Relationship between chronic testicular pain and mental health diagnoses
Introduction
Chronic testicular pain, also known as chronic orchialgia, is a common presenting complaint to the urologist. Chronic orchialgia has been defined as an intermittent or constant, unilateral or bilateral testicular pain that lasts three months or longer. This pain should also significantly interfere with the daily activities of a patient, so as to prompt him to seek medical attention (1). Appropriate evaluation of chronic orchialgia has been previously studied in the military setting (2). Current management ranges from conservative management (scrotal support, NSAIDs, rest, nerve blocks) to surgery (microsurgical denervation, epididymectomy, orchiectomy). All modalities attempt to address anatomic and physical causes for pain with varying degrees of success (3). As the etiology of the pain is not identified in many instances, it may not be addressed by current medical and surgical practice (4).
Chronic pain affecting various parts of the body has become a more prevalent complaint with possible psychological significance. In some instances, these pain syndromes can be attributed to depressive conditions (5). Conversely, conditions such as chronic back pain have been shown to be a predisposition to psychologic conditions. Many patients with orchialgia often demonstrate a strong clinical depressive abnormality on psychological testing (6). In more recent literature, there is evidence that antidepressants may help with the management of chronic orchialgia, further reinforcing this potential relationship (3). The purpose of this study was to determine if there is a statistically significant association between mental health (MH) diagnoses and orchialgia.
Methods
Database search
The study was approved by the Brooke Army Medical Center Office of the Institutional Review Board. Consent was waived as the data was provided to the investigators in a de-identified format. Data sources were the outpatient military electronic health records systems known as CHCS and AHLTA. The Armed Forces Health Longitudinal Technology Application (AHLTA) is the primary electronic medical record (EMR) used by the Department of Defense (DoD) for outpatient care. It was implemented in January 2004, but not in widespread use at military treatment facilities (MTFs) until 2005. The Composite Health Care System (CHCS) is an older medical informatics system, now only used to book appointments, order laboratory or radiology studies and review results. The retrospective review was performed by searching CHCS for adult patients within the San Antonio Military Health System with an initial entry of the ICD-9 code 608.9 (unspecified disorder of male genital organs), from January 2005 to April 2015. The search was performed by an AHLTA database administrator. Patients with an accompanying entry of the codes 608.20 (torsion of testis), 604.9 (orchitis and epididymitis), and 878.2 (open wound of scrotum and testis without complication), were excluded. Patients with an entry of the CPT codes 55250 (vasectomy), 55040 (hydrocelectomy), 54840/54830 (spermatocelectomy), 55530 (varicocelectomy), or any of the 6 codes indicating a hernia repair within the 3 months leading up the 608.9 code were also excluded. The records of the remaining patients were then searched within the AHLTA database, to confirm that the diagnosis was actually testicular pain with a duration longer than 3 months. A comparative cohort was then obtained, by searching CHCS for patients with a new entry of the ICD-9 code 603.9 (hydrocele not otherwise specified). Hydroceles were selected as a common presenting diagnosis in the same general anatomic area as orchialgia, but with no associated pain and a low likelihood of psychological distress attributed to the diagnosis. Both cohorts were then searched for the prevalence of MH diagnoses. All of the patients identified to have a MH diagnosis had an entry of at least one of the following seven ICD-9 codes: 300 (anxiety unspecified), 300.02 (generalized anxiety disorder), 311 (depressive disorder not classified elsewhere), 296.3 (major depressive affective disorder), 309.24 (adjustment disorder with anxiety), 309.28 (adjustment disorder with mixed anxiety and depressed mood), and 309.81 (post-traumatic stress disorder). The ICD9 codes in this study population were grouped into 4 for purposes of the analysis as follows: anxiety (300, 300.02), depression (311, 296.3), adjustment disorder (309.24, 309.28), and post-traumatic stress disorder (309.81).
Statistical analysis
Categorical data was summarized using percentages and analyzed using Chi-Squared tests or Fisher’s exact test, whichever was most appropriate. Means and standard deviations or medians and inter-quartile ranges were used as summary statistics for continuous variables and were analyzed using Student’s t-test and ANOVA or Wilcoxon’s Test, whichever was most appropriate. Significance for results was established when P values were less than 0.05. Comparisons between the study data and NIMH survey data were performed using Wilson’s approximation of the exact limits for a binomial distribution to determine exact 95% confidence intervals. All statistical analysis was performed using SPSS v 22.0 (IBM).
