Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion
Introduction
Testicular torsion is a surgical emergency affecting 1 in 4,000 boys below the age of 25, and accounting for up to 25% of acute scrotal disease in pediatrics (1). Although testicular torsion can occur at any age, it is most commonly seen in the adolescent population. Testicular torsion is defined as a twisting of the spermatic cord along a longitudinal axis, with resultant ischemia due to compromised blood flow to the testicle. Clinically, testicular torsion presents with an acute onset of scrotal pain, followed by scrotal swelling, nausea and vomiting. A high-riding testis in a transverse lie is often found on physical examination. These findings, in association with an absent cremasteric reflex, are highly suggestive of testicular torsion. The goal in managing testicular torsion is organ salvage. In order to maximize the chances of testicular survival, prompt diagnosis and treatment of testicular torsion is essential. Parameters associated with testis viability include duration of symptoms and the sonographic echotexture of the testis.
Non-surgical management by way of manual detorsion can be attempted, however, its success rate is not known. Manual detorsion is not a definitive treatment option and complete detorsion may not be achieved depending on the degree of twist; testicular ischemia may persist. In addition, testicle may still be at risk for torsion in the future. Shortcomings of manual detorsion can be addressed with surgical exploration which is the gold standard in the management of suspected testicular torsion. During surgical exploration, if the testicle appears viable, an orchiopexy is generally performed. On the contrary, if the testicle appears to be necrotic and dead, an orchiectomy will be the next step. While testicles undergoing orchiopexy are considered viable at the time of surgery, they are often found to undergo atrophy upon follow up. In fact, Lian et al. concluded that half of patients with testicular torsion who undergo “salvage” surgery ultimately go on to develop testicular atrophy (2). Although studies have looked at factors predicting testicular viability during surgical exploration, there is far less literature on what predicts testicular atrophy following orchiopexy and thus the true salvage rates.
It is well documented that there is a 4 to 8 h window of time from the onset of symptoms to surgery that is needed in order to save a torsed testicle (3). Delays in seeking medical care result in higher chances of needing an orchiectomy, as well as the potential burden of impaired fertility. Ramachandra et al. demonstrated through multivariate analysis of the factors associated with testicular salvage, that duration of symptoms of less than 6 h was a significant predictor of testicular salvage. They found that the median duration of pain was significantly longer in patients who underwent orchiectomy versus orchidopexy. Similar findings were seen with respect to time to operating room from initial presentation. They concluded that time to presentation is in fact the most important factor in determining salvageability of the testicle in testicular torsion. If surgical exploration is delayed, testicular atrophy will occur by 6 to 8 h, with necrosis ensuing within 8 to 10 h of initial presentation. Salvage rates of over 90% are seen when surgical exploration is performed within 6 h of the onset of symptoms, decreasing to 50% when symptoms last beyond 12 h. The chance of testicular salvage is less than 10%, when symptoms have been present for over 24 h (4).
At surgical exploration, the spermatic cord is seen twisted a variable number of times around its longitudinal axis. There is scant data regarding the degree of twisting found at surgical exploration and its association with testis outcomes. Animal models have demonstrated a relationship between various testicular outcomes and degrees of twisting in the spermatic cord (5-8). In humans, Filho et al. demonstrated that the degree of testicular rotation has a multiplicative effect on the role of presentation delay in testicular torsion. Greater degree of testicular rotation is seen in patients undergoing orchidectomy vs. orchiopexy. However, testicular atrophy rates at follow-up were not measured (9). The purpose of our study is to further explore how the degree of torsion factors into testicular outcome. It is hypothesized that the greater number of twists of the spermatic cord would offer more obstruction of the vasculature and thus a lower salvage rate based on immediate intraoperative findings (orchiectomy) along with delayed atrophy of the testicle at follow-up.
