Contemporary management of ejaculatory dysfunction
Introduction
Ejaculatory dysfunction is the most common form of sexual dysfunction experienced by men (1). Ejaculatory dysfunction covers a broad range of disorders including premature ejaculation (PE), anejaculation, painful ejaculation, and hematospermia. This report will review the anatomy and physiology of normal ejaculation, investigate the pathophysiologic processes explaining disorders of ejaculation and subsequently discuss the strategies currently utilized to manage such disorders (2).
Ejaculatory dysfunction has a wide range of severity as symptomatology varies based on subjective interpretation by the patient. Moreover, there is no standard characterization of symptom bother as an unbearable change in sexual function to one man may be of little bother to another. The term dysfunction is thus reserved for ejaculatory issues that cause significant distress to the patient.
Epidemiological studies performed in the US and Europe estimate that upwards of 30% of males have experienced ejaculatory dysfunction (3). However, due to the sensitive nature of this topic, this figure likely underestimates the true prevalence. The most commonly reported disorder experienced by men is PE followed by delayed and painful ejaculation (3,4).
Normal ejaculatory function
Any discussion of ejaculatory dysfunction first requires an understanding of the normal anatomy and physiology. Male sexual response is a complex, delicately orchestrated process involving erection, ejaculation and orgasm, and detumescence.
Innervation
The penis is innervated by a complex system of somatic and autonomic nerve fibers that mediate sexual response (5). The dorsal nerve branches from the pudendal nerve to provide somatic innervation to the penis. Tactile stimulation is transmitted retrograde to the spinal cord to initiate a reflex arc that initiates and maintains an erection. The dorsal nerve also mediates contraction of the pelvic floor muscles to achieve rigidity and plays a role in discharging ejaculatory fluid.
Autonomic innervation via the cavernous nerves mediates both erection and ejaculatory functions (6,7). Parasympathetic fibers originating from S2–4 travel alongside the pelvic nerve until it branches to pass laterally along the prostate. These nerve fibers then project through the urogenital diaphragm to the corporeal bodies, where they promote tumescence via acetylcholine-mediated vasodilation of the penis. Sympathetic fibers arising from T11–L2 travel to the penis via inferior mesenteric, hypogastric, and pelvic nerve plexuses to promotes emission and ejaculation via contractions of the vas deferens, ampulla, seminal vesicles, prostate and bladder neck (2,7).
Emission phase of ejaculation
Ejaculation can be split into two distinct phases: emission and expulsion (8). Emission is the deposition of semen and the associated products into the posterior urethra. The organs involved in this phase include the epididymis, vas deferens, seminal vesicles, prostate gland, prostatic urethra, and bladder neck. Sympathetic innervation leads to the release of oxytocin (9), neuropeptide Y (10), vasoactive intestinal polypeptide (10-12), and nitric oxide (11). These neurotransmitters subsequently stimulate smooth muscle cell contraction within the aforementioned organs leading to the sequential release of their excretions into posterior urethra.
Peripheral vs. central neural control of emission
Peripherally, retrograde sensory currents are delivered from the dorsal nerve of the penis to the pudendal nerve, which then integrates with the hypogastric plexus. Emission is ultimately stimulated as these nerves deliver their signal to the cerebrum (8). Isolated lesions affecting the hypogastric nerves serve to illustrate their crucial role in the control of emission. For example, ejaculatory dysfunction secondary to manipulation of the nerve plexus is a common sequela of para-aortic lymph node dissections (8,13). In addition, electric stimulation of the superior hypogastric plexus in paraplegic men has been reported to cause seminal emission (13).
The emission phase is under considerable cerebral control and may be elicited following visual and physical erotic stimulations (14). Associated with this phase is the closure of the bladder neck to prevent retrograde ejaculation, which is mediated by sympathetic control from T10–L2 (15).
Expulsion
Expulsion is the next phase of the ejaculatory sequence and describes the ejection of seminal fluid out of the urethra. This is facilitated in an antegrade fashion by rhythmic contractions of the bulbospongiosus and ischiocavernosus muscles. Expulsion is primarily controlled by the somatic nervous system from S2–4 nerve roots (16) with nominal input elicited through an involuntary sympathetic spinal cord reflex (17).
Somatic control of the expulsion phase is often associated with a distinct sensation that most men experience as orgasm (18). However, it is necessary to acknowledge that orgasm and ejaculation are technically separate and distinguishable events governed by unique processes. Orgasm is the cerebral processing of sensory stimuli from the pudendal nerve related to the pleasurable sensation associated with the contraction of the bulbospongiosus and ischiocavernosus muscles, and the urethral bulb (17,19). Ejaculation is the physical expulsion of semen and associated products from the urethra.
Central control of ejaculation
The process of ejaculation is also influenced by the central nervous system. Many neurotransmitters have been found to be involved, including dopamine, norepinephrine, serotonin, acetylcholine, oxytocin, GABA, and nitric oxide (7,11,16). However, dopamine and serotonin have emerged as the essential neurochemical factors, with dopamine facilitating ejaculation (20) and serotonin primarily playing an inhibitory role (20-22).
The dopaminergic system, particularly in the anterior hypothalamus, promotes seminal emission and/or ejaculation via D2 and D3 receptors (23-26). Dopaminergic stimulation also appears to increase a number of sexual behaviors such as libido and erections (23,27).
On the other hand, serotonin (5-HT) is primarily inhibitory. Animal studies in male rats show stimulation of 5-HT (2C) receptors increases erections and inhibits ejaculation (28). However, stimulation of 5-HT (1A) receptors actually has the opposite effect by facilitating ejaculation and inhibiting erections (28). This dichotomy has led to the emerging hypothesis that men with PE may have hyposensitivity of 5-HT2C and/or hypersensitivity of the 5-HT1A receptor (21,29).
Disorders of ejaculation
PE
PE is the most common ejaculatory disorder. It can be either lifelong—presenting from the first sexual encounter onward—or acquired (21). Due to discrepancies in definition of what constitutes PE, the reported prevalence varies markedly 3–75% (30,31). However, the true prevalence is estimated to be 20–30% worldwide (32).
Inconsistency in the definition of PE recently led the International Society for Sexual Medicine (ISSM) and the DSM-V to attempt a standardized definition for lifelong PE based on the results of two, multi-national population-based studies (3,33,34). Both studies asked men to use a stopwatch to time their typical coital episodes. The average intravaginal ejaculation latency time (IELT) was found to be 5.7 minutes. By invoking the statistical principle of two standard deviations below the mean as abnormal, they determined that the IELT cutoff for PE was approximately 1 minute. In addition to this objective criterion, the DSM-5 and ISSM definitions specify that the inability to delay ejaculation must result in negative personal consequences, or distress (35,36). DSM-5 further specifies that the patient must experience the disorder 75–100% of the time over the course of at least 6 months (35). Analogous studies determining the IELT for acquired PE do not exist; however the ISSM definition based on a consensus of expert opinions defines an IELT reduction to less than 3 minutes as an appropriate threshold for acquired PE (36).
Although the prevalence of PE is approximately 20–30%, significantly more men (30–60%) will self-report distressing early ejaculation (37). These men may not meet modern criteria for PE but may benefit from support and education.
Evaluation of PE
History and physical
The diagnosis of PE is based off a thorough sexual history. The specific etiology of PE is unknown, but a multitude of risk factors have been identified including: depression/anxiety, psychological difficulties, hypersensitivity of the glans, over-representation of the pudendal nerve in the cortex, abnormal serotonin neurotransmission in the brain, baseline erectile difficulties, prostatitis, metabolic syndrome and physical inactivity, recreational drug use chronic pelvic pain, and thyroid dysfunction. These risk factors should be evaluated in the history (38-50).
A physical exam can be used to assess for risk factors and causal diseases, but is not mandatory (51). If the patient has concomitant erectile dysfunction, he should be evaluated either by history or with a validated instrument such as Index of Premature Ejaculation, Premature Ejaculation Profile (PEP), or the Premature Ejaculation Diagnostic Tool (52,53). Laboratory or imaging studies are rarely required, but are occasionally indicated based upon the patient’s medical history (e.g., if there is suspicion of hyperthyroidism or prostatitis). About 30 percent of men with PE have concurrent ED, which typically results in early ejaculation without full erection (48,54,55).
Treatment for PE
There are several treatment modalities available for PE. Non-pharmacologic strategies include psychotherapy and behavioral modification (56). Medication options (Table 1) are widely available, but most are used off-label.
