
Studying the impact of comorbidity on post radical cystectomy survival: have we come a full circle?
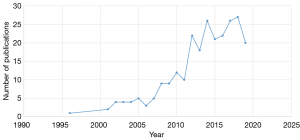
The importance of comorbidity on the survival outcomes of any major surgery cannot be understated. Furthermore, the impact of one or more significant medical comorbidities on an inherently morbid procedure such as radical cystectomy is all but obvious. The current flourish of adjuvant and neo-adjuvant treatment modalities in the treatment of localized as well as advanced bladder cancer (1), following decades of silence, has led us to wonder how to better optimize an index patient for surgery. Consequently, the increase in the armamentarium against bladder cancer has made us explore equivalent alternatives to cystectomy (2). These are only some factors that have continued to fuel our interest in better categorizing patients prior to surgery for bladder cancer. The implications of this as a shared decision making tool are also immense (3). A PubMed search with the search strings “comorbidity AND radical cystectomy” produces an interesting scatter chart (Figure 1) and provides the evidence of our continued interest.
Over the years of this increased interest, we have seen several attempts at identifying the best suited risk assessment tool for standardizing the incorporation of comorbidities into preoperative prediction models (4-9). Investigators have tried to look at several parameters and most have tried to incorporate several already existing prognostic models for the prediction of cancer specific as well as cancer independent survival. More recently, a systematic review examined the best suited index that would aid in treatment counselling and found that the American Society of Anesthesiologists (ASA) score and the Charlson Comorbidity Index (CCI) were the most easy to use and the most widely used respectively (10). However, with over a decade of research and effort towards identifying the best-suited index, we still await the litmus test for these models-validation from prospective comparative studies. A multi-institutional prospective study from Japan found that CCI ≥2 was an independent predictor of 90 day post-operative complications including high grade complications (11). However, conclusions on survival statistics were not possible due to the small sample size.
The current study by Dell’Oglio et al. (12) also attempts to address the conundrum by proposing a combined tool that uses 2 important groups of factors in a patient undergoing radical cystectomy: comorbidities and bladder cancer manifestations. This is an extension of their prior work where they had proposed a short form (9) of the Deyo adaptation of the CCI (13). Using the SEER-Medicare database they have identified 7 comorbid conditions and 2 bladder cancer manifestations as the most accurate and parsimonious in predicting 90-day mortality following radical cystectomy in a development group. These were then validated in a separate population cohort using the same database where a combination of 6 comorbid conditions and the 2 disease manifestations fared better than either as a standalone measure or the Deyo adaptation of the CCI. The two bladder cancer manifestations that were identified were urinary tract infection (UTI) prevalence and hydronephrosis. Hydronephrosis is a well-recognized factor, which has been found to correlate well with advanced stage, lymph node involvement as well as survival after radical cystectomy (14,15). This association with survival may be stronger in patients who have a higher T stage or margin positive disease (16). UTI prevalence has perhaps not been studied or individually identified as an important prognostic marker but we do have evidence that preoperative sepsis is associated with increased incidence of post-operative complications (17).
This study uses an approach to integrate patient related factors as well as disease-induced changes in predicting survival after a major surgery. It is important to have a broader vision while attempting to prognosticate patients who are undergoing a major surgery. Survival Prediction After Radical Cystectomy (SPARC) score (8) is another prediction model which has attempted to use a similar approach but has incorporated disease specific factors such as tumor stage and nodal status along with hydronephrosis and other comorbidity related factors. The most important message to take away from here would be that comorbidity should not be the sole determinant in evaluating a patient for a major procedure that also is the standard of care. To add to this, it is important to be cognizant of the fact that the average bladder cancer patient will be older, have far more preexisting chronic comorbidities (up to 8) and will be more likely to suffer from coronary artery disease and chronic kidney disease (18). Therefore, the likelihood of encountering a patient with increased perioperative mortality risk due to the number of comorbidities is high at baseline. In this regard, performance indicators like ASA score, ECOG may have a role to play. In fact, ASA score has consistently outperformed most other indices in this regard (6,10). The simplicity and the reproducibility of the score cannot be overlooked and may be considered in addition to other prediction models.