Methods
Data collection
After obtaining institutional review board approval, we reviewed the records of 229 adolescent males who presented with testicular torsion to our institution using ICD-9 and ICD-10 codes for testicular torsion (608.20 and N44.00, respectively) and CPT codes for testis detorsion with contralateral fixation or orchiectomy (54600 or 54520, respectively). We reviewed patient charts to obtain demographics, descriptive information, clinical presentation (duration of pain), imaging (scrotal ultrasound), intraoperative findings (degree of spermatic cord twisting), and if orchiopexy or orchiectomy was performed. Most testes which remained dark-colored even after detorsion were removed, however, this was largely determined by the surgeons' judgement for the possibility of testicular recovery with an orchiopexy procedure. Finally, follow-up clinic notes were reviewed for the presence of postoperative testicular atrophy after orchiopexy (defined as a >20% difference in volume when compared to the contralateral testis based on obvious physical examination findings, orchidometry, or sonographic measurements, depending on the clinician’s preference). We excluded patients without documentation of both the number of twists and duration of symptoms, those with intermittent pain upon presentation, symptom onset over 24 h from presentation (due to the assumption that there is a low risk of salvage after this time), boys under 11 years old (as assessment of the spermatic vessels along with symptomatology is more difficult and unreliable in smaller patients) or over 18 years old, and patients with less than one month follow-up (as testicular examination and measurements are misleading this early after surgery due to postoperative edema and inflammation). Testicular outcome was defined as viable (orchiopexy with adequate growth at the last clinic follow-up) or non-salvageable (orchiectomy or orchiopexy with subsequent atrophy).
Data analysis
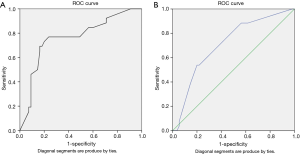
Descriptive data including age, laterality of the affected testicle, degrees of torsion, median time to surgery, intervention, and outcome were collected and analyzed using SPSS statistical analysis software platform (IBM SPSS, Version 22.0, IBM Corp, Armonk, NY, USA, 2013). Chi-Square analysis was applied to categorical data and Wilcoxon rank/Kruskal-Wallis nonparametric test or t-test was used for comparison of continuous data where this was deemed appropriate. A receiver operator characteristic (ROC) curve was used to determine the sensitivity and specificity of the degree of testicular twist for determining the risk of a non-salvageable testis based on orchiectomy or atrophy after orchiopexy. Time to intervention was analyzed in an identical fashion. Youden’s index, which comes without bias, was used for cut-offs for threshold time and degree to maximize specificity, as we wanted to determine testes that would be viable and to not remove them unnecessarily.
Multivariate analysis was then used to predict testicular viability adjusting for the patient’s age, degree of twist, and time until intervention.
Probability of non-salvage
Logistic regression analysis was then performed using the SAS JMP statistical analysis software platform (JMP, Version 13.1, SAS Institute Inc., Cary, NC, USA, 2016) to determine the predictive value of duration of pain and degree of twists for the probability of a non-salvageable testis at the time of surgical exploration. This was then used to estimate the probability of non-salvage for each patient based upon either the duration of pain or degree of twisting alone, with linear probability formulas generated for each variable.
Results
Descriptive data
Eighty-one patients met our inclusion criteria, with a mean age of 14.3 years (median 14; range, 11–17 years) and mean follow-up of 8.0 months (range, 1–48 months) of those who had orchiopexy. Forty-four (54%) torsions were left-sided and 37 were on the right side. Fifty-five (68%) testes were deemed viable at follow-up after orchiopexy, and 26 testes were non-salvageable [7 (8.6%) underwent orchiectomy and 19 had atrophy at follow-up after orchiopexy]. Interestingly, we saw a 25.7% atrophy rate after orchiopexy in our cohort (Table 1). For viable testes versus non-salvageable testes, the mean duration of pain or symptoms was 6.2 (range, 1–21) versus 13.4 h (range, 3–24 h), while mean degree of twisting seen in the torsion at exploration was 375 (range, 90–1,800) versus 529 (range, 180–1,080) degrees (Table 2).
