
Contemporary surgical and technical aspects of transurethral resection of bladder tumor
Introduction
Transurethral resection of bladder tumor (TURBT) remains the gold standard of staging urothelial cancer of the bladder and treating non-muscle invasive bladder cancer (NMIBC) (1). TURBT aims proper diagnosis, correct staging, and remove of all lesions. Indeed, residual tumor after initial TURBT is associated with a higher risk of disease recurrence (2). Therefore, complete and optimal TURBT is crucial to achieve good oncological outcomes. Given this cornerstone role, achieving a high-quality resection should be the first step of the primary management of NMIBC. This resection requires best of care in terms of diagnosis, visualization, disease burden assessment, resection and optimal specimen analysis.
Herein, we discuss the major contemporary surgical and technical aspects including en bloc resection, bipolar and laser resection as well as best standards for TURBT. New visualization and detection techniques and re-TURBT are not discussed in the current article.
Surgical and technical aspect of TURBT
Cystoscopy and mapping
The first step of the TURBT includes a thorough cystoscopy. During this step, fresh urine can be collected for urine cytology if not performed earlier. The cystoscopy assesses the number, the location, and the aspects of all suspicious lesions. Specifically, the distance to the ureteral orifices, the trigonal lesions, bladder neck, and prostatic urethra invasion. The EAU guidelines recommend a standardized mapping (1). The mapping may be useful when a distinct pathology reports is warranted in some clinical scenarios.
Resection type: conventional vs. en bloc resection
TURBT using a wire loop is considered the gold standard for staging and treating NMIBC. However, the piecemeal resection, the potential scattering of tumor cells, the absence of detrusor muscle (DM) in the resected specimen are thought to be drawbacks of the conventional resection. Thus, in order to improve the quality of the resection and, ultimately decreasing the recurrence rate, the en bloc resection was introduced (3). Different options, including loop modifications, laser techniques and water-jet based enucleation, have been reported (3-6). The “en bloc” technique include the incision of the surrounding mucosa with a safety margin to detach the tumor in one piece. Care should be taken to get deep enough in the bladder wall to remove DM (7). Studies could demonstrate DM in all cases and the resection of tumor up to 7.5 cm (4,8). However, this approach failed to demonstrate any improvements of oncological outcomes.
Energy
Modifications, such as bipolar TURBT have several advantages such as reduction of the obturator nerve injury. In fact, stimulation of the nerve may lead to the patient motion that can cause bladder perforation (7). In addition, bipolar vaporization allows, enucleation and debulking techniques and subsequent resection of the tumor base (7). However, bipolar TRUBT doesn’t preclude resection requirements including complete tumor removal and muscle sampling. A recent systematic review and meta-analysis that compared bipolar and monopolar TURBT did not report any statistically significant differences between bipolar TURBT and monopolar TURBT for rates of obturator nerve reflex, bladder perforation, and transfusion. Cautery artifacts were similar in both procedures. There was no significant difference in disease recurrence rates when comparing the two types of procedures (9).
Bladder neck and prostate biopsy
The biopsy of the bladder neck and the prostatic urethra with there is an evidence of disease is not questioned. However, in some cases, the involvement is not visible. The risk of involvement is higher in case of carcinoma in situ (CIS), high-grade tumor, and positive cytology without evidence of the disease in the bladder (10).
When indicated, the biopsy from abnormal areas in the prostatic urethra and from the precollicular area (between the 5 and 7 o’clock position) are performed using a resection loop or cold-cup biopsy when stromal invasion is not suspected (1).
Quality control
The aims of TURBT include the resection of all macroscopic lesions, establish pathological stage and grade and identify significant prognostic factors (2). These being of the utmost importance for patient management, quality control of the procedure is mandatory. Pathologists and urologists have both a major play role in achieving a gold standard procedure.
According, to the International Society of Urological pathology (ISUP) recommendations, pathology reports should be standardized and should at least mention tumor stage and grade, the presence of DM in the resected specimens, the present of any histological variants, and concomitant CIS (11). A permanent dialogue between urologists and pathologists should be established to review cases and confront pathological findings with clinical findings.
From a surgical perspective, a good-quality TURBT is not always achieved because of poor cystoscopic view, tumor size, multifocality of the disease, difficult location, an inexperienced surgeon or complications such as bleeding or bladder perforation. Inadequate tumor clearance results in early recurrence and inaccurate staging of the cancer. After reviewing published controlled studies, the recurrence rate at the first follow-up cystoscopy (RRFFC) was introduced by the European Organization for Research and Treatment of Cancer (EORTC) (12). It was concluded that this discrepancy was a result of variability in the quality of the resections. A low RRFFC was reported to be associated with the presence of DM on the specimen which is significantly more achieved when the procedure was performed by a senior surgeon (13). DM in the specimen is easy to identify allowing an immediate quality control of TURBT.
