Moderate hypofractionation for prostate cancer
Introduction
External beam radiation therapy (EBRT) has been commonly used in the definitive treatment of prostate cancer for the last four decades. In men with localized prostate cancer EBRT results in similar long-term cancer control as those achieved with radical prostatectomy (1). In the last two decades technological advances in the planning and delivery of prostate EBRT have allowed for more precise and conformal treatment. Dose-escalation using conventional fractionation (CF) with daily fractions of 1.8–2 Gy has reduced biochemical recurrence (BCR) at the expense of increased overall treatment time, extending to nine or more weeks (2-4).
In 1999 Brenner and Hall published an analysis that suggested that the fractionation sensitivity of prostate cancer, relative to the nearby normal tissues, would favor the use of fewer, larger daily fractions (hypofractionation; HF). According to these scientists, HF would be expected to result in similar levels of tumor control with logistic and financial advantages compared with CF (5). Following the publication of this paper, a number of retrospective analyses reinforced the underlying hypothesis that the fractionation sensitivity of prostate cancer might favor HF schedules (6). As a result, several groups designed and opened prospective clinical trials examining moderate HF (dose per fraction 2.4–3.5 Gy). This brief review will focus on the randomized trials that compare CF to moderate HF in the treatment of prostate cancer.
Older randomized trials
Prior to the publication of the Brenner paper, two randomized trials comparing fractionation schemes had already been designed and were actively accruing patients. Each of these studies was a pragmatic attempt to distinguish between two commonly used regimens in regions with national health care; neither made any explicit assumptions on the fractionation sensitivity of prostate cancer.
Cancer Care Ontario
In the mid 1990’s investigators in Canada designed a study that compared two radiation schedules in common usage; 66 Gy in 33 fractions over 6.5 weeks (CF) and 52.5 Gy in 20 fractions over 4 weeks (HF) (7). No androgen deprivation was allowed. The primary endpoint was a composite of biochemical or clinical failure (BCF) and the trial was designed with a non-inferiority (NI) margin of 7.5%. Eligible patients had T1–2 prostate cancer with a prostate-specific antigen (PSA) <40; there were no Gleason score requirements. CT planning was mandatory for all patients.
Between March 1995 and December 1998, 938 men were enrolled and the first publication was reported with a median follow-up of 5.7 years. The mean age was 70 (range, 53–84) years and the mean PSA was 10 ng/mL. Treatment groups were well balanced with regard to baseline characteristics and risk group stratification; approximately 40% of men in each arm had Gleason score of ≥7.
The 5-year estimate of BCF in the CF and HF arms were 53% and 60%, respectively. The absolute difference was 7% (90% CI, 1.4–12.6%) and the authors could not exclude the possibility that HF was inferior. The overall hazard ratio was 1.18 (95% CI, 0.99–1.41) in favor of CF. Overall survival at 5 years was estimated to 85% and 88% in the CF and HF arms, respectively.
Acute radiation toxicity was experienced by 11% of men in the short arm compared to 7% of men on the long arm. Late toxicity was reported by 3% of patients on each treatment arm. The majority of toxicity was genitourinary (GU).
Adelaide
A second trial was accomplished in Adelaide, Australia and enrolled men with T1–2 prostate cancer from 1996–2003 (8). The trial compared two fractionation regimens in common in Australia at the time; 55 Gy in 20 fractions (HF) and 64 Gy in 32 fractions (CF). The primary endpoint was late morbidity with a minimum follow-up of two years. The authors used unvalidated modifications of the LENT-SOMA gastrointestinal (GI) and GU toxicity scales. The sample size was calculated to be able to detect an absolute difference of 20% in late morbidity as reported by the physician using these scales.
In total, 217 men with a median age of 69 years (range, 44–82 years) were enrolled and analyzed. The majority of men (156/217, 72%) were treated with two-dimensional methods as three-dimensional capability was not available in Adelaide until 2001. No risk group stratification was used and androgen deprivation therapy was not allowed. The mean PSA for all patients was 13 ng/mL and no information on Gleason grade was provided. At the time of the final analysis the study population had been followed for a median of 90 months (range, 3–138 months). Of the 217 men, 101 (47%) had been lost to follow-up and 65 (30%) had less than five years of follow-up. This lack of follow-up was attributed to advancing age, medical comorbidities and domicile distant from the treatment center.