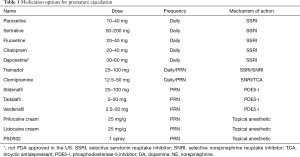
Full table
Psychotherapy and behavioral modification
The primary goal of psychotherapy in the treatment of PE is to address underlying psychological issues such as anxiety, loss of self-confidence or interpersonal tensions that may have predisposed to the development of this disorder (56). Dedicated psychologists or sex therapists often lead this therapy, which can be conducted in an individual, couples or group setting. Behavioral treatments such as the squeeze or stop-start techniques commonly supplement psychotherapy efforts (57). These techniques function to help men recognize mid-level ranges of excitement prior to ejaculatory inevitability with contraction of the pelvic muscles, or a pause in movement, facilitating a decrease in stimulation. In theory, these modifications lead to a gradual increase in IELT, sexual confidence, and self-esteem (57). Unfortunately, support for the use of psychotherapy or behavioral therapy is limited by a lack of well-designed studies. In 1971, after a 5-year follow-up, Masters and Johnson in 1971 reported failure rates as low as 2.7% in patients utilizing a combination of behavioral techniques and communication training (57). A more modern case-control study of 18 couples found an 8-fold increase in IELT among men treated with behavioral techniques (58).
Medications
Selective serotonin reuptake inhibitors (SSRI)
The use of SSRIs revolutionized management of PE is now considered to be first line treatment (17). These medications block the reuptake of serotonin from the synaptic cleft of central serotonergic neurons by 5-HT transporters, resulting in elevated levels of 5-HT neurotransmission and stimulation of postsynaptic membrane 5-HT receptors (17). As such, SSRIs exploit the inhibitory effect of serotonin on ejaculation thereby promoting longer IELT.
Many drugs in this class have been trialed for use in PE. Daily treatment with paroxetine 10–40 mg, sertraline 50–200, fluoxetine 20–40 mg, and citalopram 20–40 mg are effective, safe, and well tolerated (59-64). Paroxetine has been to shown be the most efficacious by increasing IELT approximately 8.8-fold over baseline (65-67).
These medications can be administered on-demand 4–6 hours prior to intercourse; however, ejaculatory delay is significantly lower with daily treatment and more easily facilitates spontaneous intercourse (37,68). A preference study of SSRIs for lifelong PE revealed that 81% of patients preferred daily use while 16% preferred on-demand (69).
Ejaculation delay usually occurs within 5–10 days of starting treatment with the full effect of therapy potentially reaching its maximum sustained effect after 2–3 weeks (17,70). The dose is titrated according to response and tolerability. Few patients have reported a reduced response after 6–12 months of treatment (70).
Adverse side effects (ASE) are generally minor, occur at the onset of treatment, and resolve in 2–3 weeks. They include fatigue, yawning, mild nausea, diarrhea, or perspiration (68,71). Hypoactive desire and ED are infrequently reported. A small number of patients experience significant agitation and hypomania. Treatment with SSRIs should be avoided in men with a history of bipolar depression (72). Reports of a small increase in the risk of suicidal ideation or suicide attempts in youth suggest that it would be prudent to not prescribe SSRIs to men less than 18 years of age (17). Patients can experience SSRI withdrawal symptoms, including dizziness, headache, nausea, vomiting, diarrhea, and irritation, and should be advised to avoid sudden cessation or rapid dose reduction (71,73).
Clomipramine
Clomipramine is a tricyclic antidepressant also used off-label for PE. It predates SSRI development, but due to a higher ASE profile it is now considered second-line therapy. It may be taken daily or on demand 2–6 hours prior to intercourse with doses ranging from 12.5–50 mg/day (51).
As a TCA/serotonin-norepinephrine reuptake inhibitor (SNRI), clomipramine increases levels of centrally acting serotonin (74). In a randomized, double-blind placebo-controlled trial of 100 patients, clomipramine administered at doses of 15 or 30 mg both significantly increased IELT as compared to placebo. One study showed an increase of IELT from 2 to 8 minutes (75).
Common ASEs associated with clomipramine include: dry mouth, constipation, loss of appetite, sleepiness, weight gain, sexual dysfunction, and trouble urinating (76,77). The most serious ASEs include an increased risk of suicidal behavior in those under the age of 25, seizures, mania and liver problems. If stopped suddenly, a withdrawal syndrome may occur with headaches, sweating, and dizziness (76). ASEs overall are experienced in up to 57% of patients, with less ASEs experienced patients taking a 15 mg dose (78).
Dapoxetine
Dapoxetine is the first pharmaceutical approved specifically for the treatment of PE internationally, though it has not yet received FDA approval in the United States. As a short half-life SSRI, it has the notable benefit of better efficacy with on-demand use. It is rapidly absorbed and eliminated, with minimal accumulation and no withdrawal symptoms after abrupt discontinuation (79-81).
Dapoxetine use for PE is supported by five randomized, double-blind, placebo-controlled trials in over 6,000 men (74). Collectively these studies revealed a significant increase in IELT in a dose dependent fashion as compared to placebo. Notably, it was observed that compared to an average pre-treatment IELT of 0.9 minutes, administration of 30 and 60 mg of dapoxetine increased IELT to 3.1 minutes and 3.6 minutes, respectively. Patient questionnaires indicated improved ejaculatory control, decreased distress, and increased satisfaction in their sexual encounters. It was also similarly effective and well-tolerated in men with PE and ED when combined with the use of phosphodiesterase-5 inhibitors (PDE5i) (74).
Treatment related ASEs were uncommon, dose-dependent, and largely mild to moderate in severity. The most common events were nausea (11.0–22.2%), dizziness (5.9–10.9%), and headache (5.6–8.8%) (74). Severe or serious ASEs occurred infrequently (≤3%) and included syncope.
Tramadol
Tramadol has been used off-label for the treatment of PE (82). It is a centrally acting mu-receptor opioid receptor agonist, though its efficacy in treating PE is attributed to its well-established SSRI and weak serotonin-norepinephrine receptor inhibitor (SNRI) activities (83,84). It can be used daily or on demand with similar efficacy, although patients report more satisfaction with on-demand use (85).
A 2012 RCT of tramadol for PE demonstrated a 2.5 fold increase in IELT from a baseline of 72 seconds (86). Investigators found 53.6% and 85.6% of patients reported subjective improvements in IELT when treated with 50 and 100 mg of tramadol, respectively, compared to 2.4% of those managed with placebo.
A meta-analysis of seven trials showed that tramadol was associated with a 3-minute increase in IELT (mean difference 2.77 minutes; 95% CI, 1.12–4.47; P=0.001) (84). Notably, there were no differences between tramadol and paroxetine on IELT. Patients also reported significantly greater satisfaction with tramadol (84). Another meta-analysis of eight trials had similar results but was limited by heterogeneity amongst the individual studies (87). Doses from 25–100 mg have been tested and determined to be safe and effective (85).
The most common ASEs are somnolence and GI distress (87). One study showed tramadol was associated with more ASEs than the SSRI paroxetine (88), although overall ASEs were rare. Reported ASEs include post-micturition dribble, erectile dysfunction, constipation, nausea, headache, somnolence, dry mouth, dizziness, pruritus, and vomiting (87). Tramadol is considered to have a low abuse potential as compared to traditional opioids (89,90).
In practice, tramadol is not often as a first line treatment for PE, but is an option once patients have failed alternative therapies (17). Concern for addiction seems to be a deterrent for prescribers; however, no data substantiates such fear. In a trial involving over 8,000 patients with chronic pain on tramadol, the rate of abuse with tramadol was 2.7%, similar to the rate of NSAIDS abuse (2.3%), and less than that of oxycodone (4.9%) (89).
PDE5 inhibitors
PDE5i’s have been used in treatment of PE with mixed results. Two systematic reviews including at least 14 studies suggest that PDE5i’s are significantly more effective than placebo at increasing IELT (91,92). However, sildenafil failed to significantly increase baseline IELT in men with lifelong PE in a RCT (92). There was, however, a small improvement in IELT in the subset of men with concomitant ED.
Topical local anesthetics
Under the premise that PE may result from glans sensitivity, topical anesthetics have been trialed to reduce glans sensitivity, thereby inhibiting input into the spinal reflex arc that controls ejaculation (44). Topical local anesthetics include lidocaine or prilocaine as a cream, gel, or spray (17,93).
A double blind, randomized, placebo-controlled study of 42 men showed a significant increase in the mean IELT, from 1.49 to 8.45 minutes (P<0.001), in men using a lidocaine-prilocaine cream. A second RCT demonstrated similar results. In this study, PSD502 applied topically to the glans penis 5 minutes before intercourse showed significantly improved ejaculatory latency, ejaculatory control, sexual satisfaction and distress and was shown to be well- tolerated by patients and partners (94). Side effects were mild and include glans and vaginal numbness and female anorgasmia from transvaginal absorption when no condom was used (93,94).
PSD502 is a novel compound of lidocaine-prilocaine delivered as an aerosolized metered spray. PSD502 has received marketing approval in Europe but is not yet available in the United States (93). Its novel design allows only shallow penetration into the mucosa of the glans penis, and therefore the keratinized skin of the shaft is not affected. There are also minimal reports of transfer to partners due to the unique formulation.
Combined psychological and pharmacological treatment for PE
The combined use of medical and psychological interventions harnesses the power of both therapies to provide patients with PE rapid symptom improvement. There are three studies reporting on combined pharmacological and behavioral treatment for PE (95-97) and one study reporting on consecutive treatment with pharmacotherapy followed by behavior therapy (98). Each study used a different medication, sildenafil, citalopram, clomipramine, or paroxetine, but all show combination therapy as superior to pharmacotherapy alone in lengthening IELT.
