Two cases of successful microsurgical penile replantation with ischemia time exceeding 10 hours and literature review
Introduction
Traumatic amputation of the penis is a rare surgical emergency, which can be due to self-mutilation, circumcision, assault, accidents, and animal attacks (1). Ehrich et al. firstly described the penile replantation in 1929 and since then this rare urological condition has come in attention (2). The first successful microsurgical replantation of an amputated penis was reported in 1977 (3). The current concept of treatment choice is microvascular penis replantation for penile amputation because it yields better appearance, preservation of sensation, physiological micturition and erectile function. About more than 70% of cases were treated with macroscopic penis replantation since 1970. An 80 cases systematic review from 1996 to 2007 reported that only 37.5% of cases underwent a successful replantation (4). And, failure of macroscopic penis replantation and its causes are poorly understood and reported. The aim of this study is to evaluate the treatment and prognosis of microsurgical replantation of penile amputation with a relative long-term ischemia, and review related literatures to summarize relevant clinical experiences.
Case presentation
Case 1
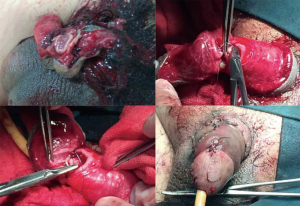
A 41-year-old patient was referred to our hospital with an incomplete amputation of penis for 9 hours during a family conflict. No ice bags were applied to the wound, and there was still an arterial bleeding around the wound in spite of a compression of his hands. At presentation, his blood pressure was 75/45 mmHg, and the heart rate was 95 bpm. Laboratory test revealed that the hemoglobin was 85 g/L. Fluid infusion was applied and the patient was taken to the operating room for an emergent surgical management. After the general anesthesia was applied, wound exploration revealed that the injury on the ventral side was severe with bleeding, and the urethra and the bilateral corpus cavernosum were completely severed. The left dorsal artery was broken, however, the tissue distal to the amputated part still looked viable, probably due to a blood supply from the intact right dorsal artery. The wound was washed with heparinized antibiotic saline solution to allow clear identification of the deep dorsal veins, nerves and arteries, and then a 16F Foley catheter was inserted into the bladder through the penile urethra. Urethra along with the spongiosum was sutured 6 points by spatulated end to end anastomosis using 4-0 of the Vicryl line. The end-to-end microsurgical repair of the left dorsal artery was sutured 6 points with 10-0 absorbable suture, followed by suturing of Buck’s fascia and skin, and pressure bandage was applied (Figure 1). The surgery time was 2 hours 10 minutes and the total ischemia time was around 12.5 hours. Postoperatively the patient was managed with intravenous antibiotics and dextran, subcutaneous injection of low molecular heparin, intra-cavernous injection of papaverine, oral tadalafil, and phototherapy of penis. Minor penile skin necrosis was observed after 1 week and cavernous injection of papaverine could induce cavernous congestion that leaded to penile erection. After 30 days, the patient was able to erect autonomously with grade III–IV rigidity and urinate normally. At three months follow-up, the patient had satisfied erections, with no urinary fistula, normal urine stream, and decent penile sensation.