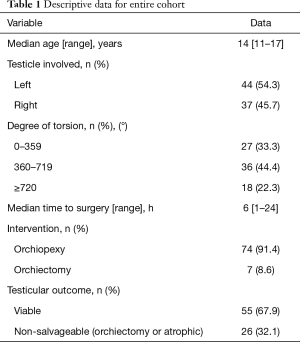
Full table
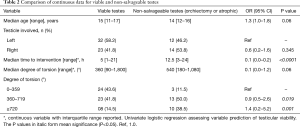
Full table
Predictors of testicular non-salvage
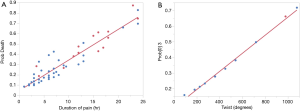
On univariate logistic regression analysis, increased time to intervention (P<0.0001) and the degree of torsion in excess of 360 degrees (P<0.019) were significantly associated with orchiectomy or atrophy. A non-parametric Wilcoxon rank/Kruskal-Wallis analysis confirmed that non-salvageable testicles tended to have significantly higher degrees of twisting when compared to their viable counterparts (P=0.002). An ROC analysis was performed and a threshold time to intervention of 8.5 h [area under the curve (AUC) 0.762, with 95% confidence intervals (CI): 0.645–0.878] would provide a 73% sensitivity and 80% specificity for the prediction of testicular non-salvage (Figure 1A). Also, a cut-off value of 495 degrees of torsion would provide a 53% sensitivity and 80% specificity for predicting non-salvage (AUC 0.711, 95% CI: 0.593–0.830) (Figure 1B).
A multivariate analysis including age, degree of testicular twist, and time until intervention revealed that only patient age and time to intervention were correlated with the risk of a non-salvageable testis (Table 3).
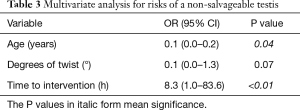
Full table
Probability of non-salvage formula
Logistic regression analysis determined that the degree of twist and duration of pain were predictive of non-salvage on nominal logistic multivariate analysis (P<0.0140, P<0.0006). A bivariate fit of probability of non-salvage based on duration of pain (r2=0.91) and degree of twist (r2=0.99) were then used, separately to estimate the probability of non-salvage. Each variable was then used to generate a linear probability formula, which was as follows:
where “x” was equivalent to the duration of pain in hours (P<0.001) and “y” was equivalent to degree of testicular twist. Overall, a 50% chance of testicular non-salvage would be coincident with 15 h of testicular pain (Figure 2A), while an 860-degree twist (Figure 2B) would coincide with a 50% chance of non-salvage (P<0.001). When both duration and degree were combined, we found a poor correlation coefficient (r2=0.2) and were unfortunately unable to derive a probability formula combining the variables.
Discussion
While the current data regarding the degree of twisting in the spermatic cord’s effects on ultimate testicular outcomes in emergent cases of testicular torsion in humans are limited, animal studies addressing this topic have been performed. In 1986, Cosentino’s team performed studies on rats to first examine the effects of duration of symptoms of testicular torsion. The degree of twisting was fixed at 720° for all rats with duration of symptoms ranging from 0–12 h and found poor histologic findings and fertility rates after a period of recovery starting at 3 h of torsion, as well as markedly decreased fertility rates at 9 h (10). Later, Lee’s group started the investigation into the degree of twisting in testicular torsion by creating torsion in five anesthetized dogs and measuring blood flow blood flow by color Doppler sonography at serial increasing degrees of twisting. They found undetectable flows starting at 450° in all but one dog, who’s flow became undetectable at 540° (5). Other studies have used contrast-enhanced ultrasound in rabbits showing mild drops in perfusion starting at 360° with significantly decreased blood flow starting at 540° (6,7). Heindel’s group decided to look at fertility rates after a period of recovery from various degrees of torsion in rats, reporting significantly decreased fertility starting at 720° of torsion, however, they did not measure 540° twisting between the 360–720° measurements (8).