DE, anejaculation, and anorgasmia
DE, anejaculation, and anorgasmia are among the least common and least understood male sexual health dysfunctions. The estimated prevalence of DE is 1–4% of the male population (99). These disorders are thought of as related entities on one end of a spectrum, with PE on the other end of the spectrum (100). DE can cause significant distress to the male and low satisfaction with partner, and is particularly problematic when procreation is a goal. As with PE, the definition of DE is nebulous, but clinicians may use an IELT greater than two standard deviations above average (5.4 minutes), which is roughly 22–25 minutes (36,100).
Anejaculation is the complete failure to achieve emission despite adequate stimulation. Men who cease sexual interaction given irritation, exhaustion, or partner request are also placed in the category (54). The patient must experience personal distress to classify this as a disorder (35,101). As mentioned in the introduction, there is a distinction between ejaculation and orgasm, but the vast majority of men will present with a complaint of combined inability to ejaculate or orgasm. In this section, “delayed ejaculation” will often refer to both delayed and complete anejaculation.
Delayed or anejaculation may be lifelong or acquired, situational or persistent. As the name implies, lifelong sufferers have always had difficulty with ejaculation, while acquired issues develop after prior “normal” ability to ejaculate. Situational DE is where the patient is able to ejaculate in some instances, but not others. Often, this is stress or anxiety induced (102). Total anejaculation is the condition where the man is never able to ejaculate semen consciously, either during intercourse or by masturbation.
Causes of DE
DE has many potential causes. First, it can simply be seen with inadequate sexual stimulation, which can be due to insufficient sexual excitement or an elevated threshold requirement for ejaculation, as seen in men with decreased sensation from penile neuropathy. Men with a history of intense penile self-stimulation (or traumatic masturbation) may have more difficulty achieving orgasm with a partner, due to conditioning and difficulty recreating intensity of stimulation with a partner (102,103).
Psychosocial variables are always important to consider in the setting of DE. Approximately 75% of affected males can achieve ejaculation through solitary masturbation, suggesting a large psychological or environmental influence on DE (104). Relationship stress, feuding, and conflict may all compromise sexual responses and inhibit achievement of orgasm and ejaculation (103,105).
Anything that interferes with the mechanisms of ejaculation described previously (damage to central control of ejaculation, the peripheral sympathetic nerve supply to the vas/bladder neck, the somatic efferent nerve supply to the pelvic floor or the somatic afferent nerve supply to the penis) can result in DE (104). From a medication standpoint, the most well-known cause is the anti-depressant class (SSRIs) which increase the amount of circulating serotonin, an ejaculatory inhibitor (47,106). Many medications including MAO-I, tricyclic antidepressants, antipsychotics with alpha antagonist activity (chlorpromazine, haloperidol) (107), opioids (40), benzodiazepines, ethanol (40,108), alpha antagonists (doxazosin, prazosin) (1) have been implicated in delayed and anejaculation.
Medical diseases including diabetic or alcoholic neuropathy, hypothyroidism (42,109), low testosterone (110,111), and even strokes have also been linked to impairment of orgasm (112).
Anatomically, damage to pelvic nerves (following prostatectomy, RPLND, TURP, bladder neck incision, or other colorectal or pelvic surgery), and spinal cord injuries may also cause DE (17,99,100,105,113,114).
Workup and evaluation
Evaluation of men presenting with DE should include a full medical and sexual history, focusing on evaluating risk factors (medications especially SSRIs, antipsychotics, drug use, ED, diabetes, depression, LUTS, low serum testosterone, penile sensory loss, idiosyncratic masturbation). Then, a focused physical examination to evaluate testes, epididymis, and vas, and a DRE should be performed. Additional investigations such as serum testosterone should be pursued as indicated. It is also important to establish whether ejaculation is absent or actually retrograde, with the presence of spermatozoa in post-ejaculation first void urine indicating retrograde ejaculation (104).
Treatment of DE
Treatment of DE should be tailored to the etiology if known. Otherwise, treatment should proceed in a step-wise fashion. Discontinuation of drugs known to interfere with orgasm, as listed above, is the first step (41,115). Modification of therapy regimens may also be advisable. For example, if the patient takes an SSRI for depression, consider a trial of bupropion, which is less likely to cause DE (71,116).
Optimizing erectile function with PDE5-I, vacuum devices, or injections as poor erectile function can contribute to DE (103). Individuals and couples should experiment with various forms of sexual stimulation, such as manual stimulation of the penis or perineum, oral sex, use of lubricants or vibrators, or change in position, as this additional stimulation may trigger orgasm (103).
Psychosexual therapy
Given the large psychosocial component of DE, referral to a sexual therapist can be helpful to evaluate and treat psychological or behavioral or relationship issues. Psychosexual therapy can be particularly helpful in primary inhibited orgasm (117), when it is not due to a medication, medical disease, or surgical side effect.
Pharmacologic treatment
There has been limited success with pharmacologic therapies for the treatment of DE. Cabergoline and bupropion are the two most commonly trialed medications (Table 2), though neither has been approved by the FDA for DE.

Full table
Cabergoline is a potent dopamine receptor agonist. By increasing dopamine neurotransmission, it is thought to promote ejaculation. One study found that cabergoline (0.5 mg twice/week) in the treatment of 72 anorgasmic men showed improvement in 69% of men (118). In another study of 131 men with orgasmic disorders treated with cabergoline, 66% reported subjective improvement, and this was regardless of testosterone status (119).
Bupropion, which blocks the reuptake of both norepinephrine and dopamine, is commonly used as an agent in depressed men when SSRIs cause delayed or anejaculation (71). Much less about its efficacy in non-depressed men, but a pilot study of 10 men with DE treated with Bupropion showed significant improvements over baseline in overall sexual satisfaction, ability to achieve an erection, and ability to achieve orgasm/ejaculation in 70% of patients (116). Researchers continue to pursue medications that increase neurotransmitters in the brain that promote ejaculation (dopamine or oxytocin) (20,113) or decrease inhibitory neurotransmitters (serotonin) (22,120) to treat this disorder.
Some case reports have suggested that intranasal oxytocin (121,122), amantadine (120), and cyproheptadine may be candidates (120,123,124). However, evidence is extremely limited.
Hormonal treatment
Testosterone replacement has been evaluated as a potential treatment of DE. Not only does testosterone play a large role in male desire, but testosterone deficiency was shown to decrease dopamine in rat models, which was reversible with testosterone supplementation (125). Although some evidence suggests an association between hypogonadism and DE, testosterone replacement has not translated to improved DE or MSHQ-EDSF scores in several RCTs (111,126).
Special cases
Spinal cord injury
Delayed or anejaculation due to spinal cord injury is dependent upon the level and completeness of the injury (104). The ability to ejaculate increases with descending levels of spinal injury (113). This is because there are three forms of erections: psychogenic (from thinking of something arousing), reflexogenic (from direct touch or stimulation), and spontaneous (from full bladder). The nerves controlling psychogenic erections are located at T11–L2, while those governing a reflexogenic or spontaneous erection are controlled by S2–S4. In a patient with a high spinal cord injury (above T11), the message from the brain cannot get through the damaged part of the spinal cord and create an erection, and loss of psychogenic erections occurs, though they may still be able to achieve reflexogenic or spontaneous erection (127,128). Less than 5% of patients with complete upper motor neuron lesions retain the ability to ejaculate (129). With a lesion below T11, ejaculation rates are higher. Approximately 22% of patients with an incomplete upper motor neuron lesion and almost all men with incomplete lower motor neuron lesions retain the ability to ejaculate (127,130).
Also, in general, the ability to experience erections is preserved more frequently than the ability to experience ejaculation, as up to 95% of men with spinal cord injury experience ejaculatory problems (129), but 80% regain some erectile function by 2 years after injury (128).
Fertility and anejaculation
All men undergoing pelvic surgery should be counseled on the potential side effects including anejaculation/retrograde ejaculation, and should be given information on sperm banking if future fertility is desired (17).
If an anejaculatory male is trying to achieve fertility, consider an alpha agonist (131,132). Alpha agonists may convert anejaculation to retrograde ejaculation which allows sperm retrieval from the urine.
If the above do not resolve the problem, penile vibratory stimulation has been described as an adjunct treatment option for DE (113,133). The vibrator works by providing a high intensity stimulus to the perineum or penis. This stimulus is strong enough to overcome any psychological or situational inhibition and trigger the orgasmic reflex. Another option is electro-ejaculation, which involves direct electrical stimulation of the nerves to the seminal vesicles and vas to elicit ejaculation, but requires general anesthesia. This is often used in patients with spinal cord injuries (127). If this does not work, sperm can be retrieved directly from the epididymis or testis (MESA, TESE) and used for ICSI (134).