Results
Patient characteristics
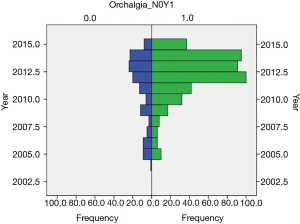
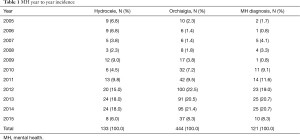
A total of 500 men were identified by ICD-9 code alone. After applying the exclusion criteria, 444 men were included in the study population, with 133 in the control cohort. Demographic data collected was age, branch of service, and enlisted versus officer. Mean age in the orchialgia cohort and controls was 32.4±7.9 and 31.2±8.8 years respectively. Both cases and controls were predominantly serving in the United States Army—298 (67.1%) and 96 (72.2%) respectively, with enlisted service members making up 379 (85.4%) and 115 (86.5%) of the cases and controls respectively. There was no significant difference in MH diagnosis based on enlisted vs. officer status (P=0.748); branch (P=0.622); or age (P=0.161). The incidence of orchialgia increased significantly over the study period (P=0.001) (Figure 1). There was a higher prevalence of MH diagnoses in the later years of the study, but this did not reach statistical significance (P=0.063) (Table 1).
Full table
MH diagnoses
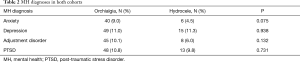
The overall prevalence of one or more MH diagnoses in both groups was 21%, with 44.6% of the patients having one diagnosis, 29.8% with two diagnoses, and 25.6% with three or four diagnoses. The prevalence of a MH diagnosis was not significantly higher in the orchialgia group than in the hydrocele group (21.6% vs. 18.8%; P=0.479). The prevalence of anxiety was twice as high in men with orchialgia (9.0% vs. 4.5%), though it did not quite reach significance (P=0.075) (Table 2). The prevalence of adjustment disorder and PTSD were also higher in the orchialgia group, but not significantly. The percentage of patients with depression was equal in both groups (11.0% vs. 11.3%; P=0.938). The prevalence of all MH diagnoses was higher than in the general male population in the US based on National Institute of Mental Health (NIMH) statistics, with the difference being strongly significant based on 95% CI (Table 3).
Full table

Full table
Discussion
The exact scope of the problem is somewhat unclear, but current reports of chronic orchialgia presentation include 38.8% of male chronic pelvic pain patients localizing their pain to the scrotum (7), and chronic scrotal pain occurring in 4.8% of men presenting to an outpatient urologist (8). Furthermore, it is a condition that can be difficult to manage. In a recently published integrated review of the literature, Quallich concluded that the research into chronic testicular pain lags behind other chronic pain syndromes, such as in comparison to female chronic pain. She also found that the 3 most commonly referenced articles for orchialgia are over 20 years old (9).
There are several papers that recommend a similar, progressive approach for management (1,6). These algorithms begin with determining any identifiable causes for pain and treating accordingly. However, 25–50% of orchialgia cases are of unknown etiology (10). In this scenario, management begins with a trial of ‘conservative management’ that may include NSAIDs, scrotal support, possible antibiotic use, rest, or some combination thereof. Alternative medical therapies such as biofeedback, have also been tried both alone and as an adjunctive measure to other treatment modalities, with some success (11). If the patient fails conservative management then the next recommendation is for spermatic cord blocks in clinic or with anesthesia. Should these fail, the final steps are surgical (microsurgical denervation, epididymectomy, orchiectomy), or neuromodulation. Microsurgical spermatic cord denervation is emerging as a relatively low risk procedure resulting in complete pain resolution in as high as 80% of well-selected patients (12). This procedure also avoids the potential adverse psychological effects of orchiectomy, which additionally does not guarantee relief of pain (success ranges from 20–73%) (3). This entire process may not only fail to address the complaint, it may also take many months and result in the frustration of both patient and physician. In a recent study involving the Israeli Defense Forces, the average chronic scrotal pain patient had an average of 5.3 visits, with one patient logging 27 visits (13). In the military setting, this time can have a significant impact on the patient’s ability to train or deploy. Additionally, chronic orchialgia has been the most cited reason for medical discharge in the US Army (14). Any additional management strategies may aid in a timelier return to duty and conservation of limited military resources.