In the final report GI and GU toxicity persisted 5 years after the completion of treatment but there was no overall difference between the two dose schedules. In multivariable analysis, the authors did report increased GU symptoms at four years with the conventional schedule but the relative risk was modest (RR =1.58; 1.01–2.47) and there was no attempt to control for the multiple comparisons throughout the analysis.
Treatment efficacy was not the primary endpoint but the authors did report freedom from BCR according to treatment regimen. Using the American Society of Radiation Oncology (ASTRO) criteria, the 7.5-year rate of FFBR is 44% for each arm (P= NS). If the Phoenix criteria was used, the FFBR was higher in the hypofractionated arm (53% vs. 34%, P<0.05). No differences were observed in overall survival between the two treatment regimens (71% vs. 69%). Only 6 of the 52 (12%) deaths were related to prostate cancer.
Summary of older randomized trials
The results observed in these two trials are somewhat discordant. The largest trial from Canada found that the shorter more hypofractionated regimen was associated with decreased efficacy whilst the Australia study suggested the opposite if the Phoenix criteria was used (with no effect seen if the ASTRO definition was used). Toxicity did not appear to be markedly different. The doses and techniques used in the older trials are very different than contemporary methods and some may consider the results irrelevant; they are included to provide some historical context.
Contemporary randomized trials: superiority design
In the years following the publication of the Brenner paper, four separate groups of investigators from the United States and Europe designed rigorous randomized trials using a superiority design to compare moderate HF to CF using contemporary methods, doses and techniques. In each study the authors made explicit assumptions about the fractionation sensitivity of prostate cancer and hypothesized that the moderate HF schedule would result in improved efficacy or decreased toxicity. These trials are summarized below.
Regina Elena trial
Investigators in Rome, Italy designed and completed a single-institution, phase III trial comparing 80 Gy in 40 fractions over 8 weeks (CF) to 62 Gy in 20 fractions over 5 weeks (HF) (9). Eligible patients were required to have at least one high-risk feature (Gleason score =8–10, PSA >20 ng/mL) or at least two intermediate-risk features (PSA 10–20, T ≥2c, Gleason score =7). All patients received nine months of neoadjuvant, concurrent and adjuvant combined androgen blockade (LHRH agonist plus antiandrogen). The study hypothesis was that moderate HF would result in a 50% reduction in grade 2 or higher GI toxicity at 3 years with no difference in efficacy.
Between January 2003 and December 2007 168 men were enrolled and the final results were reported in 2017 with a median follow-up of 9 years. In the final intent to treat analysis no differences in late GI or GU toxicity according to fractionation schedule were evident. Similarly, no differences in freedom from BCR, overall survival or cancer-specific survival according to treatment regimen were observed. The authors conclude that moderate HF did not reduce late toxicity.
The authors did report a post-randomization multivariable analysis which found that moderate HF was associated with reduced BCR (HR 0.47; 95% CI, 0.24–0.89). This finding can be explained by the small sample size which increases the likelihood that randomization does not balance out covariate differences. In this case the pretreatment PSA was an important predictor of BCR and there was an imbalance of pretreatment PSA across the randomized arms. This is evidence to argue for increased efficacy of HF but, given the post-hoc nature of the analysis, the evidence is weak.
Fox Chase trial
The Fox Chase trial was also a single-institution, phase III study comparing two schedules: 76 Gy in 38 fractions over 7.6 weeks (CF) and 70.2 Gy in 26 fractions over 5.2 weeks (HF) (10). Eligible patients had intermediate- or high-risk disease. High-risk patients received long-term androgen deprivation. The majority of intermediate risk patients received no androgen deprivation. The study hypothesis was that the HF schedule would result in 50% reduction in biochemical/clinical recurrence at 4 years.
Between June 2002 and May 2006 three hundred and three patients were enrolled and the initial results were reported in 2013 with a median follow-up of 68 months. No significant differences were observed between the arms in disease-related or treatment-related factors. The estimated 5-year rates of biochemical/clinical recurrence were not different; 21% for CF and 23% for HF (P=0.745) using the protocol prescribed modification of the ASTRO definition of BCR. No differences in prostate cancer-specific mortality or overall survival were observed. In multivariable regression higher T stage, Gleason score and initial PSA were associated with increased risk of biochemical/clinical recurrence but fractionation was not significant. As such this trial provides no support for the idea that moderate HF results in increased efficacy.