Unsatisfactory sensations of ejaculation
Painful ejaculation
Painful ejaculation (aka dysejaculation, dysorgasmia) is a poorly understood phenomenon of sexual dysfunction. It is defined as penile, perineal, scrotal, or testicular pain during or shortly after ejaculation. The prevalence is estimated around 1–10% in the general population (135); however, in patients that suffer from chronic pelvic pain/chronic prostatitis, this percentage increases to 30–75% (136). Symptoms range from minor discomfort to excruciating pain, and may last from 2–24 hours depending on the patient (137,138).
There are many potential causes of painful ejaculation, and though few are life threatening, these issues can cause a significantly decreased quality of life. The most common etiology is infectious/inflammatory processes including orchitis, epididymitis, prostatitis, or urethritis (135,139). Obstructive disease can also cause pain due to forceful pressure when seminal fluid meets resistance, including a urethral stricture, vasal obstruction after a vasectomy or radical prostatectomy. Occasionally inguinal hernia repair with mesh can cause kinking or scarring of the vas deferens or nerve compression. Less common etiologies are ejaculatory duct obstruction or seminal vesicle calculi.
Work-up these patients include a full history and physical with exam of the genitals and DRE for prostate. Obtain a urinalysis, urine culture, and STI panel. Treat infectious or inflammatory processes with antibiotics and NSAIDS. After inflammatory and infectious causes treated or ruled out, the provider may elect to pursue specialized tests depending on the clinical picture. Consider PSA in patients at risk for prostate cancer. If the patient recently underwent a radical prostatectomy, one study showed that 11% of men complain of painful orgasm afterwards, with an increased risk in those who underwent a bilateral seminal-vesicle sparing approach (140). Counsel the patient that in these instances, pain usually resolves in 12–18 months (140). Consider transrectal ultrasound to check for ejaculatory duct obstruction or calculi and treat with transurethral or endoscopic measures if needed. Consider cystoscopy to evaluate urethral stricture if possible etiology, though these patients would likely have associated LUTS or urinary symptoms. Lastly, the physician may consider an ilioinguinal nerve block to evaluate etiology of pain from nerve compression due to mesh or neuropathy (139,141) .
Pleasure dissociative orgasmic dysfunction/ejaculatory anhedonia
Ejaculatory anhedonia is the experience of normal ejaculation without pleasure or orgasm. Patients experience sexual stimulation and achieve erection, but the connection in the brain which registers these sensations as pleasure is missing. This disorder is quite rare and therefore poorly studied; however, experts believe anorgasmia is due to neurohormonal imbalance in the brain, namely decreased dopamine levels. Proposed etiologies include diminished libido, hormonal or metabolic imbalances (e.g., pituitary, thyroid or testicular dysfunction) (36), psychological disturbances, or medications.
Evaluation should include a detailed history and physical. Consider screening testosterone, thyroid function (TSH), or pituitary hormones (prolactin) to evaluate for occult causes. If it appears the anorgasmia is related to addiction (e.g., opioids, alcohol, heroin), seek appropriate treatment. If due to psychological issues (depression, addiction), consider referral to a psychiatrist and appropriate treatment of condition. If a medical cause cannot be elucidated, referral to a psychologist or sex therapist may provide benefit.
Absent ejaculate (aspermia)
Aspermia, or absent ejaculate, is the condition where no semen is expelled from the penis. There are multiple potential causes including retrograde ejaculation, ejaculatory obstruction, and anejaculation. Here we will focus on retrograde ejaculation.
Retrograde ejaculation
Retrograde ejaculation occurs when there is insufficient bladder neck resistance to the high pressures generated by the bulbospongiosus and ischiocavernosus muscles during ejaculation, leading to redirection of semen into the bladder (142,143). The failure can be mechanical, from disruption during transurethral resection of the prostate; pharmacologic, from alpha antagonism at the bladder neck (alpha blockers, antipsychotics, ganglion blockers); or neurologic, from disruption of the sympathetic pathways that potentiate bladder neck contracture (retroperitoneal pelvic lymph node dissection, abdominopelvic resection, spinal cord injury, as examples) (132,141). Neurovascular compromise of the sympathetic innervation resulting from long-standing diabetes is another etiology, reflected in the 30% incidence of retrograde ejaculation among diabetics (144).
For the patient, retrograde ejaculation can range from perceived lower volume of ejaculate, to less forceful ejaculate, to complete lack of anterograde ejaculate. The effect on the patient can be reduced satisfaction, reduced fertility, or a combination thereof (132,145).
Retrograde ejaculation should be considered in any patient with aspermia or hypospermia, defined as <2 mL semen volume. Diagnosis is confirmed with post-ejaculation urine analysis demonstrating 10–15 sperm per high powered field (143).
Treatment of pharmacologic retrograde ejaculation involves discontinuing, if able, the offending drug. For other etiologies of retrograde ejaculation, medical therapies are first line despite lack of robust studies supporting their use. Alpha agonists such as pseudoephedrine have been used off-label with the goal of stimulating more robust bladder neck contraction. In a recent prospective trial of 20 men with partial or complete retrograde ejaculation dosed with 60 mg pseudoephedrine every 6 hours the day prior to semen analysis and 2 additional doses the day of semen analysis, 70% of patients demonstrated improvement in semen parameters (146). The tricyclic antidepressant imipramine has also been used alone, as well as in combination with an alpha agonist, with modest success (132,147). Surgical intervention using collagen injection at bladder neck has been described (148-150). A series of injections in type 1 diabetics found a mean 0.7 mL increase in ejaculate volume as well as significant improvements in State-Trait Anxiety Index and Beck Depression Inventory scores (150). For those wishing to conceive and unable to obtain antegrade ejaculation through the above methods, sperm retrieval from urine or TESE are other options (132).
Low volume ejaculate
Low volume ejaculate is primarily a concern seen in men undergoing infertility workups. It is defined as a semen volume <1.5 mL. The most common cause is an incomplete semen collection or inappropriate abstinence before collection (no ejaculation for 72 hours before a collection) (151).
Pathologic causes of low volume ejaculate include retrograde ejaculation (152), anejaculation, hypogonadism (153), ejaculatory duct obstruction, congenital bilateral absence of the vas deferens (CAVD) (154), or urethral stricture (155).
Workup
These men are most often found undergoing infertility workups, though rarely a man will present with a chief complaint of low ejaculatory volume. Most critical is a detailed history and physical exam including genital exam, DRE, and lower extremity neurologic exam (151). With these two tools alone, a clinician will be able to rule out the most common cause, collection difficulties, as well as many anatomic concerns: inguinal/scrotal scars, small volume testes, mid-line prostatic cysts, and absence of the vas deferens.
The next step is to evaluate two properly-collected semen analyses, with a third if the first two are significantly different. Azoospermia suggests ejaculatory duct obstruction, absence of the vas deferens, failure of emission or complete retrograde ejaculation. Absence of fructose and an acidic pH are suggestive of ejaculatory duct obstruction or seminal vesicle pathology (156). Oligo/astheno/teratospermia may signify partial ejaculatory duct obstruction or hypogonadism (151).
Further workup is dependent on presumed cause of low volume ejaculate. Gonadotropin levels (testosterone, LH, FSH) are warranted in men concerned for hypogonadism (153). To evaluate potential retrograde ejaculation, post-ejaculate urinalysis (PEU) is often used. However, it remains controversial as 65% of fertile men (157) and 73–90% of infertile men have some sperm on PEU (151,157). In patients with low-volume ejaculate and azoospermia, transrectal ultrasound is a useful tool to investigate anatomy of the prostate, seminal vesicles and vas deferens and can be used to rule out ejaculatory duct obstruction, CAVD (156). If TRUS is inconclusive and further imaging is desired to evaluate ejaculatory duct or seminal vesicle obstruction, options include magnetic resonance imaging (158), seminal vesicle aspiration (159), and seminal vesiculography (160). In patients with CAVD, genetic screening for cystic fibrosis should be performed. A renal ultrasound can identify ipsilateral renal anomalies in patients with CUAVD. If a neurologic lesion is suspected (e.g., tethered cord causing anejaculation), consult neurology and obtain spinal MRI (151).
Treatment
Treatment varies widely based on etiology. Many of these treatments have been discussed elsewhere in this review, and will be briefly discussed here.
Anejaculation may be amenable to oral therapy, penile vibratory stimulation or electroejaculation. If fertility is desired and the above methods are unsuccessful, PESA or TESE followed by IVF are options (161).
Treatment of ejaculatory duct obstruction with trans-urethral resection of the ejaculatory ducts is extremely effective (156,162). Seminal vesicle/vas deferens malformations (hypoplasia, aplasia, cystic fibrosis) are generally not amenable to surgical reconstruction (151). In patients desiring fertility, sperm retrieval with PESA or TESE and IVF is often required (154).
Hematospermia
Hematospermia, the presence of blood in the semen, is an uncommon condition. Prevalence is difficult to estimate due to its rarity and the fact that most men do not look at their ejaculate (163). Approximately 1% of urologic visits are due to hematospermia (164). Luckily, hematospermia is almost always benign and self-limiting. However, it can be quite distressing to those patients experiencing it. Patients are often worried about sexually transmitted infections or malignancy.
