheath will be within the collecting system. As a consequence, the surgeon may need to adjust his or her technique to accommodate limitations in rigid nephroscopy or excessive torqueing in the supine position. These limitations may be overcome by routine use of a flexible nephroscope during supine PCNL. This is consistent with the recently published American Urological Association (AUA) Guidelines which suggest that flexible nephroscopy should routinely be performed during PCNL (regardless of patient position) (31). From a practical standpoint, when planning to perform supine PCNL, it may be useful to have longer length rigid nephroscopes and Amplatz sheaths. We recommend placing a “safety suture” on the plastic Amplatz sheath when performing supine PCNL in obese patients to avoid inadvertent migration of the sheath beneath the surface of the skin.
Supine PCNL: puncture technique
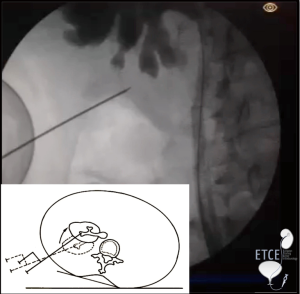
X-ray-guided puncture: triangulation
Puncture begins with the in 0° degrees, neutral position. The orientation of the needle is almost parallel to the floor and the percutaneous tract is typically horizontal in orientation. After retrograde pyelography, the advancement of the needle is followed fluoroscopically in real-time. When the needle is in the proper trajectory, the surgeon will observe the needle depressing the targeted calyx and then the needle can be advanced through the papilla and into the renal collecting system. These details are readily in supine position because the C-arm orientation is perpendicular to the trajectory of the needle. Some surgeons have argued that when performing PCNL in the prone position, if the C-arm is in the oblique position instead of perpendicular to the needle, then this depression of the calyx of interest may be more difficult to appreciate.
If the fluoroscopic image with the C-arm at 0° show demonstrates that the needle is superimposed over the desired calyx but no urine is returned, it is possible that the depth of the puncture must be adjusted. To evaluate the puncture in order to achieve the correct depth, the C-arm is rotated 30° degrees cephalad. When comparing this cephalad view to the fluoroscopic images with the C-arm in the 0° position, if the needle has moved below the targeted calyx, this suggests that the trajectory should be adjusted to be more posterior in orientation; if the needle moves above the targeted calyx, then the needle trajectory should be adjusted more anteriorly.
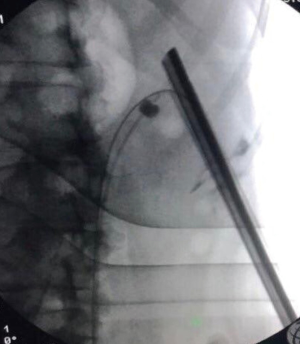
X-ray-guided puncture: the cross-table bullseye technique
A different approach to fluoroscopic-guided percutaneous renal access in the supine position is the “Cross-table bullseye technique”. This technique was modelled after the bullseye technique which has been used to perform prone puncture during PCNL for many years (32). In the supine position, this technique defines the position on the patients flank skin to begin the puncture for a puncture that is exactly parallel to the floor. A step-by-step description of the cross-table bullseye puncture technique is as follows:
- A scout film is performed with the C-arm at the 0° position;
- The C-arm is then rotated completely beneath the patient and a “cross table” image is taken—the position of the desired calyx (or calyces) of entry is marked on the skin with the C-arm in the cross-table position (Figure 6);
- The C-arm is then moved back to the 0° position and the puncture is performed with the needle parallel to the floor. If the puncture is in the correct position, depression of the calyx can be observed;
- If urine is not returned, cephalad rotation of the C-arm is performed to adjust the depth of the puncture as described in the paragraph above.

Ultrasound-guided supine PCNL
Supine percutaneous puncture may be also performed combining fluoroscopy and ultrasound or under complete ultrasound guidance (i.e., “X-ray free”).
The advantages of ultrasound-guided puncture include the following:
- Easy identification of the correct depth of the puncture without need for C-arm adjustment;
- The ability to survey the peri-renal anatomy to evaluate for potential injury to the liver, spleen, intestines, or pleura;
- Reduced radiation exposure for the patient and the OR personnel;
- Recent studies have reported on the safety and feasibility of X-ray free PCNL in the prone position (33,34), but no data have been published to date in patients undergoing supine PCNL.