The authors also reported on early and late GI and GU toxicity, finding no differences when considering all patients. In an unplanned post hoc analysis, patients on the HF arm with pretreatment International Prostate Symptom Scores above 12 (upper quartile; n=34) experienced increased late grade 2+ genitourinary toxicity.
The Fox Chase investigators have recently reported the 5-year quality of life outcomes from this trial. Overall, there were no differences between the two treatment arms. Furthermore, on multivariable analysis there was no association between fractionation regimen and any quality of life parameter.
MD Anderson trial
The MD Anderson trial was another single-institution, phase III trial comparing two fractionation schedules (11). Eligible patients had biopsy-proven adenocarcinoma, clinical stage T1b–3b (1992 AJCC staging system), PSA <20 ng/mL and Gleason score <10. Eligible patients were randomly assigned 1:1 to 75.6 Gy in 42 fractions (CF) or 72 Gy in 30 fractions (HF). The study hypothesis was that the HF arm would result in decreased BCR.
Two hundred and six men were enrolled from 2001 to 2010; the median age was 67 years. According to National Comprehensive Cancer Center Network (NCCN), 28% of men had low-risk disease and 71% had intermediate risk disease. Four months of androgen deprivation was used in 24% of men. Intensity-modulated radiation therapy (IMRT) and daily image guidance were required.
The most recent analysis of the primary endpoint was presented at the Annual Meeting of the ASTRO in 2016; no manuscript has been published to date. With a median follow-up of 8.4 years, fewer recurrences were observed in men on the HF arm. The estimated 10-year risk of BCR was 24% in the CF arm and 11% in the HF arm, respectively (P=0.034). No difference in overall survival was observed.
The authors also reported long term GI and GU toxicity. The 8-year risk of late grade 2 or greater GU toxicity was 16% in the conventional arm and 15% in the HF arm, respectively (P=0.84). The 8-year risk of late grade 2 or greater GI toxicity was 5% in the conventional arm and 13% in the HF arm, respectively (P=0.075). The authors state that men in the HF arm were less likely to meet normal tissue constraints compared to men on the conventional arm which may explain the findings.
HYPRO trial
The largest trial with a superiority hypothesis was designed and completed in the Netherlands (12). This trial included men with intermediate- and high-risk disease and randomly assigned them 1:1 to 78 Gy in 39 fractions over 7.8 weeks (CF) or 64.6 Gy in 19 fractions given three times per week (HF). The primary endpoint was disease-free survival (DFS) and the study hypothesis is that HF would result in an increase from 70% to 80% at three years; an absolute increase of 10%.
Between March 2007 and December 2010, 820 men were enrolled of whom 804 were eligible and analyzable. Two-thirds of men received concomitant androgen suppression for a median of 32 months. The most recent efficacy analysis was published in 2016 with a median follow-up of 60 months. Baseline characteristics were distributed evenly between the groups and IMRT was used in 95% of cases. Daily online image guidance with fiducial markers was used on 94% of patients. The 5-year estimate of relapse-free survival was 77.1% for those allocated to CF and 80.5% for those assigned to HF [P=0.36; adjusted HR (aHR) 0.86; 95% CI, 0.63–1.16]. The overall survival at 5 years was 85.9% and 86.2% for the patients assigned to CF and HF, respectively (P=0.92; HR 1.02; 95% CI, 0.71–1.46). Post-hoc multivariable analysis higher Gleason score, risk of seminal vesicle involvement and androgen deprivation therapy for less than 12 months were all independently associated with a higher risk of relapse.
The late toxicity from the HYPRO was published in a separate report (13). Late toxicity was scored with the Radiation Therapy Oncology Group and European Organisation for Research and Treatment of Cancer (RTOG/EORTC) criteria including physician reporting and patient self-assessment questionnaires. The incidence of grade 2 or greater GU toxicity at 3 years was 39% in the CF group and 41% in the HF group (HR 1.16; 90% CI, 0.98–1.38). The incidence of grade 2 or greater GI toxicity at 3 years was 18% in the CF group and 22% in the HF group (HR 1.19; 90% CI, 0.93–1.52). The study was designed with toxicity as a secondary endpoint with a NI HR margin of 1.11 for GU toxicity and 1.13 for GI toxicity. As such the authors concluded that the data could not confirm that HF was non-inferior for cumulative late GU and GI toxicity.