The most common cause of hematospermia in men under 40 years of age is inflammation or infection (prostatitis, urethritis, orchitis, urinary tract infection) (163,164). After infection, trauma to the perineum, prostate or genitals due to sexual activity, cycling, or constipation are possibilities. Much rarer causes include calculi of the seminal vesicle, prostate, bladder, or urethra, cysts of the reproductive organs, obstruction due to urethral stricture, or vascular abnormalities (163,165-167). Rarely, hematospermia may be associated with prostate cancer, but this was seen in less than 0.5% of men (168).
In men over 40, the most common cause is iatrogenic due to prostate biopsy (163,166). Over 80% of men who undergo prostate biopsy have hematospermia that lasts 2–4 weeks (166,169). There may also be an association between hematospermia and prostate cancer. A study of 26,000 men screened for prostate cancer found 14% of the men that reported hematospermia on the initial interview were later diagnosed with prostate cancer (168).
Evaluation
The goal of diagnostic investigation is to detect a clinically relevant or treatable cause of the hematospermia or to exclude malignancy (163). Detailed history and thorough physical examination including genital exam and digital rectal examination are first line. In men <40 with a single episode of hematospermia, send a urinalysis and urine culture, check for sexually transmitted infections (when indicated), and consider a PSA in men at risk for prostate cancer (170).
If concerning factors, recurrent episodes of hematospermia, or men over 40, consider transrectal ultrasound. This is a minimally invasive, inexpensive, and relatively useful study for the organs potentially contributing to hematospermia. One prospective study identified an anatomical correlate as causal factor of hematospermia in a group of over 100 men (166), though biopsies were taken from 10 of these patients and none identified carcinoma. If continued concern, the physician can obtain semen culture, undergo cystoscopy, or obtain a pelvic or endorectal MRI with gadolinium for further imaging.
Treatment
Hematospermia will resolve spontaneously in most men without intervention. Extensive work-up is not warranted in all patients, but should be targeted to those with recurrent hematospermia and risk factors for prostate cancer. When indicated, treat the underlying abnormality (urinary tract infection, prostatitis, excision of urethral stricture). If there is concern for infectious etiology but no pathogen is isolated, a trial of empiric antibiotics is reasonable (163). Cysts of the genital glands or ducts may be aspirated or transurethrally unroofed (164,165). If there is a seminal vesicle or prostatic stone, it may be extracted. In cases of severe, intractable hematospermia, consider treatment with embolization or excision of the bleeding structure in the operating room.
Conclusions
Disorders of ejaculation and orgasm in men are poorly understood. A careful history and physical examination are essential first steps in evaluation. While ongoing research is critical for evaluating further treatments, only a limited number of medical therapies have been advanced as potential solutions for ejaculation disorders. Behavioral and psychotherapy interventions are often helpful in these cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wolters JP, Hellstrom WJG. Current concepts in ejaculatory dysfunction. Rev Urol 2006;8 Suppl 4:S18-25. [PubMed]
- Newman HF, Reiss H, Northup JD. Physical basis of emission, ejaculation, and orgasm in the male. Urology 1982;19:341-50. [Crossref] [PubMed]
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44. [Crossref] [PubMed]
- Rosen R, Altwein J, Boyle P, et al. Lower Urinary Tract Symptoms and Male Sexual Dysfunction: The Multinational Survey of the Aging Male (MSAM-7). Eur Urol 2003;44:637-49. [Crossref] [PubMed]
- Kandeel FR, Koussa VKT, Swerdloff RS. Male Sexual Function and Its Disorders: Physiology, Pathophysiology, Clinical Investigation, and Treatment. Endocr Rev 2001;22:342-88. [Crossref] [PubMed]
- Cherches IM. Clinical neuroanatomy. In: Kass JS. editor. Neurology Secrets: Sixth Edition. Amsterdam: Elsevier, 2016:11-41.
- Giuliano F. Neurophysiology of Erection and Ejaculation. J Sex Med 2011;8:310-5. [Crossref] [PubMed]
- Chéhensse C, Bahrami S, Denys P, et al. The spinal control of ejaculation revisited: A systematic review and meta-analysis of anejaculation in spinal cord injured patients. Hum Reprod Update 2013;19:507-26. [Crossref] [PubMed]
- Filippi S, Morelli A, Vignozzi L, et al. Oxytocin mediates the estrogen-dependent contractile activity of endothelin-1 in human and rabbit epididymis. Endocrinology 2005;146:3506-17. [Crossref] [PubMed]
- Milner P, Crowe R, Burnstock G, et al. Neuropeptide Y- and vasoactive intestinal polypeptide-containing nerves in the intrinsic external urethral sphincter in the areflexic bladder compared to detrusor-sphincter dyssynergia in patients with spinal cord injury. J Urol 1987;138:888-92. [Crossref] [PubMed]
- Domoto T, Tsumori T. Co-localization of nitric oxide synthase and vasoactive intestinal peptide immunoreactivity in neurons of the major pelvic ganglion projecting to the rat rectum and penis. Cell Tissue Res 1994;278:273-8. [Crossref] [PubMed]
- Dail WG, Moll MA, Weber K. Localization of vasoactive intestinal polypeptide in penile erectile tissue and in the major pelvic ganglion of the rat. Neuroscience 1983;10:1379-86. [Crossref] [PubMed]
- Brindley GS, Sauerwein D, Hendry WF. Hypogastric Plexus Stimulators for Obtaining Semen from Paraplegic Men. Br J Urol 1989;64:72-7. [Crossref] [PubMed]
- Baird AD, Wilson SJ, Bladin PF, et al. Neurological control of human sexual behaviour: Insights from lesion studies. J Neurol Neurosurg Psychiatry 2007;78:1042-9. [Crossref] [PubMed]
- de Groat WC, Griffiths D, Yoshimura N. Neural Control of the Lower Urinary Tract. Compr Physiol 2015;5:327-96. [PubMed]
- Coolen LM, Allard J, Truitt WA, et al. Central regulation of ejaculation. Physiol Behav 2004;83:203-15. [Crossref] [PubMed]
- Althof SE, McMahon CG. Contemporary Management of Disorders of Male Orgasm and Ejaculation. Urology 2016;93:9-21. [Crossref] [PubMed]
- Alwaal A, Breyer BN, Lue TF. Normal male sexual function: Emphasis on orgasm and ejaculation. Fertil Steril 2015;104:1051-60. [Crossref] [PubMed]
- Gerstenberg TC, Levin RJ, Wagner G. Erection and Ejaculation in Man. Assessment of the Electromyographic Activity of the Bulbocavernosus and Ischiocavernosus Muscles. Br J Urol 1990;65:395-402. [Crossref] [PubMed]
- Simonsen U, Comerma-Steffensen S, Andersson KE. Modulation of Dopaminergic Pathways to Treat Erectile Dysfunction. Basic Clin Pharmacol Toxicol 2016;119 Suppl 3:63-74. [Crossref] [PubMed]
- Waldinger MD. The neurobiological approach to premature ejaculation. J Urol 2002;168:2359-67. [Crossref] [PubMed]
- Hull EM, Muschamp JW, Sato S. Dopamine and serotonin: influences on male sexual behavior. Physiol Behav 2004;83:291-307. [Crossref] [PubMed]
- Peeters M, Giuliano F. Central neurophysiology and dopaminergic control of ejaculation. Neurosci Biobehav Rev 2008;32:438-53. [Crossref] [PubMed]
- Ferrari F, Giuliani D. Behavioural effects of the dopamine D3 receptor agonist 7-OH-DPAT in rats. Pharmacol Res 1995;32:63-8. [Crossref] [PubMed]
- Eaton RC, Markowski VP, Lumley LA, et al. D2 receptors in the paraventricular nucleus regulate genital responses and copulation in male rats. Pharmacol Biochem Behav 1991;39:177-81. [Crossref] [PubMed]
- Ahlenius S, Larsson K. Effects of the dopamine D3 receptor ligand 7-OH-DPAT on male rat ejaculatory behavior. Pharmacol Biochem Behav 1995;51:545-7. [Crossref] [PubMed]
- Melis MR, Argiolas A. Dopamine and sexual behavior. Neurosci Biobehav Rev 1995;19:19-38. [Crossref] [PubMed]
- Ahlenius S, Larsson K, Svensson L, et al. Effects of a new type of 5-HT receptor agonist on male rat sexual behavior. Pharmacol Biochem Behav 1981;15:785-92. [Crossref] [PubMed]
- Pattij T, De Jong TR, Uitterdijk A, et al. Individual differences in male rat ejaculatory behaviour: Searching for models to study ejaculation disorders. Eur J Neurosci 2005;22:724-34. [Crossref] [PubMed]
- Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med 2009;6:2888-95. [Crossref] [PubMed]
- Jannini EA, Lenzi A. Epidemiology of premature ejaculation. Curr Opin Urol 2005;15:399-403. [Crossref] [PubMed]
- Carson C, Gunn K. Premature ejaculation: Definition and prevalence. Int J Impot Res 2006;18 Suppl 1:S5-13. [Crossref] [PubMed]
- Blanker MH, Bohnen AM, Groeneveld FPMJ, et al. Correlates for erectile and ejaculatory dysfunction in older Dutch Men: A community-based study. J Am Geriatr Soc 2001;49:436-42. [Crossref] [PubMed]
- Serefoglu EC, Mcmahon CG, Waldinger MD, et al. An Evidence-Based Unified Definition of Lifelong and Acquired Premature Ejaculation: Report of the Second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. Sex Med 2014;2:41-59. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). Washington, DC: American Psychiatric Publishing, 2013:280.
