
How long does it take a man to collect his semen specimen in a busy infertility clinic?
Introduction
Approximately 8–15% of couples are unable to conceive after 1 year of unprotected intercourse. A male factor is solely responsible in ~20% of infertile couples and contributes in another 30–40% of couples (1). A diagnostic semen analysis is typically performed as part of a male infertility evaluation.
In the establishment of a male infertility evaluation practice, there are a great number of organizational details to be taken into account. One of them is the timing of semen collection, a somewhat unpredictable variable that heavily impacts the organization and scheduling of clinic visits. To our knowledge, no guidelines have been reported to aid in this essential aspect of scheduling. The purpose of this study was to determine the time required for semen collection in a busy male infertility clinic.
Methods
Setting
This study took place in the setting of a male infertility and andrology clinic which is part of the department of urology at a major medical school. The andrology laboratory performs approximately 80 semen analyses per month during five 8-hour shifts per month. The semen specimens analyzed by the lab are from the patients of physicians in the department of urology. These patients collect their semen specimens in exam rooms located in the clinic.
Design
In this prospective observational study, 10% of our patient population was sampled over a 17-month period between 2017 and 2018. Patients were not informed that semen collection times would be recorded, as this information could introduce variables that may influence semen collection times. Data were collected once per patient. Semen collection took place in multi-purpose exam rooms. These rooms were equipped with chairs, an examination bed and sink (Figure 1). Curtains were available for increased privacy (Figure 2). Graphic aid material was provided as three erotic magazines in a brown envelope left in the collection rooms. Video material was also available in a portable DVD player for patients if requested. When informed, some patients stated they brought materials in their personal cell phones.


Semen collection
The patient was shown into the exam room by the provider. The provider obtained intake information about the patient, and then gave instructions for semen collection. Patients were asked to ejaculate, using only masturbation, into a specimen cup. If the patient elected to have his female partner in the room, instructions were given to abstain from oral, anal, or vaginal sex as these practices may introduce cells from the female into the semen specimen. The patient and/or his partner were given an opportunity to ask questions. The patient was instructed to text the word “done” to a cell phone number when semen collection was complete. The provider then exited the exam room.
Data collection
Timing of semen collection was performed using a stopwatch (VWR, Radnor, PA, USA). The stopwatch was started when the provider exited the exam room and was stopped when the patient texted the word “done”. The elapsed time was recorded. The following data were also recorded: purpose of the semen collection, patient age, presence or absence of a partner in the room during semen collection. Data collected was de-identified and analyzed with no reference to human subjects. The study was granted exempt status by the Institutional Review Board.
Data analysis
Group means were compared by analysis of variance. Comparison of frequencies was performed by Chi-square.
Results
The study group consisted of 136 men. Their mean age was 35.7±7.8 years old (range, 18.8 to 62.5 years old), and their indications for semen collection were: evaluation for male factor infertility in 125 cases (92%), of which 12 (9%) underwent sperm cryopreservation of the collected specimen; post-vasectomy evaluation in 7 cases (5%); and post vasoepididymostomy in 4 cases (3%).
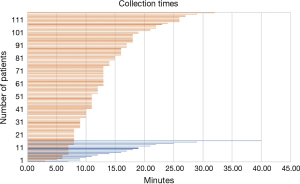
The results of semen collection times are summarized in Table 1 and Figure 3. The median collection time for all subjects was 11 minutes 57 seconds ± 9 minutes 8 seconds to 17 minutes 5 seconds, with a minimum time of 3 minutes 9 seconds, and a maximum time of 39 minutes 50 seconds. The median duration for the group of men collecting with a partner in the room (16 minutes 36 seconds) was over 4 minutes longer than the median duration for the group of men collecting without a partner in the room (12 minutes 28 seconds, P=0.009). Only one patient from this study group was unable to provide a sample, whom, of note, was accompanied by his partner.

Full table
Although the median duration for the group of men collecting for the purpose of sperm cryopreservation (14 minutes 26 seconds) was longer than the median time for the group of men collecting for purposes other than sperm cryopreservation (12 minutes 41 seconds), this difference was not statistically significant.
Interestingly, there was no statistically significant correlation between patient age and semen collection times.
Discussion
Our goal in this prospective, observational study was to determine the duration of time needed for male patients to collect their semen specimen in a busy male infertility clinic. Our results showed that the median time for collection was nearly 12 minutes, indicating that half the men required less than 12 minutes to collect their semen specimen, and half required more than 12 minutes.
