
Method of alkalization and monitoring of urinary pH for prevention of recurrent uric acid urolithiasis: a systematic review
Introduction
Urolithiasis is a common urologic condition with a wide geographic variation of prevalence worldwide; 7–13% in North America, 5–9% in Europe and 1–5% in Asia (1), and recurrence rate up to 50% in five years (2). The risk of recurrence depends on the stone composition and is based on an underlying cause. Uric acid (UA) stones are considered to have a high risk of recurrence (3). In the United States the frequency of UA stones lies around 10% of all stones (4). Trinchieri and Montanari estimated the UA stone prevalence of more than 1% in the US, 0.4–0.7% in Europe and varying in Asia between 0.2% in northern India and 3.0% in Thailand (5).
There are three main components related to UA urolithiasis formation; low urinary pH (i.e., of ≤5.5), low urinary volume and hyperuricosuria. The solubility of UA in urine is determined by the acidity of the urine. With a logarithmic acid dissociation constant (pKa) of 5.53 (6) a low urine pH of ≤5.5 leads to a higher concentration of insoluble UA supersaturation of UA. Siener and Hesse described supersaturation as a function of urinary UA concentration and urinary pH (7). This explains that at a low pH even a small amount of UA can lead to crystal formation and that increasing the pH allows a large amount of UA in the form of the soluble urate to be present in the urine without risk of stone forming (8-10).
As is expected, patients with UA stones commonly have a lower urinary pH than other stone-type or non-stone formers (11). Furthermore UA urolithiasis is found to be more common in people with diabetes mellitus type II (12), disorders seen in the metabolic syndrome, high BMI and chronic diarrhea with bicarbonate loss resulting from bowel surgery or inflammatory bowel disease (13).The metaphylaxis, or recurrence prevention focuses on the three main components of UA stone formation; increase of urinary volume, prevention of hyperuricosuria and increase of urinary pH. By increasing daily fluid intake the urinary volume increases thereby decreasing the concentration of UA (14). The association between high protein diets and increasing urinary risk factors for UA stones has been demonstrated (7,15). This has led to the introduction of dietary advice as part of the prevention of UA urolithiasis recurrence.The effect of urine pH on the formation of UA urolithiasis forms the basis of alkalizing therapy. The risk of UA crystal formation is highest at a urine pH ≤5.5 due to supersaturation of UA. Following this principle we know that raising the urine pH to ≥6.0 UA stone formation can be halted and even dissolved (9). Medication, usually potassium citrate (KCit), sodium citrate (NaCit) or sodium bicarbonate (NaHCO3) can be used to increase the urinary pH (16) and decrease the risk of supersaturation and thereby stone recurrences.In our search for a good treatment and follow up protocol for our UA patients we found that, despite the fact that these therapeutic options have been known for some time (17), there is relatively scarce evidence in the literature. Therefore, a systematic review of available literature concerning the methods and effect of metaphylaxis of UA urolithiasis was conducted to evaluate the evidence on the method, follow up and efficacy of this treatment modality.
Methods
The objective of this review was to assess literature on the methods of metaphylactic therapy using oral alkalization of UA urolithiasis and to critically evaluate the evidence provided. The review was based and written accordingly to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (18). We planned to do a quantitative analysis of included studies if deemed possible, otherwise the results would be presented as a narrative review.
Search strategy
A literature search was conducted in August 2018, performed independently by two authors (JW van Hattum and GM Kamphuis), using seven different databases; MEDLINE (PubMed), Embase (Ovid), TRIP, the Cochrane library, National guideline clearinghouse, clinicaltrials.gov and CINAHL. Search terms used, in combination with Boolean operators (AND, OR), were “urolithiasis/nephrolithiasis/(kidney) stones”, “uric acid/urinary pH/acidity”, “therapy/prevention/secondary prevention” and “recurrence” from inception of databases to August 2018. Additionally, high regarded international guidelines on urolithiasis were studied [the European Association of Urology (EAU), American Urology Association (AUA)].