- Althof SE, Abdo CHN, Dean J, et al. International Society for Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med 2010;7:2947-69. [Crossref] [PubMed]
- McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. J Urol 1998;159:1935-8. [Crossref] [PubMed]
- Xia Y, Li J, Shan G, et al. Relationship between premature ejaculation and depression A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 2016;95. [Crossref] [PubMed]
- Giuliano F. 5-hydroxytryptamine in premature ejaculation: opportunities for therapeutic intervention. Trends Neurosci 2007;30:79-84. [Crossref] [PubMed]
- Peugh J, Belenko S. Alcohol, drugs and sexual function: a review. J Psychoactive Drugs 2001;33:223-32. [Crossref] [PubMed]
- Seyam R. A systematic review of the correlates and management of nonpremature ejaculatory dysfunction in heterosexual men. Ther Adv Urol 2013;5:254-97. [Crossref] [PubMed]
- Waldinger MD, Zwinderman AH, Olivier B, et al. Thyroid-stimulating hormone assessments in a Dutch cohort of 620 men with lifelong premature ejaculation without erectile dysfunction. J Sex Med 2005;2:865-70. [Crossref] [PubMed]
- Althof SE, Needle RB. Psychological factors associated with male sexual dysfunction: screening and treatment for the urologist. Urol Clin North Am 2011;38:141-6. [Crossref] [PubMed]
- Xin ZC, Choi YD, Rha KH, et al. Somatosensory evoked potentials in patients with primary premature ejaculation. J Urol 1997;158:451-5. [Crossref] [PubMed]
- Colpi GM, Fanciullacci F, Beretta G, et al. Evoked Sacral Potentials in Subjects with True Premature Ejaculation. Andrologia 1986;18:583-6. [Crossref] [PubMed]
- Giuliano F, Clément P. Physiology of Ejaculation: Emphasis on Serotonergic Control. Eur Urol 2005;48:408-17. [Crossref] [PubMed]
- Waldinger MD, Berendsen HH, Blok BF, et al. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: The involvement of the serotonergic system. Behav Brain Res 1998;92:111-8. [Crossref] [PubMed]
- Laumann EO, Paik A, Rosen RC, et al. Erectile dysfunction and premature ejaculation. Guidel Male Sex Dysfunct 2015;281:1-38.
- Screponi E, Carosa E, Di Stasi SM, et al. Prevalence of chronic prostatitis in men with premature ejaculation. Urology 2001;58:198-202. [Crossref] [PubMed]
- Ventus D, Jern P. Lifestyle Factors and Premature Ejaculation: Are Physical Exercise, Alcohol Consumption, and Body Mass Index Associated With Premature Ejaculation and Comorbid Erectile Problems ? J Sex Med 2016;13:1482-7. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An Update of the International Society of Sexual Medicine’s Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex Med 2014;2:60-90. [Crossref] [PubMed]
- Patrick DL, Giuliano F, Ho KF, et al. The Premature Ejaculation Profile: Validation of self-reported outcome measures for research and practice. BJU Int 2009;103:358-64. [Crossref] [PubMed]
- Althof S, Rosen R, Symonds T, et al. Development and validation of a new questionnaire to assess sexual satisfaction, control, and distress associated with premature ejaculation. J Sex Med 2006;3:465-75. [Crossref] [PubMed]
- Patrick DL, Althof SE, Pryor JL, et al. Premature ejaculation: an observational study of men and their partners. J Sex Med 2005;2:358-67. [Crossref] [PubMed]
- Rosen RC, McMahon CG, Niederberger C, et al. Correlates to the clinical diagnosis of premature ejaculation: results from a large observational study of men and their partners. J Urol 2007;177:1059-64; discussion 1064. [Crossref] [PubMed]
- Althof SE. Psychological approaches to the treatment of rapid ejaculation. J Men’s Heal Gend 2006;3:180-6. [Crossref]
- Masters WH, Johnson VE. Human sexual inadequacy. Boston: Little, Brown and Company, 1971:3-4.
- de Carufel F, Trudel G. Effects of a New Functional-Sexological Treatment for Premature Ejaculation. J Sex Marital Ther 2006;32:97-114. [Crossref] [PubMed]
- Abdollahian E, Javanbakht A, Javidi K, et al. Study of the efficacy of fluoxetine and clomipramine in the treatment of premature ejaculation after opioid detoxification. Am J Addict 2006;15:100-4. [Crossref] [PubMed]
- Montorsi F, Guazzoni G, Trimboli F, et al. Clomipramine for premature ejaculation: A randomized, double-blind, placebo controlled study. Acta Urologica Italica 1995;9:5-6.
- Strassberg DS, de Gouveia Brazao CA, Rowland DL, et al. Clomipramine in the treatment of rapid (Premature) ejaculation. J Sex Marital Ther 1999;25:89-101. [Crossref] [PubMed]
- Kara H, Aydin S, Yücel M, et al. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. J Urol 1996;156:1631-2. [Crossref] [PubMed]
- Kim SC, Seo KK. Efficacy and safety of fluoxetine, sertraline and clomipramine in patients with premature ejaculation: a double-blind, placebo controlled study. J Urol 1998;159:425-7. [Crossref] [PubMed]
- Waldinger MD. Towards evidence-based drug treatment research on premature ejaculation: A critical evaluation of methodology. Int J Impot Res 2003;15:309-13. [Crossref] [PubMed]
- McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride. Int J Impot Res 1999;11:241-5; discussion 246. [Crossref] [PubMed]
- Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. Am J Psychiatry 1994;151:1377-9. [Crossref] [PubMed]
- Waldinger MD, Zwinderman AH, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: A randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol 2004;46:510-5. [Crossref] [PubMed]
- Cascade E, Kalali AH, Kennedy SH. Real-World Data on SSRI Antidepressant Side Effects. Psychiatry (Edgmont) 2009;6:16-8. [PubMed]
- Waldinger MD. What do men with premature ejaculationprefer: daily dosing or on-demand drug treatment? Sexologies 2008;17:S44. [Crossref]
- McMahon CG. Long term resuls of treatment of premature ejaculation with selective serotonin re-uptake inhibitors. Int J Impot Res 2002;14:S19.