Filho et al. recently reviewed their records of 117 patients with testis torsion, and found a correlation in time (median of 8.4 h in the orchiopexy group) and degree of torsion in the orchiopexy group. Orchiectomy rates increased starting at 540°, in which duration of symptoms became more relevant in testis survival rates seen between 6 and 12 h. Testes were salvaged in all patients less than 360° and removed in all patients over 1,080° of twisting (9). Based on this study combined with prior animal research, it appears that somewhere between 360–540° of twisting during testicular torsion lies the point where significant occlusion to arterial flow occurs with risk of damage to the testicle. While Filho's was the first study in humans giving a close look into the degree of torsion, we are unsure of the ultimate outcome of the testis based on this study as performance of orchiopexy at surgery was used as the positive outcome instead of using follow-up data via physical examination with or without orchidometry or sonographic measuring.
We are well aware that many testes undergo atrophy even after detorsion and orchiopexy (2). While lesser degrees of torsion may bring back appreciable perfusion to the testicle, along with the surgeons decision to attempt testis salvage based on the possible chance for recovery of testicular function and withholding orchiectomy until it is necessitated, many testicles undergo significant atrophy after being followed long term in the clinic setting. Our study included follow-up data in an attempt to further investigate the significance in the relationship between the degree of twisting in the prognosis of the testis during episodes of testicular torsion. Interestingly our data showed that about 25% of testes undergo atrophy after orchiopexy is performed. While the significance of an atrophied testis is questionable, it is nevertheless compromised in function, and this is clinically relevant and helpful in counseling patients to expectations on how well the testis will grow after a torsion episode if an orchiopexy is performed. Duration of symptoms appeared to be the primary predictor of outcomes. We agree with previous studies that duration of symptoms greater than 6–8 h are at higher risk for testicular demise. While immediate return of blood flow to the testicle can occur after detorsion, the inevitable effects of ischemia can have lasting effects on the viability of a testis. This was seen in our data as the non-salvageable testis rate more than doubled the orchiectomy rate due to a high number of atrophic testes seen at follow-up evaluation.
We were also able to determine the clinical significance of the degree of twisting (separate from the duration of pain as the degree of twist did not significantly contribute to derive a formula which combined both variables) in ultimate testis viability during episodes of testicular torsion in the pediatric population, despite a low sensitivity on ROC analysis. When there is greater than one twist (more than 360 degrees) seen in the spermatic cord at scrotal exploration, there is a higher risk of non-salvage for the testis based on our data. Our study is also the first to derive separate formulas for duration and degree of twisting to determine the probability of a non-salvageable testis during torsion episodes. This probability can be calculated by our formulas, 4 + (3 × duration in hours) and 7 + (0.05 × degree of twisting). The clinical significance of these formulas can be helpful in patients counseling perioperatively and monitoring these testes during follow-up. For example, a testis that is twisted 360 degrees for 6 h will have a 25% and 22% chance of non-salvage based on degree and duration, respectively. However, the role these formulas play into the decision on whether to perform an orchiopexy versus orchiectomy at time of surgery largely depend on clinical judgement, the philosophy of the urologist in the management of a testis with equivocal viability, along with other intraoperative findings.
It is likely that multiple factors including immunologic responses and fluid dynamics are at play in testicular injury during torsion that we cannot appropriately measure in humans with modern science. The later can be appreciated by Bernoulli’s principle, which states that an increase in speed of a fluid occurs simultaneously with a decrease in pressure, such that there is a conservation of energy (11). The theorem is utilized mostly in cardiovascular research, where studies looking at hemodynamics in stenotic arterial lesions have been able to derive a validated simplified formula: 4 × (maximum velocity, m/s)2 = pressure drop, mmHg (12). When fluid moves from a region of high pressure to a region of low pressure, such as is in detorsion, more pressure is behind the fluid and this gives a net force and accelerates the fluid. This can result in pressure-related damage to the testis upon return of flow to further insult the oxidative damage produced with ischemia from prolonged torsion. Therefore, a patient's blood pressure, plasma density, elasticity of the vasculature, and the length along the spermatic cord in which the torsion involves can all potentially play roles in effecting reperfusion dynamics, and thus testicular viability.