Case 2
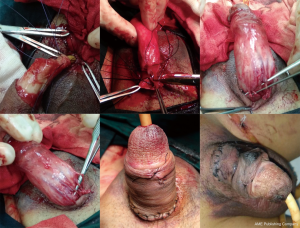
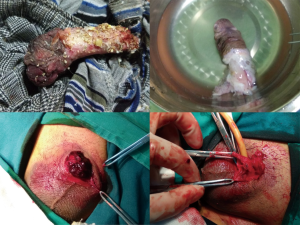
A 53-year-old patient suffered complete penile amputation by a threshing machine during farm work. He was referred to our institute with the amputated penile preserved in ice 12 hours after the injury. The severance was around the end of the penile. There was no obvious bleeding from the wound due to the formation of a blood clot on the wound. Vitals were stable and the patient was taken to operating room for further surgical procedure. The patient was unable to urinate thus a cystostomy was performed prior to the operation. The amputated penile was washed thoroughly in 4 °C normal saline to remove all foreign particle and then placed in 4 °C heparin-cephalosporin saline solution for half hour in order to prevent infection and dissolve the thrombus in the vessels (Figure 2). Then debridement was performed on the amputated penile, Buck fascia was exposed and deep dorsal vein, bilateral dorsal artery and nerve were revealed. Under the microscope the dorsal artery was infused with heparin and antibiotic solution and irrigated till clear fluid was seen coming out of the deep dorsal vein. Next, a debridement was performed on the proximal part of the wound. Urethra and corpus cavernosum were clarified, and the deep dorsal vein and the bilateral dorsal arteries were traced along dorsal part of the corpus cavernosum. Bilateral dorsal arteries were irrigated with heparin-antibiotic solution until oozing of blood, and then the arteries were clamped. Urethra along with the corpus spongiosum was sutured 6 points by spatulated end to end anastomosis using 4-0 of the Vicryl line. Following vascular anastomosis glans restored partial blood supply and pink coloration of the skin was observed. The end-to-end microsurgical anastomosis of the dorsal arteries, deep dorsal vein and dorsal nerves were sutured 6 points with 10-0 absorbable suture, followed by suturing of the skin, and finally pressure bandage was applied (Figure 3). The surgery time was 3 hours 15 minutes and revascularization was established about 14.5 hours after the amputation. Postoperatively the patient was managed with intravenous antibiotics, subcutaneous injection of low molecular heparin intra-cavernous injection of papaverine, oral tadalafil, and phototherapy of penis. Moderate penile skin necrosis was observed after 1 week, which was debrided by a followed operation. In the operation, urethra and bilateral corpus cavernosum were explored to be viable, and the skin around root of penis was released, and the remaining prepuce was sutured with the urethral opening. The patient was able to erect with grade II rigidity, and could urinate normally after 30 days. After 3 months of follow-up the patient acquired an erection with grade II–III rigidity, no urinary fistula formation, weak urine stream, and fine penile sensation. The patient was advised for urethral dilatation periodically.
Discussion
In 2013 Li et al. conducted meta-analysis of 111 cases of penile replantation in Chinese population, they proposed that unless with severe damage or contamination, penile replantation should not be abandoned (5). In 2017 Morrison et al. reported 106 cases review of penile replantation, they came up with a similar opinion (6). Penile amputation is still an uncommon genital injury thus poses a greater challenge to surgeons due to limited number of cases, demanding surgical technique and lack of standard post-operative care protocol. Thus, evaluation of the effectiveness, safety, restoration of penile function, is necessary to understand and provide a better guidance in the management of this uncommon condition. Up to now, researchers accepted that the factors contributing to the outcomes of penile replantation include duration of ischemia, type of injury, the degree of injury and the type of surgery (7,8).
Li et al. reported the average hot ischemia period of penile amputation in Chinese population was 5.18 hours with 70% of patients presenting for treatment in less than 6 hours (5). Many studies have suggested within 6 hours post amputation as a golden period for satisfactory surgical outcome but there were some cases reported successful replantation after 16 hours cold-ischemia or 6 hours of hot ischemia as well. Microsurgical repair exceeding 24 hours of injury has also shown to be successful (9,10). In this presentation, the ischemia time of the two cases both exceeded 10 hours, but finally the patient acquired a satisfactory recovery of anatomy and function. Reviewing the published data in last 5 years, we summarized the successful penile amputation replantation cases (Table 1), as a result 23.4% (3/17) cases were performed with a microsurgical management while 82.4% (14/17) cases were operated with a traditional surgery, the ages varies from 7 days to 70 years, and all of them had a good postoperative performance and complications were not severe, so this indicated that in most situations, patients can benefit from replantation surgery.

Full table
The amputation of penis can be divided into two types, complete amputation and incomplete amputation, depending on the degree of injury. In case of incomplete amputation with vessels and nerves survived, the prognosis is better than those with severe neurovascular damage. Phonsombat et al. in a review of 110 cases found that the most common causes of penile amputation were gunshot injury (49%), stab injury or laceration (44%) and bite (7%) (1). Among them 50% of the stab injury or laceration were due to psychiatric disorder and self-mutilation. Re-suturing after amputation with a sharp object might be technically less demanding due to easy access and better identification of the vessels and nerves with intact margin and smooth surface. But it’s difficult when the injury is due to blunt object because of the distorted anatomy.