- Dording CM, Mischoulon D, Petersen TJ, et al. The pharmacologic management of SSRI-induced side effects: A survey of psychiatrists. Ann Clin Psychiatry 2002;14:143-7. [Crossref] [PubMed]
- Marangell LB, Dennehy EB, Wisniewski SR, et al. Case-control analyses of the impact of pharmacotherapy on prospectively observed suicide attempts and completed suicides in bipolar disorder: Findings from STEP-BD. J Clin Psychiatry 2008;69:916-22. [Crossref] [PubMed]
- Black K, Shea C, Dursun S, et al. Selective serotonin reuptake inhibitor discontinuation syndrome: Proposed diagnostic criteria. J Psychiatry Neurosci 2000;25:255-61. [PubMed]
- McMahon CG, Althof SE, Kaufman JM, et al. Efficacy and safety of dapoxetine for the treatment of premature ejaculation: integrated analysis of results from five phase 3 trials. J Sex Med 2011;8:524-39. [Crossref] [PubMed]
- Haensel SM, Rowland DL, Kallan KTHK, et al. Clomipramine and sexual function in men with premature ejaculation and controls. J Urol 1996;156:1310-5. [Crossref] [PubMed]
- Cruz R. Clomipramine Side Effects. J Am Acad Child Adolesc Psychiatry 1992;31:1168-9. [Crossref] [PubMed]
- Beaumont G. Sexual Side-Effects of Clomipramine (Anafranil). J Int Med Res 1977;5:37-44. [PubMed]
- Kim SW, Choi J, Kim S, et al. Tolerability and adequate therapeutic dosage of oral clomipramine for the treatment of premature ejaculation: A randomized, double-blind, placebo-controlled, fixed-dose, parallel-grouped clinical study. Int J Impot Res 2018;30:65-70. [Crossref] [PubMed]
- Hoy SM, Scott LJ. Dapoxetine: In premature ejaculation. Drugs 2010;70:1433-43. [Crossref] [PubMed]
- Lee WK, Lee SH, Cho ST, et al. Comparison between on-demand dosing of dapoxetine alone and dapoxetine plus mirodenafil in patients with lifelong premature ejaculation: Prospective, randomized, double-blind, placebo-controlled, multicenter study. J Sex Med 2013;10:2832-41. [Crossref] [PubMed]
- Dresser MJ, Kang D, Staehr P, et al. Pharmacokinetics of dapoxetine, a new treatment for premature ejaculation: Impact of age and effects of a high-fat meal. J Clin Pharmacol 2006;46:1023-9. [Crossref] [PubMed]
- Waldinger MD. Pharmacotherapy for premature ejaculation. Curr Opin Psychiatry 2014;27:400-5. [Crossref] [PubMed]
- Minami K, Uezono Y, Ueta Y. Pharmacological Aspects of the Effects of Tramadol on G-Protein Coupled Receptors. J Pharmacol Sci 2007;103:253-60. [Crossref] [PubMed]
- Wu T, Yue X, Duan X, et al. Efficacy and safety of tramadol for premature ejaculation: A systematic review and meta-analysis. Urology 2012;80:618-24. [Crossref] [PubMed]
- Khan AH, Rasaily D. Tramadol use in premature ejaculation: daily versus sporadic treatment. Indian J Psychol Med 2013;35:256-9. [Crossref] [PubMed]
- Bar-Or D, Salottolo KM, Orlando A, et al. A randomized double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of two doses of the tramadol orally disintegrating tablet for the treatment of premature ejaculation within less than 2 minutes. Eur Urol 2012;61:736-43. [Crossref] [PubMed]
- Martyn-St James M, Cooper K, Kaltenthaler E, et al. Tramadol for premature ejaculation: a systematic review and meta-analysis. BMC Urol 2015;15:6. [Crossref] [PubMed]
- Alghobary M, El-Bayoumy Y, Mostafa Y, et al. Evaluation of tramadol on demand vs. daily paroxetine as a long-term treatment of lifelong premature ejaculation. J Sex Med 2010;7:2860-7. [Crossref] [PubMed]
- Adams EH, Breiner S, Cicero TJ, et al. A Comparison of the Abuse Liability of Tramadol, NSAIDs, and Hydrocodone in Patients with Chronic Pain. J Pain Symptom Manage 2006;31:465-76. [Crossref] [PubMed]
- Cicero TJ, Adams EH, Geller A, et al. A postmarketing surveillance program to monitor Ultram® (tramadol hydrochloride) abuse in the United States. Drug Alcohol Depend 1999;57:7-22. [Crossref] [PubMed]
- Aversa A, Francomano D, Bruzziches R, et al. Is there a role for phosphodiesterase type-5 inhibitors in the treatment of premature ejaculation. Int J Impot Res 2011;23:17-23. [Crossref] [PubMed]
- McMahon CG, McMahon CN, Liang JL, et al. Efficacy of type-5 phosphodiesterase inhibitors in the drug treatment of premature ejaculation: A systematic review. BJU Int 2006;98:259-72. [Crossref] [PubMed]
- Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: A double-blind, randomized, placebo-controlled study. BJU Int 2004;93:1018-21. [Crossref] [PubMed]
- Carson C, Wyllie M. Improved Ejaculatory Latency, Control and Sexual Satisfaction When PSD502 is Applied Topically in Men with Premature Ejaculation: Results of a Phase III, Double-Blind, Placebo-Controlled Study. J Sex Med 2010;7:3179-89. [Crossref] [PubMed]
- Melnik T, Althof S, Atallah AN, et al. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev 2011. [PubMed]
- Abdo CHN, Afif-Abdo J, Otani F, et al. Sexual satisfaction among patients with erectile dysfunction treated with counseling, sildenafil, or both. J Sex Med 2008;5:1720-6. [Crossref] [PubMed]
- Aubin S, Heiman JR, Berger RE, et al. Comparing sildenafil alone vs. sildenafil plus brief couple sex therapy on erectile dysfunction and couples’ sexual and marital quality of life: A pilot study. J Sex Marital Ther 2009;35:122-43. [Crossref] [PubMed]
- Steggall MJ, Fowler CG, Pryce A. Combination therapy for premature ejaculation: Results of a small-scale study. Sex Relatsh Ther 2008;23:365-76. [Crossref]
- Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol 2016;5:549-62. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. Retarded ejaculation in men: An overview of psychological and neurobiological insights. World J Urol 2005;23:76-81. [Crossref] [PubMed]
- Waldinger MD. Delayed and premature ejaculation. Clinical manual of sexual disorders 2009;273-304. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2009-12921-010&site=ehost-live&scope=site
- Jenkins LC, Mulhall JP. Delayed orgasm and anorgasmia. Fertil Steril 2015;104:1082-8. [Crossref] [PubMed]
- McMahon CG, Jannini E, Waldinger M, et al. Standard Operating Procedures in the Disorders of Orgasm and Ejaculation. J Sex Med 2013;10:204-29. [Crossref] [PubMed]
- McMahon CG. Management of ejaculatory dysfunction. Intern Med J 2014;44:124-31. [Crossref] [PubMed]
- Di Sante S, Mollaioli D, Gravina GL, et al. Epidemiology of delayed ejaculation. Transl Androl Urol 2016;5:541-8. [Crossref] [PubMed]
- Rowland D, McMahon CG, Abdo C, et al. Disorders of orgasm and ejaculation in men. J Sex Med 2010;7:1668-86. [Crossref] [PubMed]
- Harley EW-Y, Boardman J, Craig T. Sexual problems in schizophrenia: prevalence and characteristics. A cross sectional survey. Soc Psychiatry Psychiatr Epidemiol 2010;45:759-66. [Crossref] [PubMed]
- Vallejo-Medina P, Sierra JC. Adaptation, equivalence, and validation of the changes in sexual functioning questionnaire-drugs in a sample of drug-dependent men. J Sex Marital Ther 2013;39:368-84. [Crossref] [PubMed]
- Corona G, Jannini EA, Vignozzi L, et al. The hormonal control of ejaculation. Nat Rev Urol 2012;9:508-19. [Crossref] [PubMed]
- Khera M, Bhattacharya RK, Blick G, et al. Improved sexual function with testosterone replacement therapy in hypogonadal men: Real-world data from the Testim Registry in the United States (TRiUS). J Sex Med 2011;8:3204-13. [Crossref] [PubMed]
- Corona G, Jannini EA, Mannucci E, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med 2008;5:1991-8. [Crossref] [PubMed]
- Tamam Y, Tamam L, Akil E, et al. Post-stroke sexual functioning in first stroke patients. Eur J Neurol 2008;15:660-6. [Crossref] [PubMed]
- Sadowski DJ, Butcher MJ, Köhler TS. A Review of Pathophysiology and Management Options for Delayed Ejaculation. Sex Med Rev 2016;4:167-76. [Crossref] [PubMed]
- Hatzimouratidis K, Amar E, Eardley I, et al. Guidelines on Male Sexual Dysfunction: Erectile Dysfunction and Premature Ejaculation. Eur Urol 2010;57:804-14. [Crossref] [PubMed]
- Corona G, Mannucci E, Petrone L, et al. Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J Androl 2006;27:453-8. [Crossref] [PubMed]
- Modell JG, May RS, Katholi CR. Effect of bupropion-sr on orgasmic dysfunction in nondepressed subjects: A pilot study. J Sex Marital Ther 2000;26:231-40. [Crossref] [PubMed]
- Althof SE. Sexual therapy in the age of pharmacotherapy. Annu Rev Sex Res 2006;17:116-31.
- Abdel-Hamid IA, Elsaied M, Mostafa T. The drug treatment of delayed ejaculation. Transl Androl Urol 2016;5:576-91. [Crossref] [PubMed]
- Hollander AB, Pastuszak AW, Hsieh TC, et al. Cabergoline in the Treatment of Male Orgasmic Disorder-A Retrospective Pilot Analysis. Sex Med 2016;4:e28-33. [Crossref] [PubMed]
- Keller Ashton A, Hamer R, Rosen RC. Serotonin reuptake inhibitor-induced sexual dysfunction and its treatment: A large-scale retrospective study of 596 psychiatric outpatients. J Sex Marital Ther 1997;23:165-75. [Crossref] [PubMed]
- IsHak WW. Berman DS, Peters A. Male anorgasmia treated with oxytocin. J Sex Med 2008;5:1022-4. [Crossref] [PubMed]
- de Jong TR, Veening JG, Olivier B, et al. Oxytocin involvement in SSRI-induced delayed ejaculation: A review of animal studies. J Sex Med 2007;4:14-28. [Crossref] [PubMed]
- McCormick S, Olin J, Brotman AW. Reversal of fluoxetine-induced anorgasmia by cyproheptadine in two patients. J Clin Psychiatry 1990;51:383-4. [PubMed]
- Aizenberg D, Zemishlany Z, Weizman A. Cyproheptadine treatment of sexual dysfunction induced by serotonin reuptake inhibitors. Clin Neuropharmacol 1995;18:320-4. [Crossref] [PubMed]
- Bitran D, Hull EM, Holmes GM, et al. Regulation of male rat copulatory behavior by preoptic incertohypothalamic dopamine neurons. Brain Res Bull 1988;20:323-31. [Crossref] [PubMed]
- Paduch DA, Polzer PK, Ni X, et al. Testosterone replacement in androgen-deficient men with ejaculatory dysfunction: A randomized controlled trial. J Clin Endocrinol Metab 2015;100:2956-62. [Crossref] [PubMed]
- Comarr AE. Sexual Function Among Patients with Spinal Cord Injury. Urol Int 1970;25:134-68. [Crossref] [PubMed]
- Tsuji I, Nakajima F, Morimoto J, et al. The sexual function in patients with spinal cord injury. Urol Int 1961;12:270-80. [Crossref] [PubMed]
- Bors E, Comarr AE. Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960;10:191-222.
