Training in reconstructive urology: the past, present and future
Introduction
To define “training” in any discipline requires a clear definition of the discipline itself. Reconstructive urology remains one of the hardest urologic sub-specialties to define with branches extending into other sub-specialties including uro-oncology, andrology, prosthetics, incontinence/voiding dysfunction, pediatrics, robotics and even plastic surgery. The only definition easily found is from Wikipedia: “reconstructive urology is a highly specialized field of male urology that restores both structure and function to the genitourinary tract”. Despite this loose definition much of reconstructive urology has focused on urethral stricture (US) surgery. Besides urethral disease, there are some fields that also fall under the genitourinary reconstructive (GR) umbrella including surgery for erectile dysfunction, Peyronie’s disease, genital plastic surgery, male incontinence, cancer survivorship, female urology, neurogenic bladder, urinary diversion, transitional urology, urological trauma and urinary fistulae. Nonetheless, there is a tacit agreement on that US surgery is the tie which binds every GR surgeon, so that will be our starting point.
There is evidence from ancient Egypt, India (1) and the Roman Empire (2,3), describing many ingenious procedures to treat US. Some of them have remained surprisingly unchanged for centuries in spite of medical progress. In the late 18th century, the first internal urethrotome was created, so this became the main and only surgical procedure utilized to treat urethral obstructions over the following 100 years (3). Despite the fact that many novel techniques were developed throughout the 20th century (4-6), they were mastered by a handful of surgeons only. Urethroplasty was only intermittently performed during this timeframe but there was a paucity of underlying scientific principles and tissue transfer, so failure rates were often unacceptably high (7). As a consequence, the vast majority of urologists have remained doing the simple direct vision internal urethrotomy (DVIU) (8,9), in spite of its very high recurrence rate and lack of cost-effectiveness (10,11).
On the other hand, life expectancy, access to surgical procedures along with cancer survivorship rates have been rising dramatically during the 20th and 21th centuries, leading to an accumulation of economically and socially active patients with either inflammatory, iatrogenic or age-related urinary sequelae, which need to be treated.
Over the last 30 years, urethral reconstruction, prosthetics, female urology and neurourology have shown enormous progress, with much wider range of available treatments focused on patients’ quality of life (12,13). Since quality of life is a rather new concept for physicians and patients, the field of reconstructive urology continues to grow (10,14). The present article intends to be a review of the history, current status and future perspectives of GR education.
The past of male genitourinary reconstruction
The first formal fellowship training program was created in 1975 at Eastern Virginia Medical School by Dr. Charles Devine, in the form of the Adult and Pediatric Genitourinary Reconstructive Surgery Fellowship. In 1983, the Society of Genitourinary Reconstructive Surgeons (GURS) was also founded by Dr. Devine, so since its creation it has supported researching, academic activities, along with formal training in the GR field. Afterwards, the Male Genitourinary Reconstruction and Trauma Fellowship at University of California, San Francisco, was created by Dr. Jack McAninch in 1989. Shortly thereafter a fellowship in Reconstructive Urology was founded at Duke University by Dr. George Webster. For many years these three programs were the pillars of male reconstructive urology training at least in North America. Each fellowship was unique in its training experience. Additionally, equally diverse and distinguished fellowships existed in Europe throughout this timeframe. In the late early 2000s as our understanding of genitourethral diseases, anatomy, tissue transfer, and surgical techniques evolved, reconstructive urology blossomed while “standing on the shoulders of these giants”.
The present
Why formal GR training is necessary?
US is a common urological condition. In fact, the number of procedures related to stricture doubles the amount of ureteroscopies performed (14). In addition to stricture being relatively common, there also appears to be a lack of global GR surgeons relative to the population of patients with these conditions (14,15). As a result many reconstructive urologists worldwide often incur large waitlists (16).
Paradoxically, while the sub-specialty of reconstructive urology blossomed in response to this need, urologists in general became less involved in reconstructive procedures possibly due to a deficit in residency or fellowship training. In 2010, the Reconstruction Steering Committee of the American Urological Association (AUA) created a white paper entitled “Genitourinary Reconstructive Medicine: Where do we stand and what should the future look like?”. They found that among 2010 USA recertifying urologists, reconstructive procedures represented only 1.8% of the total reported by this group (17). Contrastingly, reconstructive procedures comprised 49% of the procedures performed by loosely defined “experts” in this field. Additionally, Liu et al. (10), found that the overall urethral dilation/DVIU to urethroplasty ratio was 25:1 a startling ratio which was discrepant from most recommendations (18). However, rather than a deficiency in training, these statistics may simply represent a lag in training as new certifying urologists perform urethroplasty 3.7 times more frequently when compared to recertifying urologists (10). There is also an enormous geographical variation between urethral dilation/DVIU to urethroplasty ratio in the USA, between 25.7:1 (Nevada) to as low as 2.6:1 (Wyoming). Interestingly, states with a GURS fellowship had a considerably better ratio, equal or less than 10.5:1 (10). Even more, 43.1% of all urethroplasties in the USA were logged by one of the states with a GURS fellowship (10). This centralization may be justified as there has been several publications reporting prolonged learning curves for urethroplasty success. Fossati et al. (19) described a 2% success improvement per 20 procedures. In a multi-institutional database analysis by Faris et al. (20) it was found that the number needed to achieve >90% success rate was about 100 procedures. From either perspective more robust training in reconstructive urology was and still is sorely needed.