Inclusion criteria
- Articles, written in English or German considering ways of medical metaphylaxis of UA urolithiasis and control of urine pH.
- Studies carried out in humans.
Exclusion criteria
- Studies only discussing surgical or dissolution therapy.
- Animal studies, laboratory studies and review articles.
Outcomes of interest were method of alkalizing therapy (description of medication and dosage), method of urine-pH control, recurrence rate, diagnostic tools used to determine recurrence during follow-up and patient compliance. Cross references of included studies were performed to identify further relevant evidence.
Risk of bias assessment
After inclusion the risk of bias of individual studies was determined using the Cochrane collaboration tool for assessing the risk of bias (19). To address external validity of studies the differences in treatment and follow-up between studies were compared.
Results
Included clinical studies
After removing duplicates and subsequently screening on title, abstract and full-text by two authors a total of 12 articles were included in the final review (see Figure 1). A summary of the articles is given in Table 1. Three studies consisted only in the form of congress abstracts and were not available as full-text articles. Only one study randomly dived patients into different treatment groups (31). The other 11 studies consisted of non-randomized studies (20-30). We focused on the risk of selection bias, the presence of a comparison group and the risk of selective reporting due to exclusion or attrition.

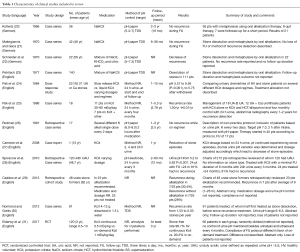
Full table
We evaluated the reported outcome, the method of alkalization, the method of pH measurement and the result of alkalization. Most studies were based on case-series without a comparison group. Upon reviewing the obtained evidence it was concluded that due to small sample sizes (number of patients varying between one and 140), variable methodology and reported outcomes, a quantitative analysis was not possible. Therefore, the analysis of literature resulted in a narrative review.
Reported outcome
Of the 12 included studies, one focuses on fluctuations in urine chemistries under different types and dosages of medication (31). This study was included in the review because it delivers important evidence for alkalization as a treatment modality which is applied in the other included studies. Five studies considered stone recurrence as primary outcome (25,26,28,29,31). Three of these reported either a decrease in stone recurrence rate or no recurrences at all during follow-up. One study (29), which only states if alkalization was suggested but does not discuss the actual compliance, reports no significant difference in stone recurrence between the alkalization therapy group (30.4%) and the control group (28%) during follow-up. Elderwy and colleagues (31) report a stone-free rate of 96.7% and 93.3% in the continuous group and on-demand treatment group respectively. It also reports a difference in compliance towards the follow-up protocol in favor of the on-demand treatment group. No further explanation about the regimen of continuous or on-demand alkalization is given. Six studies considered both stone dissolution in active stone disease and stone recurrence prevention (20-23,27,30).
Method of alkalization
All included studies but one described the medication used for alkalization therapy (24). The type of medication varied between studies. In six studies Potassium Citrate (KCit) was the drug of choice (24,25,27,28,30,31) whereas in four others a mixture of sodium-potassium citrate (NaKCit) was used (20-23). Rodman (26) describes using different potassium salts and if necessary adding sodium bicarbonate. Based on the urinalysis of 24 h urine, Sakhaee and colleagues favor KCit above alkali containing sodium because of the possible advantage of decreasing the chance of calcium stone formation (11).
Method of pH measurement
All studies, with exception of Normand (30) and Elderwy (31), describe the measurement of urine pH as guidance for medication dosages. The method of urine pH measurements with the use of pH-paper was done in five studies (20-23,26), in one study the pH was measured using a pH electrode (23), while the remaining studies did not disclose the method of pH determination (24,25,27,29). Six studies describe measurement of the pH in freshly voided urine samples (20-23,26,28) while three used pooled 24-hour urine (24,25,27). The case report by Cameron et al. (27) describes a circadian fluctuation of urine pH. This suggests that 24 h collections might not be ideal for follow-up in the treatment of UA urolithiasis. Other papers by Kollwitz (20), Makrigiannis (21) and Schneider (22) all describe a clear treatment in which pH-paper with different scales is used to monitor the urine pH by patients themselves and the dosage of alkali adjusted based on these results. Rodman (26) proposed a treatment schedule, in which patients only need a single dose every two days as long as the urine pH rises to 7.0 measured with pH-paper two hours after intake.
