Seminal vesicle schwannoma presenting as rectal pain: successful robotic-assisted excision
Introduction
Schwannomas, also known as neurilemmomas, are benign peripheral nerve sheath tumors (1). They are most commonly located in the head and neck, or extremities, less commonly in the mediastinum, retroperitoneum, and very rarely in the pelvis (2,3). A number of familial syndromes are associated with increased risk for schwannoma, including Neurofibromatosis type II, Schwannomatosis, or Carney complex (1). Malignant transformation is incredibly rare (4).
Case presentation
A 62-year-old male presented to gastroenterology with a chief complaint of rectal pain. The pain was exacerbated by defecation and prolonged sitting, was described as sharp in nature, and reached a ten-of-ten severity when at its peak. The patient denied changes in bowel habits or urinary function.
The patient’s medical history was otherwise limited to hypertension, controlled with atenolol, and degenerative disc disease requiring occasional tramadol use. Family history was negative for neoplasms aside from a brain tumor in his father at age 83. He is a nonsmoker and works as a manager at a communications firm.
He was referred to urology clinic for concern of a seminal vesicle mass found on workup for his rectal pain. He was well appearing without detectable abnormalities on abdominal and external genitourinary exams. His rectal exam was significant for a palpable mass on the right superior aspect of the prostate. Urinalysis and complete blood count were unremarkable and the prostate-specific antigen was 3.24 ng/mL.
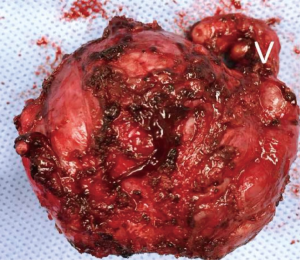
Following initial presentation to gastroenterology at an outside institution, colonoscopy identified mass effect in the rectum suggestive of a protruding external object. A computed tomography (CT) scan of the abdomen and pelvis was then obtained and revealed a mass on the right seminal vesicle. Transrectal ultrasound guided prostate biopsy yielded benign tissue, while final review of the lesion at the authors’ institution returned a diagnosis of schwannoma. To aid in operative planning, magnetic resonance imaging (Figure 1) of the prostate and pelvis was obtained, with and without contrast. This defined a 5.3×4.3×4.3 cm3 mass arising from or abutting the right seminal vesicle, without evidence of invasion into other adjacent structures.
The patient was counseled regarding the risks, benefits, and alternatives to surgical resection, including a review of open and minimally invasive approaches. He elected to pursue robotic-assisted laparoscopic excision of the mass. Under general anesthesia, the patient was placed in the dorsal lithotomy position. A supraumbilical incision was made with Veress needle used to establish pneumoperitoneum, and ports were placed in the standard W-configuration with a right lower quadrant assistant port, similar to that used for prostatectomy or cystectomy.
An approach similar to cystectomy was utilized and the right ureter was identified at its crossing over the iliac vessels. This was dissected free and suspended with a vessel loop to facilitate touch-free manipulation. It was mobilized distally towards the ureterovesical junction at in which point the large seminal vesicle mass was encountered.
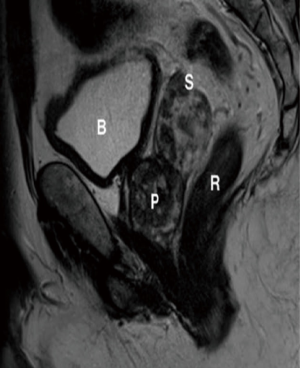
The mass was not adherently to any surrounding structures and was carefully dissected free. The right vas deferens was then transected proximal to the seminal vesicle. The seminal vesicle and right vas deferens were then divided at their insertion into the prostate. The mass was removed en-bloc with the segment of adherent right vas deferens through the supra-umbilical incision (Figure 2).
No drains were placed and the estimated blood loss was 100 mL. The patient did well immediately after surgery and was discharged home on the second post-operative day. Final surgical pathology demonstrated a completely excised schwannoma arising from the soft tissue adjacent to the seminal vesicle. The mass was noted to be adherent to the right seminal vesicle capsule.
Discussion
Schwannomas, also called neurilemmomas, are benign neoplasms of Schwann cells that comprise the myelin sheaths around peripheral nerves. Most schwannomas present between ages 20 to 50 and are sporadic, though 10% may be associated with familial syndromes including Neurofibromatosis type II, Schwannomatosis, or Carney complex (1). Schwannomas most often occur in the head and neck region or in the extremities, with pelvic nerve schwannomas being uncommon (2). To date, only 25 cases of pelvic nerve schwannomas are documented, of which only 6 were related to the seminal vesicle (2,3). Schwannomas, with only exceedingly rare exception, carry no risk of malignant transformation (4).
Other urologically-relevant schwannomas have been reported. One case involving the pudendal nerve presented as 10 years of right testicular and penile pain, while the masses have also been observed in bladder, and scrotal tissues (2,5,6). The majority of documented pelvic schwannomas have been treated in an extirpative fashion via open surgery, while some case reports described laparoscopic approaches and fewer have detailed robotic-assisted excision (7).
Conclusions
Pelvic schwannomas are rare, usually benign neoplasms that may produce significant symptoms requiring treatment, and command a high degree of clinical suspicion for diagnosis. Robotic-assisted laparoscopy offers a minimally invasive approach to the excision of pelvic lesions. To the authors’ knowledge, this report is the first documented complete excision of a seminal vesicle schwannoma utilizing a robotic assisted laparoscopic approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Rodriguez FJ, Stratakis CA, Evans DG. Genetic predisposition to peripheral nerve neoplasia: diagnostic criteria and pathogenesis of neurofibromatoses, Carney complex, and related syndromes. Acta Neuropathol 2012;123:349-67. [Crossref] [PubMed]
- Mazzola CR, Power N, Bilsky MH, et al. Pudendal schwannoma: A case report and literature review. Can Urol Assoc J 2014;8:E199-203. [Crossref] [PubMed]
- Arun G, Chakraborti S, Rai S, et al. Seminal vesicle schwannoma presenting with left hydroureteronephrosis. Urol Ann 2014;6:363-5. [Crossref] [PubMed]
- Nayler SJ, Leiman G, Omar T, et al. Malignant transformation in a schwannoma. Histopathology 1996;29:189-92. [Crossref] [PubMed]
- Ng KJ, Sherif A, McClinton S, et al. Giant ancient schwannoma of the urinary bladder presenting as a pelvic mass. Br J Urol 1993;72:513-4. [Crossref] [PubMed]
- Chan PT, Tripathi S, Low SE, et al. Case report--ancient schwannoma of the scrotum. BMC Urol 2007;7:1. [Crossref] [PubMed]
- Bindal V, Bhatia P, Kalhan S, et al. Robot-assisted excision of a large retroperitoneal schwannoma. JSLS 2014;18:150-4. [Crossref] [PubMed]