- McDonald JW, Sadowsky C. Spinal-cord injury. Lancet 2002;359:417-25. [Crossref] [PubMed]
- Tomasi PA, Fanciulli G, Delitala G. Successful treatment of retrograde ejaculation with the α1-adrenergic agonist methoxamine: Case study. Int J Impot Res 2005;17:297-9. [Crossref] [PubMed]
- Jefferys A, Siassakos D, Wardle P. The management of retrograde ejaculation: A systematic review and update. Fertil Steril 2012;97:306-12. [Crossref] [PubMed]
- Muneer A, Hirsh A. Retrograde Ejaculation and Anejaculation. In: Sharif K, Coomarasamy A. editor. Assisted Reproduction Techniques: Challenges and Management Options. Hoboken: Wiley-Blackwell, 2012:360-3.
- Barazani Y, Stahl PJ, Nagler HM, et al. Management of ejaculatory disorders in infertile men. Asian J Androl 2012;14:525-9. [Crossref] [PubMed]
- Blanker MH, Bosch JL, Groeneveld FP, et al. Erectile and ejaculatory dysfunction in a community-based sample of men 50 to 78 years old: Prevalence, concern, and relation to sexual activity. Urology 2001;57:763-8. [Crossref] [PubMed]
- Nickel JC, Elhilali M, Vallancien G. Benign prostatic hyperplasia (BPH) and prostatitis: Prevalence of painful ejaculation in men with clinical BPH. BJU Int 2005;95:571-4. [Crossref] [PubMed]
- Barnas JL, Pierpaoli S, Ladd P, et al. The prevalence and nature of orgasmic dysfunction after radical prostatectomy. BJU Int 2004;94:603-5. [Crossref] [PubMed]
- Barnas J, Parker M, Guhring P, et al. The utility of tamsulosin in the management of orgasm-associated pain: A pilot analysis. Eur Urol 2005;47:361-5. [Crossref] [PubMed]
- Ilie CP, Mischianu DL, Pemberton RJ. Painful ejaculation. BJU Int 2007;99:1335-9. [Crossref] [PubMed]
- Mogorovich A, Nilsson AE, Tyritzis SI, et al. Radical prostatectomy, sparing of the seminal vesicles, and painful orgasm. J Sex Med 2013;10:1417-23. [Crossref] [PubMed]
- Parnham A, Serefoglu EC. Retrograde ejaculation, painful ejaculation and hematospermia. Transl Androl Urol 2016;5:592-601. [Crossref] [PubMed]
- Yeates W. Ejaculatory Disturbances. In: Pryor J, Lipschultz L. editors. Andrology. London: Butterworth, 1987:183.
- McMahon C. Disorders of Male Orgasm and Ejaculation. In: Wein AJ, Kavoussi LR, Partin AW, et al. editors. Campbell-Walsh Urology. Philadelphia: Elsevier, 2016:692-708.
- Fedder J, Kaspersen MD, Brandslund I, et al. Retrograde ejaculation and sexual dysfunction in men with diabetes mellitus: a prospective, controlled study. Andrology 2013;1:602-6. [Crossref] [PubMed]
- Paduch DA, Polzer P, Morgentaler A, et al. Clinical and Demographic Correlates of Ejaculatory Dysfunctions Other Than Premature Ejaculation: A Prospective, Observational Study. J Sex Med 2015;12:2276-86. [Crossref] [PubMed]
- Shoshany O, Abhyankar N, Elyaguov J, et al. Efficacy of treatment with pseudoephedrine in men with retrograde ejaculation. Andrology 2017;5:744-8. [Crossref] [PubMed]
- Ochsenkühn R, Kamischke A, Nieschlag E. Imipramine for successful treatment of retrograde ejaculation caused by retroperitoneal surgery. Int J Androl 1999;22:173-7. [Crossref] [PubMed]
- Reynolds JC, McCall A, Kim ED, et al. Bladder neck collagen injection restores antegrade ejaculation after bladder neck surgery. J Urol 1998;159:1303. [Crossref] [PubMed]
- Nagai A, Nasu Y, Watanabe M, et al. Analysis of retrograde ejaculation using color Doppler ultrasonography before and after transurethral collagen injection. Int J Impot Res 2004;16:456-8. [Crossref] [PubMed]
- Kurbatov D, Russo GI, Galstyan GR, et al. Correction of Retrograde Ejaculation in Patients with Diabetes Mellitus Using Endourethral Collagen Injection: Preliminary Results. J Sex Med 2015;12:2126-9. [Crossref] [PubMed]
- Roberts M, Jarvi K. Steps in the investigation and management of low semen volume in the infertile man. Can Urol Assoc J 2009;3:479-85. [Crossref] [PubMed]
- Miner M, Rosenberg MT, Perelman MA. Treatment of lower urinary tract symptoms in benign prostatic hyperplasia and its impact on sexual function. Clin Ther 2006;28:13-25. [Crossref] [PubMed]
- Tash JA, McGovern JH, Schlegel PN. Acquired hypogonadotropic hypogonadism presenting as decreased seminal volume. Urology 2000;56:669xvii-xix.
- Wilschanski M, Corey M, Durie P, et al. Diversity of reproductive tract abnormalities in men with cystic fibrosis. JAMA 1996;276:607-8. [Crossref] [PubMed]
- Santucci RA, Joyce GF, Wise M. Male Urethral Stricture Disease. J Urol 2007;177:1667-74. [Crossref] [PubMed]
- Ozgök Y, Tan Ö, Kilciler M, et al. Diagnosis and treatment of ejaculatory duct obstruction in male infertility. Eur Urol 2001;39:24-9. [Crossref] [PubMed]
- Sigman M, Boyle K, Jarow JP. Prevalence of Sperm in the Post-Ejaculatory Urine of Fertile and Subfertile Men. Urology 2008;71:110-2. [Crossref] [PubMed]
- Engin G, Kadioǧlu A, Orhan I, et al. Transrectal US and endorectal MR imaging in partial and complete obstruction of the seminal duct system: A comparative study. Acta radiol 2000;41:288-95. [Crossref] [PubMed]
- Engin G, Celtik M, Sanli O, et al. Comparison of transrectal ultrasonography and transrectal ultrasonography-guided seminal vesicle aspiration in the diagnosis of the ejaculatory duct obstruction. Fertil Steril 2009;92:964-70. [Crossref] [PubMed]
- Purohit RS, Wu DS, Shinohara K, et al. A prospective comparison of 3 diagnostic methods to evaluate ejaculatory duct obstruction. J Urol 2004;171:232-5. [Crossref] [PubMed]
- Kanto S, Uto H, Toya M, et al. Fresh testicular sperm retrieved from men with spinal cord injury retains equal fecundity to that from men with obstructive azoospermia via intracytoplasmic sperm injection. Fertil Steril 2009;92:1333-6. [Crossref] [PubMed]
- Fisch H, Kang YM, Johnson CW, et al. Ejaculatory duct onstruction. Curr Opin Urol 2002;12:509-15. [Crossref] [PubMed]
- Mathers MJ, Degener S, Sperling H, et al. Hematospermia-a Symptom With Many Possible Causes. Dtsch Arztebl Int 2017;114:186-91. [PubMed]
- Stefanovic KB, Gregg PC, Soung M. Evaluation and treatment of hematospermia. Am Fam Physician 2009;80:1421-7. [PubMed]
- Leocádio DE, Stein BS. Hematospermia: etiological and management considerations. Int Urol Nephrol 2009;41:77-83. [Crossref] [PubMed]
- Raviv G, Laufer M, Miki H. Hematospermia-the added value of transrectal ultrasound to clinical evaluation: Is transrectal ultrasound necessary for evaluation of hematospermia? Clin Imaging 2013;37:913-6. [Crossref] [PubMed]
- Suzuki K, Nishimi D, Morioka H, et al. Hematospermia associated with congenital arteriovenous malformation of internal iliac vessels. Int J Urol 2007;14:370-2. [Crossref] [PubMed]
- Han M, Brannigan RE, Antenor JA, et al. Association of hemospermia with prostate cancer. J Urol 2004;172:2189-92. [Crossref] [PubMed]
- Raaijmakers R, Kirkels WJ, Roobol MJ, et al. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology 2002;60:826-30. [Crossref] [PubMed]
- Wilson C, Boyd K, Mohammed A, et al. A single episode of haematospermia can be safely managed in the community. Int J Clin Pract 2010;64:1436-9. [Crossref] [PubMed]


