Treatment of failed vasectomy reversal using a microsurgical two-layer anastomosis technique
Introduction
Vasectomy is a common urologic procedure in North America and about 0.5 to 1 million men received this operation each year. Due to various reasons, some men who had already received surgical sterilization want to regain their reproductive function and therefore require for the vasectomy reversal. There are some problems in traditional vasectomy. Although both ends of the vas deferens can be sutured together under direct vision or using the surgical loupe mounted on the head, it is difficult to meet the standard of anastomosis. Some tissues may enter the lumen and thus cause luminal stenosis, which affects the normal peristalsis and ejaculation of vas deferens. In our center, the vasectomy reversal was performed on 24 patients with failed vasectomy reversal using microsurgical two-layer anastomosis technique, with satisfactory effectiveness.
Patients and methods
Clinical data
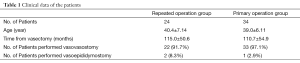
Totally 24 patients, with an average age of 40.4±7.14 years (range, 26 to 55 years), were enrolled in the treatment group. Reasons for vasectomy reversal included: remarried (n=16); unexpected injury or death of their children (n=3); mental disabilities of their children (n=4); and painful nodules after vasectomy (n=1). The average time from the vasectomy to this operation was (115.0±50.6) months (range, 22-222 months). All patients in the treatment group received a second operation after previous failed vasectomy reversal, among whom 17 patients had failed once and 7 patients twice. Testicular biopsy was performed before the operation to confirm whether the testicles had good spermatogenic function. Thirty-four patients who underwent the same surgical procedure for the first time during the same period were selected as the control group. The control group had an average age of (39.0±6.11) years (range, 25-51 years) (P=0.482) and an average time to the vasectomy of (110.7±54.9) months (range, 12-208 months) (P=0.763) (Table 1).
Full table
Surgical maneuvers
All patients underwent epidural anesthesia. The preoperative skin preparation was routinely performed. The patients were in the supine position, with legs apart and scrotum elevated. After the previous anastomosis site was found, the vas deferens was fixed under the skin using the three-finger method. The skin and sarcolemma were then incised in the scar nodules of the previous anastomosis site and the vas deferens was fixed using the vas deferens fixation pliers. The serosa of vas deferens was opened to isolate the scar nodules and the distal and proximal vas deferens, during which the vas deferens and its supplying artery should be carefully protected. The scar nodules were then removed till the normal vas deferens. The two ends of the vas deferens were expanded with a micro forceps under microscope. The proximal vas deferens was squeezed to observe whether there was semen spills; if so, the semen was collected. A 40-time optical microscope was used to check whether there were living sperms. With the surgical trocar latex shell, 5 mL physiological saline was injected into the distal vas deferens without resistance to determine whether the distal vas deferens was unobstructed. The both cut ends were fully dissociated, and the outer connective tissue was fixed with 4-0 absorbable suture. The two ends were pushed together for anastomosis without tension after a relaxation was made. For patients with absence of the proximal vas deferens after the removal of the scar and short vas deferens, the vasoepididymostomy was applied. The full-thickness of vas deferens was sutured with 9-0 PROLENE nonabsorbable suture (Johnson & Johnson medical equipment co., LTD., Ethicon, Inc) under the 16× light microscope without knots for the traction. Discontinuous isometric 3 stitches were done on both sides using the outer-in and inner-out approaches. The knot was tied after one side was sutured and the suture knot was left outside the vas deferens lumen. Then discontinuous 6-stitche method was used to reinforce the serosa of the vas deferens. For the patients undergoing vasoepididymostomy, 9-0 PROLENE 2-suture microsurgical intussusception technique with longitudinal suture placement was adopted. And discontinuous 4 stitches were used to reinforce the vas deferens and serosa of epididymis. The incision was closed layer-by-layer. The scar nodules were removed for pathology. The operation process was shown in Figures 1,2.

The scrotums of patients were elevated after the surgery. Oral antibiotics were administered for 3 days. The surgical site was keep clean and dry by dressing.
Results
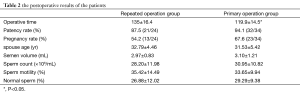
The operations were successful in all patients, with an average duration of (135±16.4) min (range, 100-178 min) in the treatment group and (119.9±14.5) min (range, 94-150 min) in the control group (P=0.000). No significant bleeding was found in both groups, and all patients were discharged from hospital one day after the operation. All the 58 patients were followed up postoperatively for 9 months to 6 years, yielding a follow-up rate of 100%. As shown in the routine semen examination 3 months after the operation, the patency rate was 87.5% (21/24) in the treatment group and 94.1% (32/34) in the control group (χ2=0.7821, P=0.376) (Table 1). There were 13 patients of the reoperation group successfully made the woman pregnant with the pregnancy rate of 54.2% (13/24), while they were 23 patients and 54.2% (13/24) in the control group with no statistical difference (χ2=1.0859, P=0.297), as shown in Table 2.