Outcomes
Currently, it is generally accepted that prone and supine PCNL have equivalent stone free rate and complication rates based on several prior publications (5,35,36). One perceived barrier to greater adoption of the supine position for PCNL is that given that supine PCNL accounts for nearly 20% of PCNLs worldwide (5), many surgeons learned PCNL from mentors who practice the prone position. Many surgeons would acknowledge that a position change from prone to supine for a surgery that can be performed with a high success rate in the prone position may be something that experienced prone surgeons are reluctant to take on. In a study of this particular topic, Sofer et al. demonstrated that changing position is not cumbersome and the learning curve short, yielding similar, or even better outcomes, rather quickly for an experienced urologist or endourologist (37).
In conclusion, in our opinion the balance between pros and cons clearly favors supine position for PCNL. Experience gained in more than one decade of supine PCNL allowed us to identify some tips and tricks to facilitate transition from prone to supine position and to optimize its outcomes while minimizing complications’ rate.
Acknowledgments
None.
Footnote
Conflicts of Interest: G Giusti: consultant for Coloplast, Rocamed, Olympus, Lumenis, Boston Scientific, BD-Bard, Cook Medical, Quanta System; S Proietti: consultant for Quanta System; B Eisner: consultant for Boston Scientific, Olympus, Kalera Medical, Sonomotion. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol 1976;10:257-9. [Crossref] [PubMed]
- Valdivia Uría JG, Lachares Santamaría E, Villarroya Rodríguez S, et al. Percutaneous nephrolithectomy: simplified technic (preliminary report). Arch Esp Urol 1987;40:177-80. [PubMed]
- Valdivia JG, Valer J, Villarroya S. Why is Percutaneous Nephroscopy Still Performed with the Patient Prone?* J Endourol 1990;4:269-77. [Crossref]
- Hopper KD, Sherman JL, Luethke JM, et al. The retrorenal colon in the supine and prone patient. Radiology 1987;162:443-6. [Crossref] [PubMed]
- Valdivia JG, Scarpa RM, Duvdevani M, et al. Supine versus prone position during percutaneous nephrolithotomy: a report from the clinical research office of the endourological society percutaneous nephrolithotomy global study. J Endourol 2011;25:1619-25. [Crossref] [PubMed]
- Kerbl K, Clayman RV, Chandhoke PS, et al. Percutaneous stone removal with the patient in a flank position. J Urol 1994;151:686-8. [Crossref] [PubMed]
- Falahatkar S, Moghaddam AA, Salehi M, et al. Complete supine percutaneous nephrolithotripsy comparison with the prone standard technique. J Endourol 2008;22:2513-7. [Crossref] [PubMed]
- Ibarluzea G, Scoffone CM, Cracco CM, et al. Supine Valdivia and modified lithotomy position for simultaneous anterograde and retrograde endourological access. BJU Int 2007;100:233-6. [Crossref] [PubMed]
- Papatsoris AG, Zaman F, Panah A, et al. Simultaneous anterograde and retrograde endourologic access: "the Barts technique J Endourol 2008;22:2665-6. [Crossref] [PubMed]
- Bach C, Goyal A, Kumar P, et al. The Barts 'flank-free' modified supine position for percutaneous nephrolithotomy. Urol Int 2012;89:365-8. [Crossref] [PubMed]
- Hoznek A, Rode J, Ouzaid I, et al. Modified supine percutaneous nephrolithotomy for large kidney and ureteral stones: technique and results. Eur Urol 2012;61:164-70. [Crossref] [PubMed]
- Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth 2008;100:165-83. [Crossref] [PubMed]
- Manohar T, Jain P, Desai M. Supine percutaneous nephrolithotomy: Effective approach to high-risk and morbidly obese patients. J Endourol 2007;21:44-9. [Crossref] [PubMed]
- Khoshrang H, Falahatkar S, Ilat S, et al. Comparative study of hemodynamics electrolyte and metabolic changes during prone and complete supine percutaneous nephrolithotomy. Nephrourol Mon 2012;4:622-8. [Crossref] [PubMed]
- Baard J, Kamphuis GM, Westendarp M, et al. How well tolerated is supine percutaneous nephrolithotomy? Curr Opin Urol 2014;24:184-8. [Crossref] [PubMed]
- Atkinson CJ, Turney BW, Noble JG, et al. Supine vs prone percutaneous nephrolithotomy: an anaesthetist's view. BJU Int 2011;108:306-8. [Crossref] [PubMed]
- Cracco CM, Scoffone CM. ECIRS (Endoscopic Combined Intrarenal Surgery) in the Galdakao-modified supine Valdivia position: a new life for percutaneous surgery? World J Urol 2011;29:821-7. [Crossref] [PubMed]
- Mazzucchi E, Vicentini FC, Marchini GS, et al. Percutaneous nephrolithotomy in obese patients: comparison between the prone and total supine position. J Endourol 2012;26:1437-42. [Crossref] [PubMed]
- De Sio M, Autorino R, Quarto G, et al. Modified supine versus prone position in percutaneous nephrolithotomy for renal stones treatable with a single percutaneous access: a prospective randomized trial. Eur Urol 2008;54:196-202. [Crossref] [PubMed]
- Liu L, Zheng S, Xu Y, et al. Systematic review and meta-analysis of percutaneous nephrolithotomy for patients in the supine versus prone position. J Endourol 2010;24:1941-6. [Crossref] [PubMed]
- Negrete-Pulido OR, Gutirrez-Aceves J. Antibiotic prophylaxis and infections complications in PNL. In: Scoffone CM, Hoznek A, Cracco CM. editors. Supine percutaneous nephrolithotomy and ECIRS. France: Springer, 2014:279-92.