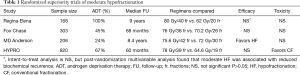
Summary of contemporary trials with superiority hypothesis
The results of these four studies are summarized in Table 1. Despite different eligibility criteria, different fractionation regimens and non-uniform use of androgen deprivation a few general statements can be made. First, there is some evidence to support the idea that moderate HF improves efficacy; but the evidence is weak in that it comes from the two smallest studies and in one case the evidence is based on a post-hoc analysis. Second, the rate of late toxicity appears similar with moderate HF compared to CF provided the dose per fraction stays below 3 Gy. The HYPRO trial did find a modest increase in late toxicity with 64.6 Gy in 19 fractions given three times per week (3.4 Gy/fraction) and this regimen cannot be recommended. Altogether these four trials included <1,500 men; the trials to be considered next included more than 5,000 men.
Full table
Contemporary randomized trials: NI design
All of the trials discussed so far, with one exception, are trials with a superiority design. In other words, the hypothesis tested was that HF would either increase efficacy or reduce toxicity. Trials can also be designed to test a NI hypothesis; e.g., the efficacy of HF is “no worse than” CF. NI trials have been relatively rare in oncology but the numbers of NI trials are increasing. NI trials are typically designed to demonstrate that a new treatment is not worse than a standard treatment, especially when the new treatment has potential advantages of less toxicity, convenience or cost. NI trials are typically much larger than superiority trials because the NI margin that motivates the sample size is generally smaller than superiority studies. Finally, NI trials are notoriously difficult to design and interpret (14). In the next several paragraphs the results of three large NI trials testing moderate HF will be described.
The NRG Oncology trial
The first NI trial to be published is the NRG Oncology trial 0415 (15). Eligible patients were required to have low-risk prostate cancer (T1c–2a, Gleason ≤6 and PSA ≤10 ng/mL). Patients were randomly assigned 1:1 to 73.8 Gy/41 fractions of 1.8 Gy over 8.2 weeks (CF) or 70 Gy/28 fractions of 2.5 Gy over 5.6 weeks (HF). Daily image guidance was required and no androgen suppression was allowed. The primary endpoint was DFS and the pre-specified NI margin was 7.65% at five years (HR <1.52).
Between April 2006 and December 2009, 1,115 participants were enrolled. One thousand and ninety-two men were evaluable. The initial results were published in 2016 with a median follow-up of 5.8 years. The median age was 67 years and the median pretreatment PSA was 5.4 ng/mL. The treatment arms were well balanced with no substantial between-group differences.
The estimated 5-year DFS was 85% in the CF arm and 86.3% in the HF arm. The HR comparing DFS was 0.85 (95% CI, 0.64–1.14) favoring the HF arm and meeting the pre-specified NI criterion (null hypothesis HR >1.52 rejected; P<0.001). The cumulative incidence of BCR at five years was 8% (95% CI, 5.9–10.6%) in the CF arm and 6% (95% CI, 4.5–8.6%) in the HF arm. The HR comparing BCR was 0.77 (95% CI, 0.51–1.17) favoring the HF arm and meeting the pre-specified NI criterion (null hypothesis HR >1.67 rejected; P<0.001). Similarly, the estimated five-year overall survival was 93% (95% CI, 90.7–95.1%) in the CF arm and 92% (95% CI, 89.9–94.5%) in the HF arm (HR 0.95; 95% CI, 0.64–1.41).
No differences in early GI or GU adverse events were observed. Late grade 2 GI toxicity was reported in 11% of patients on the CF arm and 18% of patients on the HF arm (HR 1.59; P<0.005). Late grade 2 GU toxicity was reported in 21% of patients on the CF arm and 26% of patients on the HF arm (HR 1.31; P<0.009). No differences in late grade 3 GI or GU toxicity were observed. One late grade 4 GI/GU toxicity was observed in a patient on the conventional arm. No grade 5 events were observed. Patient reported outcomes from this trial have been presented and no differences were evident but the results have not been published.