There is also increased interest in the utilization of other measures and indices that rely on body composition and nutritional measures. Most urological guidelines have not yet highlighted the significance of cancer related malnutrition assessed by signs and symptoms of anorexia, cachexia and sarcopenia. Sarcopenia as measured by skeletal muscle index (SMI), is strongly validated to be associated with up to a twofold increased risk of cancer specific and all-cause mortality (19). This association is interestingly the highest in the lowest SMI quartile with the highest Body Mass Index (BMI) (20). The measurement of SMI is also being standardized with most measurements based on the use of axial CT scans (19). BMI lacks the specificity in characterizing the true body compositions and does not truly represent the balance between lean muscle and adipose tissue (21). The fact that sarcopenia may be a modifiable risk factor has motivated researchers to look at prehabilitation as a possible intervention is patients undergoing radical cystectomy (22). Malnutrition has an intricate relationship with cancer cachexia and sarcopenia which is brought about by a complex interaction of cancer related dietary changes exaggerated by increased expression of pro-inflammatory cytokines (19). Validated nutritional assessment tools like NRS 2002 scores have been found to correlate with higher complication rates in patients undergoing radical cystectomy (23).
Increasingly researchers are showing interest in newer approaches, which are likely to have impact on post-operative mortality. Frailty is being assessed with several indices (24) and the domain is now extending to the assessment of cognitive frailty as being an important predictor of surgical outcomes (19). Comprehensive geriatric assessment (CGA) is also being recognized as an important predictor of outcomes in the elderly population and has the potential of being important assessment tool in patients undergoing radical cystectomy (19) considering the fact that patients aged >60 comprise more than 2/3 of the cystectomy population (25).
The study by Dell’Oglio et al. has utilized the SEER-Medicare database, which comprises a sizeable population, to identify the most accurate and parsimonious group of comorbidities and bladder cancer manifestations and subsequently validated this construct with a large population from the same database. The use of ICD-9-CM diagnostic codes reliably captures the treatments received by the patient population and thus is more inclusive. However, the inability of this database to reliably record all relevant morbidities along with the possibility of misclassification errors can drastically limit the interpretation of results. The authors have taken extreme care and have only included patients who were enrolled in Medicare A and B for a minimum of 1 year prior to and 3 months after the surgery. They have also acknowledged the limited generalizability of the study in view of the age group that is represented by the SEER-Medicare database. The other limitation is the higher mortality rates in cohorts used. The development cohort and the validation cohort had mortality rates of 10.4% and 13.1% respectively which is considerably higher than the reported by most large studies (25). This can influence the identification of factors, which may not have been seen in previous studies. For example, UTI with a high prevalence of 60% in the development cohort was found to be an important predictor while most prior studies have not recognized this as an important preoperative factor influencing mortality (17). The accuracy of this comprehensive index is fair (71.1%). Although the authors have demonstrated that it was better than the CCI (71.1% vs. 68%), comparative statistics between the indices have not been provided. Therefore, the question of a broader applicability of this index is limited.
In summary, while re-examining the scatter plot (Figure 1), there is an important question that we need to ask ourselves. After a decade long search and over 100 publications later, do we have the silver bullet now? The answer we feel is not a simple yes or no. We have indeed come a long way. We are now better equipped to understand post cystectomy survival than a decade ago. Treatment of bladder cancer has evolved to a great extent and we may be at a turning point in the history of cancer care with the continued advent of new therapies. The elements to be considered in comprehensive assessment of disease status and patient condition and their interplay in predicting immediate post cystectomy outcome is becoming clearer.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Boegemann M, Aydin AM, Bagrodia A, et al. Prospects and progress of immunotherapy for bladder cancer. Expert Opin Biol Ther 2017;17:1417-31. [PubMed]
