Looking into the clinical application of CD47-targeted near-infrared photoimmunotherapy for human bladder cancer treatment
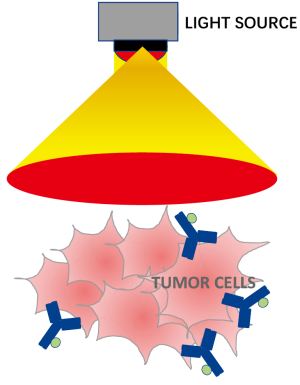
A recently published paper by a Stanford research team led by Dr. Joseph C. Liao in Clinical Cancer Research (1) reported on their well-designed study demonstrating the potential application of CD47-targeted near-infrared photoimmunotherapy (NIR-PIT) for human bladder cancer (BC) (Figure 1).
CD47, also known as an integrin-associated protein, is a cell surface transmembrane protein that plays a role in neutrophil migration and T-cell co-stimulation. In the context of BC, high expression levels of CD47 have been observed in BC tumor cells (in both non-muscle invasive and muscle invasive BC). However, expression was found to be absent in terminally differentiated luminal umbrella cells of the normal bladder epithelium. Thus, blocking CD47 may enable our immune system to selectively recognize BC cells, leading to the hypothesis that targeting CD47 may be the potential strategy for specifically killing cancer cells while avoiding unnecessary harm to normal bladder cells. In this paper, the authors elegantly performed a series of in vitro experiments using well-characterized BC cell lines. Their in vivo experiments used human specimens, which successfully showed that anti-CD47-IR700 may play as a molecular photosensitizer for NIR-PIT of BC. Further experimental results using a xenograft mouse model suggested that CD47-targeted NIR-PIT may effectively block BC growth.
Phototherapy, also known as light therapy, utilizes specific wavelengths of light to treat medical conditions. The inception of this idea began in the late 19th century by Ryberg Finsen, who developed phototherapy for the treatment of lupus vulgaris, a type of skin condition (2). Since then, phototherapy has been adapted and modified into various forms, such as photoimmunological, photochemical, and photodynamic therapies (3). These different phototherapies have become incredibly advantageous when it comes to treating cancer. They have diversified treatment options and are versatile enough to be combined with other therapies. For instance, photoimmunotherapy (PIT) has been shown to increase nano-drug uptake 24-fold in tumor tissues compared to normal (4). Photodynamic therapy (PDT) has been demonstrated to successfully destroy tumor cells, which leads to stimulation of anti-tumor immunity and generation of an innate immune response (5). Because treatment options for BC are mainly limited to surgery and chemotherapy, utilization of these phototherapies are of particular interest.
Unfortunately, when it comes to BC, PDT has largely been abandoned. Clinical trials of PDT lead to several noted adverse events that ultimately demonstrated toxicity and bystander effects on normal bladder cells (6). Another potential challenge of using PDT in BC is the hypoxic microenvironment in BC tissues, which limits the needed O2 supply for creating reactive oxygen species and eventual cell death (7,8). There have been some studies that have addressed the issue of hypoxia and demonstrated potential reintroduction of PDT in BC, but clinical application remains far ahead (9). On the other hand, PIT has had promising results and is being further explored as a viable treatment option. Studies have demonstrated highly-selective targeting of BC cells by conjugating a photoabsorber dye with panitumumab, an anti-EGFR antibody (10). This strategy takes advantage of the fact that EGFR is overexpressed in BC tissue, with relatively low expression in normal bladder urothelial cells (11,12). A recent study took this a step further by targeting HER2 along with EGFR, which would allow for more effective apoptosis of BC cells across different tumor phenotypes (13).
Collectively, these promising findings by this research team was able to provide persuasive evidence that CD47-targeted NIR-PIT can be deployed endoscopically and holds the potential to augment treatment of localized BC. NIR-PIT, a localized molecular cancer therapy combining a photosensitizer-conjugated monoclonal antibody and light energy, is a particularly attractive tool to use in the urinary tract due to ease of access. One major and important concern is related to safety and therapeutic efficacy. Since it is currently being investigated in other clinical trials for hematopoietic and solid cancers (ClinicalTrials.gov NCT02216409), I believe that we will have better idea how CD47-targeted NIR-PIT therapy can be used as a potential standard option of treatment against BC in the real clinical setting soon.