The CHHiP trial
The Conventional versus Hypofractionated High-dose intensity-modulated radiotherapy for Prostate cancer (CHHiP) trial is the largest NI trial examining moderate HF (16). Eligible patients had T1–3b prostate cancer, a pretreatment PSA of <30 ng/mL and a risk of seminal vesicle involvement of <30%. The original cohort of 450 men could have a PSA as high as 40 ng/mL and a risk of pelvic lymph node involvement as high as 30%. The trial enrolled more than 3,000 men in the United Kingdom and randomized them 1:1:1 onto three arms. The CF regimen is 74 Gy/37 fractions over 7.4 weeks. There are two experimental HF arms: 60 Gy/20 fractions over 4 weeks and 57 Gy/19 fractions over 3.8 weeks. The vast majority of patients were treated with 3–6 months of androgen suppression before and during radiotherapy. The primary endpoint was time to BCF and the critical hazard ratio for NI was 1.208.
The initial report on efficacy was published in 2016. Between Oct 18, 2002, and June 17, 2011, 3,216 men were enrolled from 71 centers in the United Kingdom. The median follow-up was 62.4 months (IQR, 53.9–77.0). The majority of patients (72%) had intermediate risk disease according to the NCCN risk group, but low-risk (15%) and high-risk (12%) patients were represented as well. The proportion of patients who were BCF-free at 5 years was 88% (95% CI, 86.0–90.2%) in the 74 Gy group, 91% (95% CI, 88.5–92.3%) in the 60 Gy group, and 86% (95% CI, 83.4–88.0%) in the 57 Gy group. As such, the authors concluded that 60 Gy was non-inferior to 74 Gy [HR 0.84 (90% CI, 0.68–1.03), pNI =0.0018] but NI could not be claimed for 57 Gy compared with 74 Gy [HR 1.20 (0.99–1.46), pNI =0.48]. No significant differences in overall survival were observed between the control group and either of the hypofractionated groups.
The report included a toxicity analysis as well. Investigators included three different physician-reported measures and one patient-reported measure. Acute bowel and bladder toxicity was reported more frequently in the hypofractionated arms. There were no observable differences in the long-term side effects according to treatment arm. There were no significant differences in either the proportion or cumulative incidence of side-effects 5 years after treatment according to any of the outcome measures. The 5-year estimated cumulative incidence of Radiation Therapy Oncology Group (RTOG) grade 2 or worse bowel and bladder adverse events was 14% (111 events) and 9% (66 events) in the74 Gy group, 12% (105 events) and 12% (88 events) in the 60 Gy group, and 11% (95 events) and 7% (57 events) in the 57 Gy group, respectively. Patient-reported outcomes from this trial have been published and the results support the finding that toxicity is similar between the two arms (17).
PROstate Fractionated Irradiation Trial (PROFIT)
PROFIT is a multi-national, prospective, randomized trial completed at 27 centers (14 in Canada, 12 in Australia, and 1 in France) (18). Eligible patients were required to have intermediate risk disease (T1 to 2a, Gleason score ≤6, and PSA =10.1 to 20 ng/mL; T2b to 2c, Gleason ≤6, and PSA ≤20 ng/mL; or T1 to 2, Gleason =7, and PSA ≤20 ng/mL). The trial assigned participants 1:1 to 78 Gy/39 fractions over 7.8 weeks (CF) or 60 Gy/20 fractions over 4 weeks (HF). Androgen suppression was not permitted with treatment. The primary outcome was biochemical or clinical failure (BCF) defined by any of the following: PSA failure (nadir + 2 ng/mL), hormonal intervention, clinical local or distant failure, or death as a result of prostate cancer. The pre-specified NI margin was 7.5% (critical hazard ratio of <1.32).
The first analysis of this trial was reported in 2017. Between May 2006 and November 2011, one thousand two hundred and six men were randomly assigned; 598 to the CF arm and 608 to the HF arm. The median follow-up is 6 years. Baseline characteristics were comparable and the median age was 71 years. The five-year estimate of BCF disease-free survival was 85% in both arms. The adjusted HR was 0.96 (90% CI, 0.77–1.20). This met the pre-defined NI criterion.
Acute and late GU and GI toxicities were reported. Acute GU toxicity was similar (4% grade ≥3 in both arms) but there was more acute grade ≥2 GI toxicity in the HF arm (17% vs. 11%). The late grade ≥2 GU toxicity was observed in 22% of men in each arm. Late GI toxicity was reported in 14% of men in the CF arm and 9% in the HF arm; P=0.006. Patient reported outcomes from this trial have been presented and no differences were evident but the results have not been published.