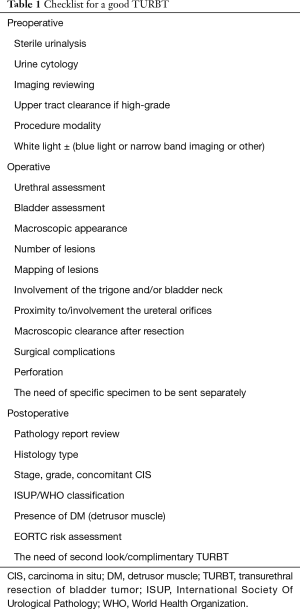
Another way of improving the quality of TURBT is the implementation of a check-list in order to standardize the surgical procedure and therefore enhance its performance and improve surgical and oncological outcomes. As such, an eight-item check-list was reported to improve disease-free survival after TURBT but failed to improve the rate of DM in the resected specimens (14).
Finally, the best TURBT is achieved when the procedure is performed in standardized fashion (Table 1). This standardization should be part of the training process of junior urologists.
Full table
Conclusions
TURBT is a cornerstone of the primary management of bladder tumors. Achieving a high-quality resection allows a correct treatment, staging and classification of the tumor. Because of the jeopardized prognosis of a bad TURBT, the procedure should be performed by experienced surgeons or strictly supervised when performed by trainees. Ideally, procedure should be standardized according to best practice recommendations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- The EAU Guidelines in non-muscle-invasive bladder cancer (TaT1 and CIS). Available online: http://www.uroweb.org/gls/pdf/05_TaT1_Bladder_Cancer_LR.pdf
- Mariappan P, Zachou A, Grigor KM, et al. Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on opesrator experience. Eur Urol 2010;57:843-9. [Crossref] [PubMed]
- Ukai R, Kawashita E, Ikeda H. A new technique for transurethral resection of superficial bladder tumor in 1 piece. J Urol 2000;163:878-9. [Crossref] [PubMed]
- Fritsche HM, Otto W, Eder F, et al. Water-jet-aided transurethral dissection of urothelial carcinoma: a prospective clinical study. J Endourol 2011;25:1599-603. [Crossref] [PubMed]
- Gao X, Ren S, Xu C, et al. Thulium laser resection via a flexible cystoscope for recurrent non-muscle-invasive bladder cancer: initial clinical experience. BJU Int 2008;102:1115-8. [Crossref] [PubMed]
- Xishuang S, Deyong Y, Xiangyu C, et al. Comparing the safety and efficiency of conventional monopolar, plasmakinetic, and holmium laser transurethral resection of primary non-muscle invasive bladder cancer. J Endourol 2010;24:69-73. [Crossref] [PubMed]
- Bach T, Muschter R, Herrmann TR, et al. Technical solutions to improve the management of non-muscle-invasive transitional cell carcinoma: summary of a European Association of Urology Section for Uro-Technology (ESUT) and Section for Uro-Oncology (ESOU) expert meeting and current and future perspectives. BJU Int 2015;115:14-23. [Crossref] [PubMed]
- Zhang J, Wang L, Mao S, et al. Transurethral en bloc resection with bipolar button electrode for non-muscle invasive bladder cancer. Int Urol Nephrol 2018;50:619-23. [Crossref] [PubMed]
- Cui Y, Chen H, Liu L, et al. Comparing the Efficiency and Safety of Bipolar and Monopolar Transurethral Resection for Non-Muscle Invasive Bladder Tumors: A Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A 2016;26:196-202. [Crossref] [PubMed]
- Hara T, Takahashi M, Gondo T, et al. Risk of concomitant carcinoma in situ determining biopsy candidates among primary non-muscle-invasive bladder cancer patients: retrospective analysis of 173 Japanese cases. Int J Urol 2009;16:293-8. [Crossref] [PubMed]
- Compérat EM, Burger M, Gontero P, et al. Grading of Urothelial Carcinoma and The New “World Health Organisation Classification of Tumours of the Urinary System and Male Genital Organs 2016”. Eur Urol Focus 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Brausi M, Collette L, Kurth K, et al. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: a combined analysis of seven EORTC studies. Eur Urol 2002;41:523-31. [Crossref] [PubMed]
- Mariappan P, Finney SM, Head E, et al. Good quality white-light transurethral resection of bladder tumours (GQ-WLTURBT) with experienced surgeons performing complete resections and obtaining detrusor muscle reduces early recurrence in new non-muscle-invasive bladder cancer: validation across time and place and recommendation for benchmarking. BJU Int 2012;109:1666-73. [Crossref] [PubMed]
- Suarez-Ibarrola R, Soria F, Abufaraj M, et al. Surgical checklist impact on recurrence-free survival of non-muscle invasive bladder cancer patients undergoing transurethral resection of bladder tumor. BJU Int 2018. [Epub ahead of print]. [Crossref]