Current GR fellowships
In the 2000s the number of GR fellowship programs grew dramatically. In 2014, the GURS began developing a formal reconstructive match, which initially offered 13 different programs. For the 2015–2019 match, 17 fellowship positions were offered while for the 2019–2020 academic year, five new programs were approved (while one withdrew). Most positions (86%; 18/21) are located in the USA, with one in Canada, one in India and one of the new programs is located in Buenos Aires, Argentina, becoming the first South American fellowship in the GURS match. By email communication, we also found other non-GURS reconstructive urology fellowships in Australia, Brazil, Chile, Dominican Republic, United Kingdom, Germany, and Italy.
Through the GURS match, “reconstructive urology” is broadly defined as one of six main categories including:
- Male urethral reconstruction;
- Male incontinence surgery;
- Male sexual health;
- Genital reconstruction (including gender confirming surgery);
- Urinary diversion/ureteral reconstruction;
- Female urethral reconstruction (including female continence surgery, prolapse repair, urethral diverticulum, nerve stimulation).
To qualify for GURS certification a program must meet minimum requirements in two of these areas, at least one of which is urethroplasty. University sponsorship, program director’s experience, along with academic proficiency are also required and annually reviewed in order to be recognized by GURS (available in http://www.societygurs.org/initiatives/fellowship/fellowship-requirements).
Increasing interest in reconstructive urology
For the 2018–2019 academic year, the GURS match had 44 registered applicants and 34 applicants submitting lists for a total of 16 programs and 17 vacancies listed. Among the aforementioned 34 applicants, 28 (82%) were American or Canadian, while the remaining 18% were international medical graduates. Ultimately 17 applicants matched, 15 (88%) and 2 (12%) were American/Canadian and foreign graduates, respectively. It appears interest continues to grow in GR fellowship training as previous years had between 26–28 total applicants and 17–23 candidates ranking programs.
The typical GURS fellowship experience
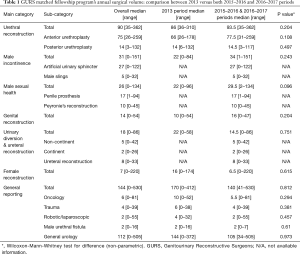
We created a Case Log database, including GURS programs from the 2013–2014, 2015–2016 and 2016–2017 training periods (from GURS Fellowship Committee database). We also included five non-GURS fellowships in the analysis. Not every program had available data for every period, so we grouped them in 2 periods, i.e., 2013–2014 and 2015–2017 (2 training years). All programs were 12 months clinical, but one which was 18 months and other was variable. Four programs offer an optional second research year. Comparison between specific fellowships is out of the scope of this article.
Over a period of 12 months, the median total volume of urethroplasty was 90, 31 male incontinence procedures, 26 male sexual surgeries, 14 genital reconstruction, 18 urinary diversion/upper tract and 7 female reconstructive procedures (Table 1).
Full table
Interestingly, the only surgery performed by every single fellow was urethroplasty (Table 1), however, there were considerable differences in between programs (Kruskall-Wallis test, P=0.0027).
There was an enormous variability among the remaining reconstructive fields, reflecting important disparities in the skills acquired by graduates. For example, in a same training period there were GURS graduates who did not perform any female procedures, while others did 220.
When comparing both 2013–2014 and 2015–2017 periods, we found some differences, nevertheless, none of them were statistically relevant (Table 1).
Strikingly, the only significant differences between a GURS and a non-GURS fellowship were observed in both penile prosthesis, with 17 vs. 6 (P=0.01), and genital reconstruction, with 14 vs. 4 (P=0.006) procedures, respectively. Moreover, non-GURS programs showed a urethroplasty volume of 96, which is slightly higher than the GURS’s 90 (P=0.71).