Full table
Discussion
Vasectomy, the most simple and safe sterilization for males has been widely applied. Due to various reasons, however, some individuals may want to regain their reproductive capability. While vasectomy reversal is one of the most important means for these people, it needs skilled surgical techniques, particularly for some patients admitted in this study who had complex conditions that accepted a second or more operations. The patency rate and the postoperative pregnancy rate of the conventional procedure are not satisfactory. Nevertheless, the introduction of the microsurgical technique undoubtedly brings hope for patients. According to literature review and our own experiences, the success of vas deferens recanalization is related to many factors.
The time interval from vasoligation to recanalization is the most important. A report summarized the result of 747 cases that the patency rate of microsurgical vas deferens recanalization was related to the time interval: a longer interval was associated with lower success rate (3). Fischer reported the similar findings (4). Due to the insufficient sample size of this study, it was different to analyze the time-effect relationship between the vas deferens recanalization and the patency rate. However, we did find that in patients with long time interval, the fibrous scar hyperplasia tended to be more obvious and the operation was more difficult. In addition, some authors have believed that the age of patients were associated with the postoperative recanalization, which might be indirectly explained by the time interval.
The ligation site is also related to the postoperative patency rate. It has been reported that the closer the ligation site was to the epididymis, the lower the success rate was. In the repeated operation group of this study, the operation was more difficult in patients with the lower ligation sites, because a lower ligation site was closer to the epididymis, and the lumen of epididymis became finer. The 24 patients in our repeated operation group had previously undergone the vas deferens recanalization for one or more times, parts of the vas deferens had been removed and the anastomosis site was very close to the epididymis. The vaso-epididymis anastomosis was required in some of them. Therefore, the operation was quite challenging. To ensure the quality of operation, we used oblique cutting and end-to-end vasovasostomy to increase the diameter of anastomosis. Although the microsurgical vaso-epididymis anastomosis has been frequently used for patients with idiopathic obstructive azoospermatism (5-7), the vaso-epididymis anastomosis after the dissociation of the longer epididymal tube was more feasible for patients with failed vasectomy reversal because of the deficiency of the longer vas deferens and even the vas deferens close to the epididymis end. Using the microsurgical intussusception vasoepididymostomy, Chan et al. greatly improve the postoperative pregnancy rate (8). With the continuous improvement of microscopic technology, the microsurgical vaso-epididymis anastomosis has also been upgraded (9). The autologous materials have also been applied for the vasoplasty as alternative materials (10). Using the cryopreservation technology, Naughton et al. used the frozen-thawed vas deferens as the repair material after the cryopreservation and thawing (11). However, these methods have not been well recognized.
The indwelling of vas deferens stent was also used for the vas deferens anastomosis to increase the probability of recanalization (12), which, however, also remains controversial. The vas deferens stent-assisted vasovasostomy has good recent operation effectiveness. However, the vas deferens wall needs to be penetrated and the mucosal layer will be damaged during the stent placement. Therefore, it will increase the probability of lumen blockage and sperm outflow, resulting in poor long-term outcome. The microscopic technique can not only bring good contraposition of the two ends, which has also been widely recognized (13,14).
In terms of the suture layer of the vas deferens recanalization, one-, two-, and three-layer methods have been employed. While the specific implementation remains controversial, studies have shown that the three methods were not significantly different in restoring the continuity of the lumens, especially under the direct vision of the microscope (4,15,16). The two-layer suture was used in all patients in this study. The outer-in and inner-out stitching method was used in the first layer with the full thickness, and the suture knot was tied outside the lumen to reduce the foreign body. The suture of the serosa was for the purpose of reducing the tension to avoid the complications such as semen spills.
Also, the selection of absorbable and nonabsorbable sutures during the surgery also remains controversial (17). The absorption of the absorbable sutures, whether natural or synthetic, is a process of digestion or hydrolysis, which may cause secondary inflammatory reaction and increase the risk of vas deferens restenosis. The nonabsorbable RROLENE suture was used in all the cases in this study. The polypropylene suture has been widely used in cardiovascular, plastic, and ophthalmologic surgeries. The biological activity of the suture is weak, with light tissue reaction. It will not easily stick to the tissue, and therefore has more advantages for the patients with scar constitution or tissue hypertrophy. More importantly, as a single-fiber suture, it encounters less resistance when passing through the tissue and causes less damage to the vas deferens. Also, it can prevent the attachment of bacteria, minimizing the postoperative complications.