The limitations of the study are its retrospective nature and the relatively low number of patients with more than one month of follow-up as well as the degree of twisting dictated in the operative notes. Also, while our study was able to determine clinically helpful formulas using degree of twisting and duration of pain for testicular prognosis, we were unable to combine these variables into one formula to give one definitive probability of non-salvage. While more studies in humans are needed to truly determine the clinical relevance of twisting degree in relation to prognosis of testicular torsion, we must also look to other areas of torsion pathology to better enhance our knowledge in this common emergency room presentation in children.
Conclusions
The viability of the torsed testis can be determined by the duration of symptoms along with degree of twisting, with 15 h of symptom duration and 860 degrees of torsion leading to a 50% probability of non-salvage. Twenty-five percent of testes undergo atrophy after orchiopexy, which proves the concept of reperfusion injury having delayed and lasting effects on testis viability. Further studies are need to accurately characterize the significance of twisting degree in relation to time and prognosis during testicular torsion.
Acknowledgements
We would like to thank Kaitlin Kosinsky in the Department of Urology at Winthrop University Hospital in Mineola, NY, USA for her research coordination in this study.
Footnote
Conflicts of Interest: LS Palmer is a speaker for Laborie. The other authors have no conflicts of interest to declare.
Ethical Statement: We obtained ethical approval to conduct this research by the institutional review board (IRB ID#1048707-1). Informed consent is not required due to the retrospective nature of this study.
References
- Lemini R, Guanà R, Tommasoni N, et al. Predictivity of Clinical Findings and Doppler Ultrasound in Pediatric Acute Scrotum. Urol J 2016;13:2779-83. [PubMed]
- Lian BS, Ong CC, Chiang LW, et al. Factors Predicting Testicular Atrophy after Testicular Salvage following Torsion. Eur J Pediatr Surg 2016;26:17-21. [Crossref] [PubMed]
- Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med 2005;159:1167-71. [Crossref] [PubMed]
- Ramachandra P, Palazzi KL, Holmes NM, et al. Factors influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. West J Emerg Med 2015;16:190-4. [Crossref] [PubMed]
- Lee FT Jr, Winter DB, Madsen FA, et al. Conventional color Doppler velocity sonography versus color Doppler energy sonography for the diagnosis of acute experimental torsion of the spermatic cord. AJR Am J Roentgenol 1996;167:785-90. [Crossref] [PubMed]
- Paltiel HJ, Estrada CR Jr, Alomari AI, et al. Multi-planar dynamic contrast-enhanced ultrasound assessment of blood flow in a rabbit model of testicular torsion. Ultrasound Med Biol 2014;40:361-70. [Crossref] [PubMed]
- Paltiel HJ, Padua HM, Gargollo PC, et al. Contrast-enhanced, real-time volumetric ultrasound imaging of tissue perfusion: preliminary results in a rabbit model of testicular torsion. Phys Med Biol 2011;56:2183-97. [Crossref] [PubMed]
- Heindel RM, Pakyz RE, Reinking LN, et al. The effect of various degrees of unilateral spermatic cord torsion on fertility in the rat. J Urol 1990;144:366-9. [Crossref] [PubMed]
- Dias AC. The Amount of spermatic cord rotation magnifies the timerelated orchidectomy risk in intravaginal testicular torsion. Int Braz J Urol 2016;42:1210-9. [Crossref] [PubMed]
- Cosentino MJ, Nishida M, Rabinowitz R, et al. Histopathology of prepubertal rat testes subjected to various durations of spermatic cord torsion. J Androl 1986;7:23-31. [Crossref] [PubMed]
- Babinsky H. How do wings work? Phys Educ 2003;38:497. [Crossref]
- Faccenda F, Usui Y, Spencer MP. Doppler measurement of the pressure drop caused by arterial stenosis: an experimental study: a case report. Angiology 1985;36:899-905. [Crossref] [PubMed]