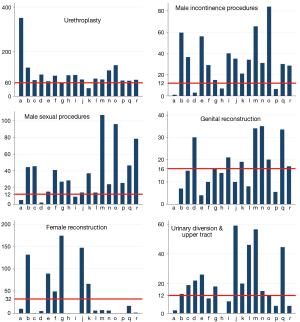
The GURS Society has established thresholds for each sub-category. We pooled data from 18 programs and 19 positions of all periods above mentioned (excluding non-GURS fellowships) and we calculated their medians. The vast majority of programs reached the urethroplasty criteria (60 cases). For other procedures, 56% did not accomplish the necessary genital reconstruction volume, while 44% in female reconstruction along with 33% in urinary diversion-upper tract surgery did not either. Regarding male incontinence and male sexual health procedures, 78% and 83% of all programs complied with the volume required (Figure 1).
Fellowship training outcomes: results of a GURS graduate survey
A recent survey of GURS fellowship graduates from 2014 to 2016 (21) has shed some light on the current status of GURS fellowship training. In general, fellows are pleased with their fellowship experience as 92% of respondents would have repeated their GURS fellowship. Additionally most were satisfied with their operative volumes and felt ready to enter reconstructive practice. In particular, 92% of fellows were satisfied with the volume of urethroplasties offered during fellowship, while 83% were satisfied with the volume of male incontinence surgery. Moreover, 79% and 92% were pleased with their male sexual health and genital reconstruction surgical volume. Satisfaction rates were slightly lower regarding ureteral reconstruction and urinary diversion (71%) while female pelvic reconstruction experience continues to be variable as only 21% felt they experienced a sufficient volume of female reconstruction during fellowship. Overall, 100% of graduates “felt competent to enter unsupervised reconstructive urology practice after fellowship” with 96%, 92%, 92%, 88%, and 33% of fellows reporting that they felt competent in urethral reconstruction, male incontinence, urinary diversion/ureteral reconstruction, male sexual health, and female reconstruction, respectively, upon graduation. On balance, fellowship training appears to prepare most graduates for practice. However, 36% of respondents would favor an additional training track other than urethroplasty suggesting either a robotic/abdominal reconstruction and/or a urologic prosthetic track.
GURS graduates readily find employment as 100% secured a job within 6 months of completed fellowship and 88% secured a job prior to fellowship completion. Additionally, 92% of GURS graduates practice in a location that they consider one of their top 3 destinations and 92% were satisfied with their practice as a reconstructive urologist.
In general, certified GURS fellowship training appears to meet fellow expectations while providing highly competent, satisfied and gainfully employed GR surgeons. Is this good enough and what does the future hold?
The future of GR training
While GR training has come a long way and generally speaking creates competent reconstructive surgeons, there remains a lot of challenges to address. Moreover, fellowship training at individual centers also has some inherent variability. A few possible ways to improve current training might be:
- Create a formal GURS approved curriculum with periodic updating, which could help bridge gaps in GR knowledge worldwide and between fellowship programs.
- To modify current Fellowship Case Logs in order to obtain more comprehensive data about fellow training experiences. For instance, transitional urology is a growing field which has no specific representation in the current Case Log. Female Urology is more diverse than slings, with female urethroplasty, sacral nerve stimulation, artificial urinary sphincter, mesh erosion, bulking agents and vesicovaginal fistulae widely underreported.
- Volume thresholds may need to be reviewed. In some cases the male urethroplasty threshold could be reduced at the expense of increase in other fields, allowing incorporation of new technologies such as robotics and other conditions such as gender confirming surgery.
- There is likely an emerging need to make training more flexible to incorporate more this diversity in training. Rather than programs potentially withdrawing because of the inability to satisfy urethroplasty threshold, we believe that GURS should take advantage of this diversity. Potentially offering program certification according to different sub-categories might be beneficial. This eventually would allow having, for example, a “graduate GURS fellow trained in urethroplasty, prosthetics and female urology”.
- Another option may be to evaluate expanding reconstructive urology training to 2 years, allowing for a broader surgical exposure.
- To establish formal exchange programs between centers also could help more rapidly disseminate technical advances. Additionally, given that most reconstructive fellowships are in North America and the biggest need exists outside of this region, further worldwide outreach and collaborative creation of new fellowship programs in these regions of need would be very helpful.
- To favour scientific publications in regard to GR epidemiological topics, so that regions requiring a GURS led needs assessment of reconstructive urology.
- Live surgery courses at noted centers of excellence such as those in London, Hamburg and Santiago will continue to be an area of needed growth.
- To innovate in new educational resources for residents and general urologists to be updated in GR basics: webinars, online courses, social networking (chats, surgeries by streaming).
- To introduce new technologies such as surgical simulation can help to augment exposure of less common but important areas such as trauma surgery.
- As reconstructive training evolves there will also be a need for further communication and collaboration with other sub-specialty organizations whom overlap in our training. One sub-specialty cannot exist in a silo, sharing key ideas will benefit us, our trainees and our patients.