Summary of contemporary NI trials
The results of these three NI trials are summarized in Table 2. The eligibility criteria, use of androgen deprivation and the fractionation schedules compared are different for each trial but some overarching conclusions can be made. First, moderately hypofractionated regimens (4–5 weeks with dose per fraction of 2.5–3 Gy) are non-inferior to conventional regimens lasting 8–9 weeks. Second, at least with regimens using 3 Gy/fractions more acute toxicity is observed. Third, moderate HF has similar risks of late GI and GU toxicity compared to CF. Finally, the patient-reported outcomes are similar between moderate HF and CF.

Full table
Future randomized trials of moderate HF
Following the results of the randomized trials of moderate HF at least two groups have developed trials comparing moderate HF to extreme HF using moderate HF as the standard arm. These trials are summarized in the paragraphs below.
Investigators at the University of Miami have designed and opened a multinational randomized trial (NCT01794403) known as the Hypofractionation via Extended versus Accelerated Therapy (HEAT) study. Eligible patients have low- or intermediate-risk disease and are required to have a prostate volume of ≤80 cc and an International Prostate Symptom Score (IPSS) of ≤12. Once accrued, patients are randomly assigned 1:1 to 70.2 Gy in 26 fractions over 5.2 weeks or 36.25 Gy in 5 fractions over two weeks. The primary endpoint is BCF (including positive biopsy) and the hypothesis tested is that the extreme HF is non-inferior to the moderate HF arm (NI margin is 12%). The sample size is 456 patients. The trial was opened in April 2013 and the estimated date of study completion is March 2023.
NRG Oncology GU-005 is a prospective randomized trial comparing the moderate HF arm of NRG 0415 (70 Gy in 28 fractions over 5.6 weeks) to an extreme HF arm of 36.25 Gy in 5 fractions over 2 weeks. Eligible patients have intermediate risk prostate cancer and an IPSS score of <15. The primary endpoint is patient-reported GI and GU toxicity. The hypothesis tested is that the extreme HF will reduce patient-reported GI and GU toxicity (superiority design). The sample size is 622 patients. The study is expected to open in late 2017 or early 2018.
The future of moderate HF: will this innovation be widely adopted?
Rogers has developed and described a theory on how clinical innovations are diffused or adopted (19). He describes five elements that interact to determine when adoption will occur: relative advantage, compatibility, complexity, “trialability” and observability. In the next several paragraphs each of these elements will be discussed as they relate to moderate HF.
The element of relative advantage is the extent to which an innovation is perceived to be better than the standard it replaces. The strongest case for moderate HF comes from the three large NI trials which demonstrate, at this point in time, that moderate HF is “not worse than” CF. Unless longer follow-up demonstrates superiority, relative advantage is not likely to drive adoption.
Compatibility is the extent to which an innovation is perceived as being compatible with existing values and needs of potential adopters. Moderate HF involves fewer overall treatments and in the fee-for-service model leads to lower levels of reimbursement. Alternatively, in a capitated model moderate HF may be financially advantageous to practitioners. The present dominance of fee-for-service in the United States suggests that diffusion will be slow.
Complexity in this context is related to the perceived difficulty understanding and implementing the innovation. Moderate HF cannot be considered any more complex that CF. The machines and techniques are the same; the only difference is the daily radiation dose. Complexity cannot reasonably be seen as preventing diffusion of moderate HF.
“Trialability” is the extent to which individuals can explore implementation of the procedure and see for themselves the acceptability to patients and outcomes. Given that prostate cancer outcomes take several years to develop and severe complications are rare, moderate HF should not be considered very “trialable” and individual practitioners will need to rely on the existing information from clinical trials. This element is not likely to positively drive adoption of moderate HF.
The final element is observability, which is the extent to which the results of innovation are visible to others. The results of the most recent NI trials have been published in high-visibility journals and over the last several years moderate HF has been the subject of multiple panels at scientific meetings across the globe. In the last 5 years more than 20 review papers examining HF have been published. Finally, the ASTRO, together with the American Society of Clinical Oncology (ASCO) and the American Urological Association (AUA), has created a consensus, evidence-based guideline on the subject which will be published in 2018. Prostate HF is clearly visible in the scholarly literature and at scientific meetings. If the technique is not adopted it can hardly be blamed on lack of observability.