The major source of blood supply to penis is from the internal pudendal artery but accessory arteries arising from the external iliac, obturator, vesicular and femoral arteries also exist. At the perineum the internal pudendal artery becomes the common penile artery and it further divides into three major branches namely the dorsal, bulbourethral, and the cavernous artery. These arteries join at the glans to forms a vascular ring. The dorsal penile artery that runs between the Buck fascia and tunica albuginea is responsible for the engorgement of the glans during erection. The bulb and the corpus spongiosum are supplied by the bulbourethral artery. The cavernous artery enters the corpus cavernosum at the hilum of penis and effects the tumescence of the cavernosum. It then further divides into many helical arteries along its course supplying the erectile tissue and sinusoids. The bulbourethral and the urethral arteries are located outside of the tunica albuginea on the lateral and dorsal sides of the corpus spongiosum. The cavernous and the urethral arteries unite outside the tunica of the spongiosum. It has been reported that selective or total ligation of dorsal penile arteries does not cause necrosis or loss of erectile function (22). There are three main parts of the venous flow of the penis. The superficial dorsal vein collected the blood flow of the subcutaneous tissue of penis, which then joined into external pudendal veins, great saphenous vein and vena iliaca externa successively. The small venous flow of the distal 2/3 of the penis head and the cavernous body are remitted into the deep vein, then into the prostate vein plexus, vena cava and internal iliac vein in turn. The venous flow of proximal 1/3 penis cavernous, penile and urethral cavernous venous remit into the cavernous venous vein and urethral vein, and then into the vena cava and internal iliac vein. Because of the blood supply characteristic of the penis, it is possible to succeed in the penile replantation without blood vessels anastomosed (23). Based on the meta-analysis reported by Li et al., and together with the reported cases in recent years, there were 51 partial and 73 complete amputations that were successful with a replantation operation, and there was no difference in complication rates between partial and complete amputation. Among them microsurgical repair was applied in 63 cases and non-microsurgical technique used in 49 cases, and the others were unknown about the exact kind of operation (11-21). The major complications associated with penile replantation are skin necrosis, venous congestion, abnormal sensation of the skin, urethral stricture, urethral fistula formation, and loss of erectile function. Microsurgical repair is not only associated with better erectile function, lower urethral stricture and fistula formation, and penile sensation can also be restored better with this technique. The early microsurgical re-anastomosis of the dorsal penile vein, penile arteries, and dorsal nerves is the critical factor for the success of replantation (4,24,25). Therefore, microsurgical replantation should be offered and be treatment of choice for penile amputation patients preferentially for a better physical and psychosocial outcome.
After replantation surgery postoperative administration of broad-spectrum antibiotics vasoactive agents and diethylstilbestrol has been reported. In some reported cases, phototherapy treatment has also been applied. In clinical practice, diethylstilbestrol is used to inhibit erection in order to resist the postoperative bleeding, however, the blood supply of corpus cavernosum would be suppressed as well. Comparing to bleeding, we consider that the risk is higher for inadequate blood supply to the graft. Thus, we did not prescribed diethylstilbestrol in both cases, and tadalafil combined with injection of chemical prosthesis were administered to increase the intracavernosal blood supply (26).
Conclusions
(I) Except for severe injury, gross contamination or loss of the amputated penile ischemia time should not be the determining factor and Penile replantation surgery, microsurgical re-anastomosis should be offered unless otherwise. (II) The mode of injury contributes to the replantation outcomes. The prognosis in the ones with intact or partially damaged nerves and vessels will be better than those with severe neurovascular injuries. Re-suturing after amputation with a sharp object might be technically less demanding due to easy access and better identification of the vessels and nerves with intact margin and smooth surface. But is difficult when the injury is due to blunt object because of the distorted anatomy. (III) Because