While the age of the patients did not significantly impact their collection time, patients accompanied by their partners tended to require longer times, and were significantly more likely to take longer than 15 minutes compared to patients who were unaccompanied. We consider these observations to be useful to institutions that may be planning to start their own male infertility practices, as well as to centers currently encouraging their patients to be accompanied by partners during collection, as our results indicate that this may not be the most efficient collection method.
The use of infertility treatments in the United States has risen sharply over the past three decades (2). Likewise, our male infertility practice has grown over the years, with an increasing demand for limited clinical space. It is important that semen analysis be performed within one hour of semen collection to optimize the accuracy of results. In most cases, this time requirement necessitates that semen collection be performed in clinical space that is in close proximity to the testing laboratory so that the semen specimen can be handed-off to laboratory personnel. The custody and quality control of the semen specimen can be monitored in the clinic setting whereas this monitoring cannot be performed when the specimen is collected at home or in other conditions not administered by the testing laboratory. Therefore, to schedule time in the clinic for semen collection, it is important to understand the average duration necessary for male patients to collect their semen specimens in this setting.
Numerous measures and indexes have been used in the literature to evaluate the outcomes and best practices of infertility in assisted reproduction clinics and laboratories (3,4), however, to our knowledge, the duration of time required for semen collection in men attending an infertility clinic has not been reported, even though this factor can have a major impact on the organization of such a practice. We hypothesized, based on our clinical observations, that older men would tend to take longer, as well as men with their partners. We were surprised to find that age did not significantly correlate with collection time; nor did any comparison between different age groups show significant differences. Regarding the presence or absence of the patients’ partners in the room, however, our cohort did show significant differences—patients with their partners tended to require longer times and were significantly more likely to require more than 15 minutes.
These results have relevance for optimizing the efficiency of this essential step in any male infertility-related practice, as it is a very common practice for healthcare providers in this setting to encourage female partners to accompany patients into the semen collection rooms. We do not know the reason for this difference, but we hypothesize from qualitative observations, in the form of conversations with our patients, that it might be due to the couples’ attempt to “romanticize” the situation—a circumstance missing when the patient is alone. In some cases, patients stated that their partners “made them nervous”, one of them being unable to provide a sample because of this reason. For patients unable to provide a semen sample because of situational anxiety, the use of PDE5 inhibitors has been suggested as a helpful aid without affecting the quality of the sample (5). This event was very rare in our sample, and therefore PDE5 is not currently part of our practice.
Infertility evaluation, as well as cryopreservation in cancer patients, are highly anxiety-inducing experiences, therefore this might also be a contributing factor. The purpose of semen collection, i.e., screening, cryopreservation, evaluation after a surgery (vasectomy or vasectomy reversal)—did not have a significant impact on semen collection time. It is worth noting, however, that our cohort contained a very limited number of patients in some of those groups, and the lack of significant differences may be due to limited statistical power. Similarly, we were unable to detect differences between patients cryopreserving prior to a cancer treatment (and who may be in poor health) compared to those collecting for other reasons, due to the limited representation of this patient group in our random sample.
Despite these limitations, we provide in this study some observations on duration of semen collection that have not been previously reported. The results of our study will aid practices related to male infertility that are initiating a semen analysis program, or aiming for quality improvement in scheduling time and space for semen collection.
In conclusion, in the establishment of a male infertility clinic, there are a number of organizational factors to take into consideration and plan in detail. Many indexes have been developed and studied to assess the functioning and outcomes of this kind of practice. Timing of semen collection, however, has not been previously reported. In our cohort, the median semen collection time was 12 minutes. The only variable with a negative impact on the collection time was the presence of a female partner in the collection room. Our findings can aid in optimizing the scheduling of patients requiring semen collection in a clinical setting.
Acknowledgements
The authors acknowledge Teodoro Aballa, MS for his valuable technical contributions.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was granted exempt status by the Institutional Review Board.
References
- Practice Committee of American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril 2012;98:294-301. [Crossref] [PubMed]
- Odisho AY, Nangia AK, Katz PP, et al. Temporal and geospatial trends in male factor infertility with assisted reproductive technology in the United States from 1999-2010. Fertil Steril 2014;102:469-75. [Crossref] [PubMed]
- Mourad SM, Hermens RP, Cox-Witbraad T, et al. Information provision in fertility care: a call for improvement. Hum Reprod 2009;24:1420-6. [Crossref] [PubMed]
- Sunde A, Balaban B. The assisted reproductive technology laboratory: toward evidence-based practice? Fertil Steril 2013;100:310-8. [Crossref] [PubMed]
- Aversa A, Mazzilli F, Rossi T, et al. Effects of sildenafil (Viagra) administration on seminal parameters and post-ejaculatory refractory time in normal males. Hum Reprod 2000;15:131-4. [Crossref] [PubMed]