A recent National Cancer Database analysis has found that HF has increased in the years from 2004–2013 in the United States, reaching 14% in 2013 (20). The fastest growing method of HF is the extreme technique described in another article in this issue; extreme HF increased from 0.3% in 2004 to 8.5% in 2013. This is unexpected given that the quantity and quality of evidence supporting extreme HF is lower than that supporting moderate HF. It will be of great interest to monitor these trends as evidence matures and health care reform continues. For practitioners interested in judicious use of resources and patients’ convenience, a moderately hypofractionated regimen can be presented confidently and discussed with patients as an alternative to CF.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hamdy FC, Donovan JL, Lane JA, et al. 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 2016;375:1415-24. [Crossref] [PubMed]
- Dearnaley DP, Jovic G, Syndikus I, et al. Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: long-term results from the MRC RT01 randomised controlled trial. Lancet Oncol 2014;15:464-73. [Crossref] [PubMed]
- Beckendorf V, Guerif S, Le Prise E, et al. 70 Gy versus 80 Gy in localized prostate cancer: 5-year results of GETUG 06 randomized trial. Int J Radiat Oncol Biol Phys 2011;80:1056-63. [Crossref] [PubMed]
- Zietman AL, Bae K, Slater JD, et al. Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long-term results from proton radiation oncology group/american college of radiology 95-09. J Clin Oncol 2010;28:1106-11. [Crossref] [PubMed]
- Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys 1999;43:1095-101. [Crossref] [PubMed]
- Cabrera AR, Lee WR. Hypofractionation for clinically localized prostate cancer. Semin Radiat Oncol 2013;23:191-7. [Crossref] [PubMed]
- Lukka H, Hayter C, Julian JA, et al. Randomized trial comparing two fractionation schedules for patients with localized prostate cancer. J Clin Oncol 2005;23:6132-8. [Crossref] [PubMed]
- Yeoh EE, Botten RJ, Butters J, et al. Hypofractionated versus conventionally fractionated radiotherapy for prostate carcinoma: final results of phase III randomized trial. Int J Radiat Oncol Biol Phys 2011;81:1271-8. [Crossref] [PubMed]
- Arcangeli G, Saracino B, Arcangeli S, et al. Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III Randomized Trial. J Clin Oncol 2017;35:1891-7. [Crossref] [PubMed]
- Pollack A, Walker G, Horwitz EM, et al. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol 2013;31:3860-8. [Crossref] [PubMed]
- Hoffman KE, Voong KR, Levy LB, et al. Randomized trial of hypofractionated dose-escalated intensity modulated radiation therapy versus conventionally fractionated intensity modulated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2016;96:S32. [Crossref]
- Incrocci L, Wortel RC, Alemayehu WG, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol 2016;17:1061-9. [Crossref] [PubMed]
- Aluwini S, Pos F, Schimmel E, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol 2016;17:464-74. [Crossref] [PubMed]
- Mauri L, D'Agostino RB Sr. Challenges in the design and interpretation of noninferiority trials. N Engl J Med 2017;377:1357-67. [Crossref] [PubMed]
- Lee WR, Dignam JJ, Amin MB, et al. Randomized Phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol 2016;34:2325-32. [Crossref] [PubMed]
- Dearnaley D, Syndikus I, Mossop H, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 2016;17:1047-60. [Crossref] [PubMed]
- Wilkins A, Mossop H, Syndikus I, et al. Hypofractionated radiotherapy versus conventionally fractionated radiotherapy for patients with intermediate-risk localised prostate cancer: 2-year patient-reported outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 2015;16:1605-16. [Crossref] [PubMed]
- Catton CN, Lukka H, Gu CS, et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol 2017;35:1884-90. [Crossref] [PubMed]
- Rogers E. Diffusion of Innovations. New York: Free Press; 1983.
- Stokes WA, Kavanagh BD, Raben D, et al. Implementation of hypofractionated prostate radiation therapy in the United States: A National Cancer Database analysis. Pract Radiat Oncol 2017;7:270-8. [Crossref] [PubMed]