Results of alkalization
Three studies report positive results in terms of dissolution and prevention of stone recurrence (23,27,30). Rodman (26) found no recurrences when the treatment protocol was upheld and stated that if a stable state is reached patient could lower the frequency of measurements to once in every two weeks. Pak (25) and Spivacow (28) based the medication dosages on pooled 24 hour urine every three or four months at the outpatient clinic and both reached a significant decrease in stone recurrence rate. Elderwy (31) reports high stone free rats in both treatment groups with only six patients with recurrences, five of which were dissolved by alkalization.
The risk of bias
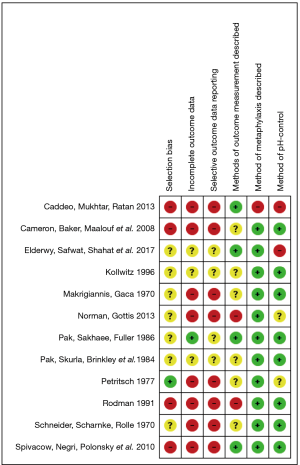
The risk of bias was assessed using the Cochrane collaboration tool (19). In general, the risk of bias was unclear or high. Most studies were retrospective case series with chance of selection bias, follow up bias and heterogeneity in outcome measures. The only study which randomly assigned patients in treatment groups (31) did not discuss the method of randomization. We summarize the risk of bias is in Figure 2.
Discussion
The principle of metaphylaxis of UA urolithiasis by oral alkalization therapy is standard treatment and included in AUA (32) and EAU (33) guidelines. In this review we find that there is limited evidence on how to apply alkalization therapy in both method and measurement on the effect on urinary pH level. Only one randomized study was identified compared to 11 non-randomized studies which inherently leads to a high risk of bias and limited external validity.
Urine collection: 24 hours urine or periodic measurements
There are two different collection conditions mentioned throughout the different studies. This could have significant impact on the outcome of the measurement. In the case of 24 hr urine collections, the pH is prone to alkalization in time, due to bacterial growths and formation of ammonia from the breakdown of urea, especially if the right storage and preservation conditions are not met (34). One study by Kessler and Hesse (35) mentioned the use of preserving agents and cold storage during the collection period, while the other studies have not commented on this matter. Also the timing of collection can have an influence on the result, e.g., in relation to the time of medication, and in light of the circadian rhythm as mentioned in the report of Cameron et al. (27).
Periodic measurements direct after urinating seems to be favourable, but no evidence exists on the number of times a day, or days a week.
Measurement of urinary pH: pH paper or electronic pH measurement
There seems to be considerable variation in the methods used to monitor the treatment. Although most studies use periodic measurements of urine pH, there is no uniformity in measurement intervals, the collection conditions and method of analysis. Generally, it can be stated that potentiometric determination of the urine pH allows for greater accuracy than the use of indicator paper. One could argue that the higher resolution that is obtainable with a potentiometric pH meter might not be of relevance in the treatment of UA urolithiasis, but there is no clear evidence for this. Evaluation of urinary pH with pH paper could however lead to errors in follow up, due to problems with interpretation of color changes of the paper. This could be particularly the case when the determination of the pH is done by the patient and not by trained laboratory technicians. Recently developments have been made towards the implementation of electronic pH measuring devices. De Coninck (36) evaluated the use and accuracy of a portable electronic device compared to reagent strips and Omar (37) compared the use of such a device during dissolution therapy with reagent strips.
Type of medical intervention with dosage and frequency
The type of medication used is in general Sodium citrate or Potassium citrate or a combination of both. The choice of medication is probably in general decided on local custom and preferences. No comparison studies have been done on effect, efficacy or patient experience. Also, the administration of the medication varies widely, from daily once to several times up to periodically usage.