The postoperative pregnancy rate is most concerned by patients. It has been proposed that the postoperative monitoring of the antisperm antibody is particularly important since the antisperm antibody influences the final pregnancy rate (3,18). Gerrard et al. has proposed that there was a close relationship between the postoperative pregnancy rate and the age of sexual partner (19); in this study, however, it was difficult to analyze the time-effect relationship between the age of sexual partner and the postoperative pregnancy rate due to the insufficient sample size. Literature review and our clinical experiences have shown that most patients who have undergone the vasectomy reversal can give birth. In our center, testicular biopsy is performed before the recanalization to determine that the testicular spermatogenetic function is good. While normal sperms can be detected in most patients during the postoperative routine semen examination, the postoperative pregnancy rate remains relatively low. Therefore, the anatomical recanalization is far from sufficient. Studies have shown that the vasoligation or acquired obstruction had irreversible impact on the functions of the testicle and epididymis (20).
Our study had some limitations. For example, it was not a prospective study, and, as a clinical study, larger sample size is needed.
Conclusions
The microsurgical two-layer anastomosis technique is a good operation method. It can provide satisfactory patency rate for patients with a previous failed vasectomy reversal, which is comparable with the results of patients who had undergone primary procedure. However, prospective studies with large sample sizes are needed to verify the results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Li B, Chen G, Wang X. Microsurgical vasovasostomy. Asvide 2014;1:196. Available online: http://www.asvide.com/articles/208
- Li B, Chen G, Wang X. Microsurgical vasoepididymostomy. Asvide 2014;1:197. Available online: http://www.asvide.com/articles/209
- Bolduc S, Fischer MA, Deceuninck G, et al. Factors predicting overall success: a review of 747 microsurgical vasovasostomies. Can Urol Assoc J 2007;1:388-94. [PubMed]
- Fischer MA, Grantmyre JE. Comparison of modified one- and two-layer microsurgical vasovasostomy. BJU Int 2000;85:1085-8. [PubMed]
- Kumar R, Mukherjee S, Gupta NP. Intussusception vasoepididymostomy with longitudinal suture placement for idiopathic obstructive azoospermia. J Urol 2010;183:1489-92. [PubMed]
- Peng J, Yuan Y, Zhang Z, et al. Patency rates of microsurgical vasoepididymostomy for patients with idiopathic obstructive azoospermia: a prospective analysis of factors associated with patency--single-center experience. Urology 2012;79:119-22. [PubMed]
- Zhao L, Deng CH, Sun XZ, et al. A modified single-armed technique for microsurgical vasoepididymostomy. Asian J Androl 2013;15:79-82. [PubMed]
- Chan PT, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int 2005;96:598-601. [PubMed]
- Chan PT. The evolution and refinement of vasoepididymostomy techniques. Asian J Androl 2013;15:49-55. [PubMed]
- Artyukhin AA. Deferent duct plasty from autologous testicular vaginal tunica propria on an arteriovenous pedicle. Bull Exp Biol Med 2007;143:479-82. [PubMed]
- Naughton CK, Thomas AJ Jr. Optimizing laboratory use of human vas deferens specimens for microsurgical practice. Urology 2002;60:320-3. [PubMed]
- Kolettis PN. Restructuring reconstructive techniques--advances in reconstructive techniques. Urol Clin North Am 2008;35:229-34. viii-ix. [PubMed]
- Schwarzer JU, Steinfatt H. Current status of vasectomy reversal. Nat Rev Urol 2013;10:195-205. [PubMed]
- Herrel L, Hsiao W. Microsurgical vasovasostomy. Asian J Androl 2013;15:44-8. [PubMed]
- Hsieh ML, Huang HC, Huang ST, et al. Loupe-assisted modified one-layer vasovasostomy. Arch Androl 2005;51:141-8. [PubMed]
- Elzanaty S, Dohle GR. Vasovasostomy and predictors of vasal patency: a systematic review. Scand J Urol Nephrol 2012;46:241-6. [PubMed]
- Fallick ML, Sable DB, Faller G, et al. Histological evidence of an inflammatory reaction to suture material in the dog vas deferens. Br J Urol 1997;79:70-3. [PubMed]
- Amarin ZO, Obeidat BR. Patency following vasectomy reversal. Temporal and immunological considerations. Saudi Med J 2005;26:1208-11. [PubMed]
- Gerrard ER Jr, Sandlow JI, Oster RA, et al. Effect of female partner age on pregnancy rates after vasectomy reversal. Fertil Steril 2007;87:1340-4. [PubMed]
- Li BK, Wang X, Liu CX, et al. Influence of reproductive tract obstruction on expression of epididymal proteins and their restoration after patency. Asian J Androl 2013;15:105-9. [PubMed]