of the multiple and complex blood supply system to the penis, it is sometime possible for replanted graft survive without anastomosis of the vessels. (IV) Microsurgical repair is associated with greater graft survival, better sensation restoration and lower incidence of erectile dysfunction, urethral stricture, urinary fistula formation and skin necrosis. Thus, microsurgical replantation should be offered and be treatment of choice preferentially in penile amputation patients for a better physical and psychosocial outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional (Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Phonsombat S, Master VA, Mcaninch JW. Penetrating external genital trauma: a 30-year single institution experience. J Urol 2008;180:192-5; discussion 195-6. [Crossref] [PubMed]
- Ehrich WS. Two unusual penile injuries. J Urol 1929;21:239. [Crossref]
- Cohen BE, May JW Jr, Daly JS, et al. Successful clinical replantation of an amputated penis by microneurovascular repair: Case Report. Plast Reconstr Surg 1977;59:276-80. [Crossref] [PubMed]
- Babaei AR, Safarinejad MR. Penile replantation, science or myth. A systematic review? Urol J 2007;4:62-5. [PubMed]
- Li GZ, Man LB, He F, et al. Replantation of amputated penis in Chinese men: A meta-analysis. Zhonghua Nan Ke Xue 2013;19:722-6. [PubMed]
- Morrison SD, Shakir A, Vyas KS, et al. Penile Replantation: A Retrospective Analysis of Outcomes and Complications. J Reconstr Microsurg 2017;33:227-32. [Crossref] [PubMed]
- Landström JT, Schuyler RW, Macris GP. Microsurgical penile replantation facilitated by postoperative HBO treatment. Microsurgery 2004;24:49-55. [Crossref] [PubMed]
- Chou EK, Tai YT, Wu CI, et al. Penile replantation, complication management, and technique refinement. Microsurgery 2008;28:153-6. [Crossref] [PubMed]
- Wei FC. Microsurgical replantation of a completely amputated penis. Ann Plast Surg 1983;10:317-21. [Crossref] [PubMed]
- Faydaci G, Ugur K, Osman C, et al. Amputation of glans penis: A rare circumcision complication and successful management with primary anastomosis and hyperbaric oxygen therapy. Korean J Urol 2011;52:147. [Crossref] [PubMed]
- Musa MU, Abdulmajid UF, Mashi SA, et al. Traumatic penile amputation in a 15-year-old boy presenting late in northwestern Nigeria. Clin Case Rep 2016;4:786-8. [Crossref] [PubMed]
- Facio FN Jr, Spessoto LC, Arruda P, et al. Penile Replantation After Five Hours of Warm Ischemia. Urol Case Rep 2015;3:77-9. [Crossref] [PubMed]
- Garg S, Date SV, Gupta A, et al. Successful microsurgical replantation of an amputated penis. Indian J Plast Surg 2016;49:99-105. [Crossref] [PubMed]
- Fuoco M, Cox L, Kinahan T. Penile amputation and successful reattachment and the role of winter shunt in postoperative viability: A case report and literature review. Can Urol Assoc J 2015;9:E297-9. [Crossref] [PubMed]
- Gurunluoglu R, Shah M, Kim F. Microsurgical Penile Replantation after Self-inflicted Amputation in a Schizophrenic Patient: 5-year Follow-up. Plast Reconstr Surg Glob Open 2015;3:e319. [Crossref] [PubMed]
- Raheem OA, Mirheydar HS, Patel ND, et al. Surgical management of traumatic penile amputation: a case report and review of the world literature. Sex Med 2015;3:49-53. [Crossref] [PubMed]
- Banihani OI, Fox JA, Gander BH, et al. Complete penile amputation during ritual neonatal circumcision and successful replantation using postoperative leech therapy. Urology 2014;84:472-4. [Crossref] [PubMed]
- Biswas G. Technical considerations and outcomes in penile replantation. Semin Plast Surg 2013;27:205-10. [Crossref] [PubMed]
- Riyach O, El Majdoub A, Tazi MF, et al. Successful replantation of an amputated penis: a case report and review of the literature. J Med Case Rep 2014;8:125. [Crossref] [PubMed]
- Krishnakumar KS, Petkar KS, Lateef S, et al. Penile replantation. Indian J Plast Surg 2013;46:143-6. [Crossref] [PubMed]
- Li GZ, He F, Huang GL, et al. Penile replantation: report of two cases and review of the literature. Chin J Traumatol 2013;16:54-7. [PubMed]
- Burt FB, Schirmer HK, Scott WW. A new concept in the management of priapism. J Urol 1960;83:60-1. [Crossref] [PubMed]
- Mineo M, Jolley T, Rordriguez G. Therapy in penile replantation: a case of recurrent penile self-amputation. Urology 2004;63:981-3. [Crossref] [PubMed]
- Essid A, Hamzaoui M, Sahli S, et al. Glans reimplantation after circumcision accident. Prog Urol 2005;15:745-7. [PubMed]
- Virasoro R, Tonkin JB, McCammon KA, et al. Penile Amputation: Cosmetic and Functional Results. Sex Med Rev 2015;3:214-22. [Crossref] [PubMed]
- Bai WJ. Efficacy of tadalafil for erectile dysfunction: an updated review. Zhonghua Nan Ke Xue 2007;13:568-72. [PubMed]