- Williams SB, Huo J, Chamie K, et al. Underutilization of Radical Cystectomy Among Patients Diagnosed with Clinical Stage T2 Muscle-invasive Bladder Cancer. Eur Urol Focus 2017;3:258-64. [Crossref] [PubMed]
- Williams SB, Huo J, Chu Y, et al. Cancer and All-cause Mortality in Bladder Cancer Patients Undergoing Radical Cystectomy: Development and Validation of a Nomogram for Treatment Decision-making. Urology 2017;110:76-83. [Crossref] [PubMed]
- Boorjian SA, Kim SP, Tollefson MK, et al. Comparative performance of comorbidity indices for estimating perioperative and 5-year all cause mortality following radical cystectomy for bladder cancer. J Urol 2013;190:55-60. [Crossref] [PubMed]
- Meng X, Press B, Renson A, et al. Discriminative Ability of Commonly Used Indexes to Predict Adverse Outcomes After Radical Cystectomy: Comparison of Demographic Data, American Society of Anesthesiologists, Modified Charlson Comorbidity Index, and Modified Frailty Index. Clin Genitourin Cancer 2018;16:e843-50. [Crossref] [PubMed]
- Mayr R, May M, Martini T, et al. Comorbidity and performance indices as predictors of cancer-independent mortality but not of cancer-specific mortality after radical cystectomy for urothelial carcinoma of the bladder. Eur Urol 2012;62:662-70. [Crossref] [PubMed]
- Froehner M, Koch R, Novotny V, et al. Lee mortality index as comorbidity measure in patients undergoing radical cystectomy. Springerplus 2015;4:55. [Crossref] [PubMed]
- Eisenberg MS, Boorjian SA, Cheville JC, et al. The SPARC score: A multifactorial outcome prediction model for patients undergoing radical cystectomy for bladder cancer. J Urol 2013;190:2005-10. [Crossref] [PubMed]
- Dell'Oglio P, Tian Z, Leyh-Bannurah SR, et al. Short-Form Charlson Comorbidity Index for Assessment of Perioperative Mortality After Radical Cystectomy. J Natl Compr Canc Netw 2017;15:327-33. [Crossref] [PubMed]
- Williams SB, Kamat AM, Chamie K, et al. Systematic Review of Comorbidity and Competing-risks Assessments for Bladder Cancer Patients. Eur Urol Oncol 2018;1:91-100. [Crossref] [PubMed]
- Hirobe M, Tanaka T, Shindo T, et al. Complications within 90 days after radical cystectomy for bladder cancer: results of a multicenter prospective study in Japan. Int J Clin Oncol 2018;23:734-41. [Crossref] [PubMed]
- Dell'Oglio P, Tian Z, Leyh-Bannurah SR, et al. Development of a New Comorbidity Assessment Tool for Specific Prediction of Perioperative Mortality in Contemporary Patients Treated with Radical Cystectomy. Ann Surg Oncol 2019;26:1942-9. [Crossref] [PubMed]
- Deyo RA, Cherkin AC, Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. J Clin Epidemiol 1992;45:613-9. [Crossref] [PubMed]
- Bartsch GC, Kuefer R, Gschwend JE, et al. Hydronephrosis as a Prognostic Marker in Bladder Cancer in a Cystectomy-Only Series. Eur Urol 2007;51:690-7. [Crossref] [PubMed]
- Oh JJ, Byun SS, Jeong CW, et al. Association Between Preoperative Hydronephrosis and Prognosis After Radical Cystectomy Among Patients With Bladder Cancer: A Systemic Review and Meta-Analysis. Front Oncol 2019;9:158. [Crossref] [PubMed]
- Chapman DM, Pohar KS, Gong MC, et al. Preoperative hydronephrosis as an indicator of survival after radical cystectomy. Urol Oncol 2009;27:491-5. [Crossref] [PubMed]
- Lavallée LT, Schramm D, Witiuk K, et al. Peri-operative morbidity associated with radical cystectomy in a multicenter database of community and academic hospitals. PLoS One 2014;9:e111281. [Crossref] [PubMed]
- Garg T, Young AJ, Kost KA, et al. Burden of Multiple Chronic Conditions among Patients with Urological Cancer. J Urol 2018;199:543-50. [Crossref] [PubMed]
- Psutka SP, Barocas DA, Catto JWF, et al. Staging the Host : Personalizing Risk Assessment for Radical Cystectomy Patients. Eur Urol Oncol 2018;1:292-304. [Crossref] [PubMed]
- Wan F, Zhu Y, Gu C, et al. Lower skeletal muscle index and early complications in patients undergoing radical cystectomy for bladder cancer. World J Surg Oncol 2014;12:14. [Crossref] [PubMed]
- Psutka SP, Boorjian SA, Moynagh MR, et al. Mortality after radical cystectomy: Impact of obesity versus adiposity after adjusting for skeletal muscle wasting. J Urol 2015;193:1507-13. [Crossref] [PubMed]
- Jensen BT, Laustsen S, Jensen JB, et al. Exercise-based pre-habilitation is feasible and effective in radical cystectomy pathways—secondary results from a randomized controlled trial. Support Care Cancer 2016;24:3325-31. [Crossref] [PubMed]
- Karl A, Staehler M, Bauer R, et al. Malnutrition and clinical outcome in urological patients. Eur J Med Res 2011;16:469. [Crossref] [PubMed]
- Burg ML, Clifford TG, Bazargani ST, et al. Frailty as a predictor of complications after radical cystectomy: A prospective study of various preoperative assessments. Urol Oncol 2019;37:40-7. [Crossref] [PubMed]
- Nielsen ME, Mallin K, Weaver MA, et al. Association of hospital volume with conditional 90-day mortality after cystectomy: An analysis of the National Cancer Data Base. BJU Int 2014;114:46-55. [Crossref] [PubMed]