There is a growing body of literature that suggests a link between urologic pain and MH disorders. In a commonly cited article, Schover showed that in male patients with genital pain, a psychologist was able to diagnose 56% with somatization disorder and 27% with major depression (15). Ching et al. found that 14% of orchialgia patients had psychiatric or behavioral issues and 9% had identifiable life stressors (16). These findings have resulted in treatment strategies that incorporate management of psychologic conditions for chronic orchialgia. Many recommend the addition of tricyclic antidepressants, as they have been shown to be effective in the management of chronic pain conditions to include orchialgia (2,16,17). Sinclair was able to find through a prospective trial that 66% of patients on nortriptyline had a greater than 50% reduction in their symptoms (3). Some advocate a multidisciplinary approach advocating treatment of identifiable underlying behavioral health issues and potential management of psychosomatic pain disorders (1,18).
As there was no statistically significant relationship between the diagnosis of orchialgia and any MH disorders included in this study, management of these patients exclusively by the urologist may be warranted. However, a few factors can be considered cause for involvement of a MH professional. First, it is possible that patients who are more likely to present with somatic complaints like orchialgia are less likely to present for evaluation and treatment for explicit MH complaints, even if psychological symptoms are present, due to a primary focus on physical rather than psychological symptoms of distress. Thus, while these patients may actually reach diagnostic criteria for a MH disorder, they would not have a previous diagnosis listed. Second, while the culture around evaluation and management of MH disorders in the military population has evolved, there still exists concern that being diagnosed with a MH disorder could have career-related consequences. This may have also influenced the rate at which patients with orchialgia would present for treatment of MH complaints. Third, there are psychological factors that contribute to health-related concerns that do not meet diagnostic criteria for a MH diagnosis. For example, patients with orchialgia may be more likely to engage in maladaptive pain-related cognitions which exacerbate pain intensity and duration but do not contribute to overall levels of more generalized MH complaints. If this were the case, it could indicate that while patients with orchialgia may have a less psychologically adaptive response to pain than others, they are not necessarily more likely to be diagnosed with a MH disorder.
One concerning finding of this study is the higher prevalence of MH diagnoses compared to the general US male population. This statistically significant difference was demonstrated in both control and orchialgia groups. This, however, is consistent with previously published data obtained from Veterans Health Administration (VHA) databases. Trivedi et al. reported a 25.7% overall prevalence of any mental illness among patients assigned to a primary care provider within the VHA system, with a significant co-occurrence among the diagnoses of PTSD, anxiety, depression, and substance use disorder (19). Additionally, there was an increasing prevalence of MH diagnoses towards the end of the review period. One important factor that may explain these findings is the timeframe incorporated into the review. During this time, the United States was engaged in combat operations in Afghanistan (Operation Enduring Freedom 2001–2014) and Iraq (Operation Iraqi Freedom 2003–2011, Operation New Dawn 2010–2011). Other published reports have also shown an increase in the prevalence of MH diagnoses over the progression of these conflicts (20,21). This baseline higher prevalence of MH diagnoses in the military population may have impacted the lack of statistical significance of our findings.
There was a significant increase in the diagnosis of chronic testicular pain from year to year throughout the study. This trend follows the increasing prevalence of MH diagnoses over the same timeframe and may represent a correlation between the two. This also could be related to the aforementioned combat operations and the associated exposure to stressful environments. However, based on our study design, the significance of this finding is unclear.
This retrospective review was done over a 10-year period of time with a large number of patients through a single electronic medical record system. A significant limitation of the study is that the findings are based on the accuracy of the ICD-9 codes entered into the system by a variety of DoD providers. However, this common EMR allowed review of the patients’ records to confirm the diagnosis of chronic testicular pain and exclude patients diagnosed with pain from other etiologies such as posttraumatic, infectious, post-surgical, etc. Additionally, another potential weakness is that although hydroceles may not generally cause pain, the psychological impact on the patient is unknown and may have affected the results.
This is the first study to investigate the possible link between MH diagnoses and chronic orchialgia in military patients. Although there was an increased prevalence of anxiety in patients with orchialgia, this did not reach statistical significance. Continued research is necessary to further elucidate the role of psychological factors in the presentation of orchialgia. Future research should independently evaluate patients presenting with orchialgia both for symptoms of MH disorders that may not have been previously diagnosed as well as for pain-related cognitions contributing to a less-adaptive response pattern.