Area of future research
Urologist worldwide use alkalization of urine for the metaphylaxis of UA urolithiasis. In our experience, a proportion of UA urolithiasis patients still have frequent recurrences. The question rose whether or not we were using the right medication, administration regime for usage or pH measurement tools. Our review shows the lack of unbiased evidence for this general applicable method in decreasing UA stone recurrence rates. There is a long history of papers on UA urolithiasis and the possible treatment of alkalization, however, the quality of evidence is debatable. In both the AUA (32) and EAU (33) guidelines alkalization is recommended. However, no explanation on the exact way to do so, or follow-up or effectiveness are discussed or commented upon. As is shown in this review the recommendations for alkalizing urine in the urological daily practice are based on non-randomized trials containing different methods.
Conclusions
There is clear advice on prevention of UA stones in patients with recurrent urolithiasis by alkalinization of urine. But guidance on how this should be done including the type, dosage and duration is still lacking. The evidence on the method of metaphylaxis for UA urolithiasis by alkalization of urine through oral alkalization therapy and pH measurement and follow up is limited. The studies published on this topic are scarce and contain notable risks of bias which should be kept in mind when interpreting the stated results.
Acknowledgements
Miss F. S. van Etten-Jamaludin, Clinical librarian of the AMC for her help with building a search strategy used for the review of literature.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sorokin I, Mamoulakis C, Miyazawa K, et al. Epidemiology of stone disease across the world. World J Urol 2017;35:1301-20. [Crossref] [PubMed]
- Keoghane S, Walmsley B, Hodgson D. The natural history of untreated renal tract calculi. BJU Int 2010;105:1627-9. [Crossref] [PubMed]
- Hesse A, Tiselius HG, Siener R, et al. Urinary Stones, Diagnosis, Treatment and Prevention of Recurrence. 3rd editio. Basel: Karger, 2009.
- Moses R, Pais VM, Ursiny M, et al. Changes in stone composition over two decades: evaluation of over 10,000 stone analyses. Urolithiasis 2015;43:135-9. [Crossref] [PubMed]
- Trinchieri A, Montanari E. Prevalence of renal uric acid stones in the adult. Urolithiasis 2017;45:553-62. [Crossref] [PubMed]
- Smith RC, Gore JZ. The First Dissociation Constant of Uric Acid. Microchem J 1988;38:118-24. [Crossref]
- Siener R, Hesse A. The effect of a vegetarian and different omnivorous diets on urinary risk factors for uric acid stone formation. Eur J Nutr 2003;42:332-7. [Crossref] [PubMed]
- Maalouf NM, Cameron MA, Moe OW, et al. Novel insights into the pathogenesis of uric acid nephrolithiasis. Curr Opin Nephrol Hypertens 2004;13:181-9. [Crossref] [PubMed]
- Asplin JR. Uric acid stones. Semin Nephrol 1996;16:412-24. [PubMed]
- Mehta TH, Goldfarb DS. Uric Acid Stones and Hyperuricosuria. Adv Chronic Kidney Dis 2012;19:413-8. [Crossref] [PubMed]
- Sakhaee K, Adams-Huet B, Moe OW, et al. Pathophysiologic basis for normouricosuric uric acid nephrolithiasis. Kidney Int 2002;62:971-9. [Crossref] [PubMed]
- Daudon M. Type 2 Diabetes Increases the Risk for Uric Acid Stones. J Am Soc Nephrol 2006;17:2026-33. [Crossref] [PubMed]
- Kenny JES, Goldfarb DS. Update on the pathophysiology and management of uric acid renal stones. Curr Rheumatol Rep 2010;12:125-9. [Crossref] [PubMed]
- Gutman AB, Yu T. Uric acid nephrolithiasis. Am J Med 1968;45:756-79. [Crossref] [PubMed]
- Siener R, Hesse A. Comparison of the effect of variations in dietary purine on risk of uric acid stone formation. Am J Clin Nutr 1999;70:630-2.