- Scoffone CM, Cracco CM, Cossu M, et al. Endoscopic combined intrarenal surgery in Galdakao-modified supine Valdivia position: a new standard for percutaneous nephrolithotomy? Eur Urol 2008;54:1393-403. [Crossref] [PubMed]
- Grasso M, Nord R, Bagley DH. Prone split leg and flank roll positioning: simultaneous antegrade and retrograde access to the upper urinary tract. J Endourol 1993;7:307-10. [Crossref] [PubMed]
- Proietti S, Sortino G, Giannantoni A, et al. Single-session supine bilateral percutaneous nephrolithotomy. Urology 2015;85:304-9. [Crossref] [PubMed]
- Proietti S, de la Rosette J, Eisner B, et al. Bilateral endoscopic surgery for renal stones: a systematic review of the literature. Minerva Urol Nefrol 2017;69:432-45. [PubMed]
- Giusti G, Proietti S, Rodríguez-Socarrás ME, et al. Simultaneous Bilateral Endoscopic Surgery (SBES) for Patients with Bilateral Upper Tract Urolithiasis: Technique and Outcomes. Eur Urol 2018;74:810-5. [Crossref] [PubMed]
- Sofer M, Giusti G, Proietti S, et al. Upper Calyx Approachability through a Lower Calyx Access for Prone Versus Supine Percutaneous Nephrolithotomy. J Urol 2016;195:377-82. [Crossref] [PubMed]
- Altschuler J, Jain R, Ganesan V, et al. Supracostal Upper Pole Endoscopic-Guided Prone Tubeless "Maxi-Percutaneous Nephrolithotomy": A Contemporary Evaluation of Complications. J Endourol 2019;33:274-8. [Crossref] [PubMed]
- Duty B, Waingankar N, Okhunov Z, et al. Anatomical variation between the prone, supine, and supine oblique positions on computed tomography: implications for percutaneous nephrolithotomy access. Urology 2012;79:67-71. [Crossref] [PubMed]
- Yazici CM, Kayhan A, Dogan C. Supine or prone percutaneous nephrolithotomy: do anatomical changes make it worse? J Endourol 2014;28:10-6. [Crossref] [PubMed]
- Assimos D, Krambeck A, Miller NL. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART II. J Urol 2016;196:1161-9. [Crossref] [PubMed]
- Miller NL, Matlaga BR, Lingeman JE. Techniques for fluoroscopic percutaneous renal access. J Urol 2007;178:15-23. [Crossref] [PubMed]
- Hudnall M, Usawachintachit M, Metzler I, et al. Ultrasound Guidance Reduces Percutaneous Nephrolithotomy Cost Compared to Fluoroscopy. Urology 2017;103:52-8. [Crossref] [PubMed]
- Usawachintachit M, Tzou DT, Hu W, et al. X-ray-free Ultrasound-guided Percutaneous Nephrolithotomy: How to Select the Right Patient? Urology 2017;100:38-44. [Crossref] [PubMed]
- Al-Dessoukey AA, Moussa AS, Abdelbary AM, et al. Percutaneous nephrolithotomy in the oblique supine lithotomy position and prone position: a comparative study. J Endourol 2014;28:1058-63. [Crossref] [PubMed]
- Karami H, Mohammadi R, Lotfi B. A study on comparative outcomes of percutaneous nephrolithotomy in prone, supine, and flank positions. World J Urol 2013;31:1225-30. [Crossref] [PubMed]
- Sofer M, Tavdi E, Levi O, et al. Implementation of supine percutaneous nephrolithotomy: a novel position for an old operation. Cent European J Urol 2017;70:60-5. [PubMed]