Acknowledgments
The author would like to thank Mr. Austin Yeon for careful review and editing the manuscript.
Funding: The author acknowledges support from National Institutes of Health grants (1U01DK103260), Department of Defense grants (W81XWH-15-1-0415 and W81XWH-19-1-0109), Centers for Disease Control and Prevention (1U01DP006079), the Steven Spielberg Discovery Fund in Prostate Cancer Research Career Development Award, the U.S.-Egypt Science and Technology Development Fund by the National Academies of Sciences, Engineering, and Medicine, Burroughs Wellcome Fund (BWF) 2017 Collaborative Research Travel Grant (CRTG), and Southeast Center for Integrated Metabolomics (SECIM) Pilot and Feasibility Grant (to J Kim).
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Kiss B, van den Berg NS, Ertsey R, et al. CD47-Targeted Near-infrared Photoimmunotherapy for Human Bladder Cancer. Clin Clin Cancer Res 2019;25:3561-71. [Crossref] [PubMed]
- Grzybowski A, Pietrzak K. From patient to discoverer--Niels Ryberg Finsen (1860-1904) --the founder of phototherapy in dermatology. Clin Dermatol 2012;30:451-5. [Crossref] [PubMed]
- Li Y, Li X, Zhou F, et al. Nanotechnology-based photoimmunological therapies for cancer. Cancer Lett 2019;442:429-38. [Crossref] [PubMed]
- Kobayashi H, Choyke PL. Super enhanced permeability and retention (SUPR) effects in tumors following near infrared photoimmunotherapy. Nanoscale 2016;8:12504-9. [Crossref] [PubMed]
- Mroz P, Hashmi JT, Huang YY, et al. Stimulation of anti-tumor immunity by photodynamic therapy. Expert Rev Clin Immunol 2011;7:75-91. [Crossref] [PubMed]
- Railkar R, Agarwal PK. Photodynamic Therapy in the Treatment of Bladder Cancer: Past Challenges and Current Innovations. Eur Urol Focus 2018;4:509-11. [Crossref] [PubMed]
- Blick C, Ramachandran A, Wigfield S, et al. Hypoxia regulates FGFR3 expression via HIF-1alpha and miR-100 and contributes to cell survival in non-muscle invasive bladder cancer. Br J Cancer 2013;109:50-9. [Crossref] [PubMed]
- Hunter BA, Eustace A, Irlam JJ, et al. Expression of hypoxia-inducible factor-1alpha predicts benefit from hypoxia modification in invasive bladder cancer. Br J Cancer 2014;111:437-43. [Crossref] [PubMed]
- Lin T, Zhao X, Zhao S, et al. O2-generating MnO2 nanoparticles for enhanced photodynamic therapy of bladder cancer by ameliorating hypoxia. Theranostics 2018;8:990-1004. [Crossref] [PubMed]
- Railkar R, Krane LS, Li QQ, et al. Epidermal Growth Factor Receptor (EGFR)-targeted Photoimmunotherapy (PIT) for the Treatment of EGFR-expressing Bladder Cancer. Mol Cancer Ther 2017;16:2201-14. [Crossref] [PubMed]
- Chaux A, Cohen JS, Schultz L, et al. High epidermal growth factor receptor immunohistochemical expression in urothelial carcinoma of the bladder is not associated with EGFR mutations in exons 19 and 21: a study using formalin-fixed, paraffin-embedded archival tissues. Hum Pathol 2012;43:1590-5. [Crossref] [PubMed]
- Rotterud R, Nesland JM, Berner A, et al. Expression of the epidermal growth factor receptor family in normal and malignant urothelium. BJU Int 2005;95:1344-50. [Crossref] [PubMed]
- Siddiqui MR, Railkar R, Sanford T, et al. Targeting Epidermal Growth Factor Receptor (EGFR) and Human Epidermal Growth Factor Receptor 2 (HER2) Expressing Bladder Cancer Using Combination Photoimmunotherapy (PIT). Sci Rep 2019;9:2084. [Crossref] [PubMed]