- Sakhaee K, Nicar M, Hill K, et al. Contrasting effects of potassium citrate and sodium citrate therapies on urinary chemistries and crystallization of stone-forming salts. Kidney Int 1983;24:348-52. [Crossref] [PubMed]
- Atsmon A, Vries A, Lazebink J, et al. Uric Acid Stones Fluid by Alkalinization in a Patient Suffering from Gout. Am J Med 1959;27:167-71. [Crossref] [PubMed]
- Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [Crossref] [PubMed]
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Collab 2011.
- Kollwitz AA. Treatment and prophylaxis of uric acid stones of the kidney by oral alkalinization. Dtsch Med Wochenschr 1966;91:1257-9. [Crossref] [PubMed]
- Makrigiannis D, Gaca A. Oral dissolution and prevention of recurrences of uric-acid stones in the kidney by oral medication. Dtsch Med Wochenschr 1970;95:1383-7. [Crossref] [PubMed]
- Schneider HJ, Tscharnke J, Rolle E. Clinical experiences with the citrate granulate blemaren in the prevention and therapy of uric acid lithiasis. Z Urol Nephrol 1970;63:47-54. [PubMed]
- Petritsch PH. Uric acid calculi results of conservative treatment. Urology 1977;10:536-8. [Crossref] [PubMed]
- Pak CYC, Skurla C, Brinkley L, et al. Augmentation of renal citrate excretion by oral potassium citrate administration: Time course, dose frequency schedule, and dose-response relationship. J Clin Pharmacol 1984;24:19-26. [Crossref] [PubMed]
- Pak CY, Sakhaee K, Fuller C. Successful management of uric acid nephrolithiasis with potassium citrate. Kidney Int 1986;30:422-8. [Crossref] [PubMed]
- Rodman JS. Prophylaxis of uric acid stones with alternate day doses of alkaline potassium salts. J Urol 1991;145:97-9. [Crossref] [PubMed]
- Boari B, Salmi R, Rizzioli E, et al. Circadian variation in urine pH and uric acid nephrolithiasis risk. Nephrol Dial Transplant 2008;23:411-2. [Crossref] [PubMed]
- Spivacow FR, Negri AL, Polonsky A, et al. Long-term treatment of renal lithiasis with potassium citrate. Urology 2010;76:1346-9. [Crossref] [PubMed]
- Caddeo G, Mukhtar B, Ratan HL. Recurrence of uric acid stones in patients on oral alkalinization therapy. Eur Urol Suppl 2013;12:79. [Crossref]
- Normand M, Gottis M. Medical treatment of uric acid urolithiasis. Eur J Clin Invest 2013;43:78-9.
- Elderwy AA, Safwat A, Shahat A, et al. Metaphylaxis of uric acid nephrolithiasis in children: Continuous versus ondemand oral potassium citrate. Eur Urol Suppl 2017;16:e1274. [Crossref]
- Pearle MS, Goldfarb DS, Assimos DG, et al. Medical management of kidney stones: AUA guideline. J Urol 2014;192:316-24. [Crossref] [PubMed]
- Skolarikos A, Straub M, Knoll T, et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur Urol 2015;67:750-63. [Crossref] [PubMed]
- Cook JD, Strauss K, Caplan Y, et al. Urine pH: the effects of time and temperature after collection. J Anal Toxicol 2007;31:486-96. [Crossref] [PubMed]
- Kessler T, Hesse A. Cross-over study of the influence of bicarbonate-rich mineral water on urinary composition in comparison with sodium potassium citrate in healthy male subjects. Br J Nutr 2000;84:865-71. [Crossref] [PubMed]
- De Coninck V, Keller EX, et al. Rodríguez-Monsalve M, Evaluation of a portable urinary pH meter and reagent strips. J Endourol 2018;32:end.2018.0202.
- Omar M. Optimization of Uric Acid Dissolution Therapy By Hand Held Digital Ph Meter. J Urol 2018;199:e413. [Crossref]