- Lastly, we cannot forget our residents, there is clearly a need to educate all urologists in reconstructive principles by ensuring all residency training programs offer formal and informal training in GR urology.
Acknowledgements
The authors would like to thank Daniela Andrich, Jessica DeLong, Andrew Fuller, Carlos Giudice, Reynaldo Gómez, Jodi Hirst, Wellington Ledezma, Ramón Virasoro.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Das S. Urology in ancient India. Indian J Urol 2007;23:2-5. [Crossref] [PubMed]
- Attwater HL. The history of urethral stricture. Brit J Urol 1943;15:39. [Crossref]
- Blandy JP. Urethral stricture. Postgrad Med J 1980;56:383-418. [Crossref] [PubMed]
- Sapezhko KM. To the treatment of urethral defects using mucosa grafts Chirurgicheskaya Letopis 1894;4:775-84. (in Russian).
- Korneyev I, Ilyin D, Schultheiss D, et al. The first oral mucosal graft urethroplasty was carried out in the 19th century: the pioneering experience of Kirill Sapezhko (1857-1928). Eur Urol 2012;62:624-7. [Crossref] [PubMed]
- Barbagli G, Balò S, Montorsi F, et al. History and evolution of the use of oral mucosa for urethral reconstruction. Asian J Urol 2017;4:96-101. [Crossref] [PubMed]
- Bandhauer K. Chapter 2: Historical Highlights in the Development of Urethral Surgery. In: Schreiter F, Jordan GH. editors. Reconstructive Urethral Surgery. Heidelberg: Springer, 2006:5-10.
- Bullock TL, Brandes SB. Adult anterior urethral strictures: a national practice patterns survey ofboard certified urologists in the United States. J Urol 2007;177:685-90. [Crossref] [PubMed]
- Anger JT, Buckley JC, Santucci RA, et al. Trends in stricture management among male Medicarebeneficiaries: underuse of urethroplasty? Urology 2011;77:481-5. [Crossref] [PubMed]
- Liu JS, Hofer MD, Oberlin DT, et al. Practice Patterns in the Treatment of Urethral Stricture Among American Urologists: A Paradigm Change? Urology 2015;86:830-4. [Crossref] [PubMed]
- Rourke KF, Jordan GH. Primary urethral reconstruction: the cost minimized approach to the bulbous urethral stricture. J Urol 2005;173:1206-10. [Crossref] [PubMed]
- Le B, Burnett AL. Evolution of penile prosthetic devices. Korean J Urol 2015;56:179-86. [Crossref] [PubMed]
- Costantini E, Lazzeri M. Lean Mean Research: The 21st Century Challenge for Urology. European Urology 2010;57:980-2. [Crossref] [PubMed]
- Santucci RA. The reconstructive urology work force: present and future. Transl Androl Urol 2014;3:205-8. [PubMed]
- Neuwahl S, Thompson K, Fraher E, et al. HPRI data tracks. Urology workforce trends. Bull Am Coll Surg 2012;97:46-9. [PubMed]
- Hoy NY, Chapman DW, Dean N, et al. Incidence and Predictors of Complications Due to Urethral Stricture in Patients Awaiting Urethroplasty. J Urol 2017. [Epub ahead of print]. [PubMed]
- Flanigan RC, Badlani G, Howards S, et al. White Paper on Genitourinary Reconstructive Medicine: Where do we stand and what should the Future look like? Available online: https://www.google.ca/url?sa=t&rct=j&q=&esrc=s&source=web&cd=9&cad=rja&uact=8&ved=0ahUKEwjE_-mjsunXAhUHrlQKHbpdBqwQFghwMAg&url=https%3A%2F%2Fwww.auanet.org%2FDocuments%2Feducation%2Fclinical-guidance%2FGenitourinary-Reconstruction-WP.pdf&usg=AOvVaw2y5TuE14032ifyFneh0rqF
- Wessells H, Angermeier KW, Elliott S, et al. Male Urethral Stricture: American Urological Association Guideline. J Urol 2017;197:182-90. [Crossref] [PubMed]
- Fossati N, Barbagli G, Larcher A, et al. The Surgical Learning Curve for One-stage Anterior Urethroplasty:A Prospective Single-surgeon Study. Eur Urol 2016;69:686-90. [Crossref] [PubMed]
- Faris SF, Myers JB, Voelzke BB, et al. Assessment of the Male Urethral Reconstruction Learning Curve. Urology 2016;89:137-42. [Crossref] [PubMed]
- Buckley J, Rourke K, McCammon K. Training the Next Generation of Genitourinary Reconstructive Surgeons Feedback and Future Directions. In Press.