Conclusions
In this study population, orchialgia was not found to be significantly associated with the presence of a MH diagnosis. Though there were twice as many orchialgia than hydrocele patients with anxiety, the relationship did not meet statistical significance, possibly due to the overall low prevalence of anxiety. The incidence of orchialgia began at levels similar to prior reports in civilian populations, but then rose significantly over the study timeframe, possibly related to the unique occupational hazards of the study population. These results may also be skewed by the overall higher percentage of MH diagnoses in the study population than in the general population.
Acknowledgements
Special thanks to: Dairyel C. McCloud, AAS, Crystal L. Delvalle, BA: General and administrative support; James K. Aden, PhD: Statistics; Daniel Dedman: EMR administration.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Brooke Army Medical Center Office of the Institutional Review Board (number 386528-1). Consent was waived as the data was provided to the investigators in a de-identified format.
References
- Costabile RA, Hahn M, McLeod DG. Chronic orchialgia in the pain prone patient: the clinical perspective. J Urol 1991;146:1571-4. [Crossref] [PubMed]
- Davis BE, Noble MJ, Weigel JD, et al. Analysis and management of chronic testicular pain. J Urol 1990;143:936-9. [Crossref] [PubMed]
- Sinclair AM, Miller B, Lee LK. Chronic orchialgia: Consider gabapentin or nortriptyline before considering surgery. Int J Urol 2007;14:622-5. [Crossref] [PubMed]
- Granitsiotis P, Kirk D. Chronic testicular pain: An overview. Eur Urol 2004;45:430-6. [Crossref] [PubMed]
- Magni G, de Bertalini C. Chronic pain as a depressive equivalent. Postgrad Med 1983;73:79-85. [Crossref] [PubMed]
- Masarani M, Cox R. The aetiology, pathophysiology and management of chronic orchialgia. BJU Int 2003;91:435-7. [Crossref] [PubMed]
- Zermann DH, Ishigooka M, Doggweiler R, et al. Neurourological insights into the etiology of genitourinary pain in men. J Urol 1999;161:903-8. [Crossref] [PubMed]
- Ciftci H, Savas M, Yeni E, et al. Chronic orchialgia and associated diseases. Curr Urol 2010;4:67-70. [Crossref]
- Quallich SA, Arslanian-Engoren C. Chronic testicular pain in adult med: an integrative literature review. Am J Mens Health 2013;7:402-13. [Crossref] [PubMed]
- Sigalos JT, Pastuszak AW. Chronic orchialgia: epidemiology, diagnosis and evaluation. Transl Androl Urol 2017;6:S37-43. [Crossref] [PubMed]
- Ye ZQ, Cai D, Lan RZ, et al. Biofeedback therapy for chronic pelvic pain syndrome. Asian J Androl 2003;5:155-8. [PubMed]
- Tatem A, Kovac JR. Chronic scrotal pain and microsurgical spermatic cord denervation: tricks of the trade. Transl Androl Urol 2017;6:S30-6. [Crossref] [PubMed]
- Rottenstreich M, Glick Y, Gofrit ON. Chronic scrotal pain in young adults. BMC Res Notes 2017;10:241. [Crossref] [PubMed]
- Kavoussi PK, Costabile RA. Orchialgia and the chronic pelvic pain syndrome. World J Urol 2013;31:773-8. [Crossref] [PubMed]
- Schover LR. Psychological factors in men with genital pain. Cleve Clin J Med 1990;57:697-700. [Crossref] [PubMed]
- Ching CB, Hays SR, Luckett TR, et al. Interdisciplinary pain management is beneficial for refractory orchialgia in children. J Pediatr Urol 2015;11:123.e1-6. [Crossref] [PubMed]
- Starke NR, Costabile RA. Medical management of chonic orchalgia. Transl Androl Urol 2017;6:S48-50. [Crossref] [PubMed]
- Lian F, Shah A, Mueller B, et al. Psychological perspectives in the patient with chronic orchialgia. Transl Androl Urol 2017;6:S14-9. [Crossref] [PubMed]
- Trivedi RB, Post EP, Sun H, et al. Prevalence, Comorbidity, and Prognosis of Mental Health Among US Veterans. Am J Public Health 2015;105:2564-9. [Crossref] [PubMed]
- Seal KH, Metzler TJ, Gima KS, et al. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health 2009;99:1651-8. [Crossref] [PubMed]
- Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med 2007;167:476-82. [Crossref] [PubMed]