Perspective on cytoreduction and metastasis-directed therapy in node positive and metastatic urothelial carcinoma of the bladder
Introduction
Guidelines advocate to offer radical cystectomy to patients with localized muscle invasive bladder cancer (MIBC) defined as stage T2-4aN0M0 MIBC (1). However, the optimal management of patients presenting with node positive (N+) MIBC is less clear. Cisplatin based multi-agent chemotherapy is standard of care for patients diagnosed with metastatic urothelial carcinoma of the bladder (mUCB). Nevertheless, outcome remains poor and complete cure extremely rare. This situation is waiting for improvement. The place of immunotherapy in the setting of mUCB is currently explored and promising results have been published in a subgroup of the patients (2).
A multidisciplinary approach combining systemic therapy with a local treatment, either radiation or surgery, might be of interest for patients with N+ MIBC or mUCB. It is an old concept that the elimination of the primary tumor may affect further metastatic progression by eliminating secretions that promote cancer cell growth in distant organs resulting in improved survival as has been proven for cytoreduction in other solid cancers (3,4). It has also been postulated that metastasis-directed treatment of oligometastasis could have clinical benefits in terms of disease control or survival while even possibly postponing or omitting the side-effects of a systemic treatment (5). Either surgery or high dose radiation therapy can be applied in these 2 scenarios in order to try to improve survival or at least delay disease progression. These concepts are now explored in several types of solid tumors (6-11), but has been scarcely explored in mUCB. Three recently published articles reviewed the available experience for mUCB demonstrating the renewed interest in the subject. One of the reviews is on the role of surgery in advanced MIBC and mUCB (12), one on surgical treatment after induction chemotherapy (consolidation cystectomy and lymphadenectomy) (13) and one on metastasectomy (14). A few interesting and radiotherapy experiences can be added.
The purpose of this article is to discuss the perspectives which are opened by these data. Three questions have to be answered: (I) Can radical cystectomy or high dose local radiotherapy (cytoreduction) after chemotherapy prolong survival in node positive MIBC and mUCB? (II) Can metastasis-directed therapy (metastasectomy or irradiation) prolong survival in mUCB? (III) Which clinical trial(s) must be performed?
Can radical cystectomy or high dose local radiotherapy after chemotherapy prolong survival in node positive MIBC and mUCB?
Node positive MIBC
Several publications mention the possible long-time survival in pathologically node positive BC which were clinically node negative (cN0) at time of radical cystectomy and lymphadenectomy (15).
Mills et al. (16) found in 83 cN0 patients that survival was best with few and small, unsuspected lymph node metastasis and those without lymph node capsule perforation have the best results after removal.
Steven and Poulsen (17) described the results of extended pelvic lymphadenectomy at the time of radical cystectomy without any additional treatment. The node dissection began at the distal aorta, including the common, external and internal iliac nodes and the periaortic, presacral and obturator fossa nodes. Of 336 patients 64 (19%) had nodal metastasis. Their overall survival (OS) at 5 years was 39% while this was 76% for the node negative patients. The location of the nodal involvement had no influence on survival. Dhar et al. (18) compared 2 consecutive series of cT2-3N0M0 patients treated with radical cystectomy and limited pelvic lymph node dissection (n=336) versus extended lymphadenectomy. In the limited dissection, 13% positive nodes were detected and at the extended dissection 26% were node positive. Recurrence-free survival was 67% and 77% in the limited and extended lymphadenectomy group respectively.
Small trials evaluated the outcome of clinically node positive (cN+) MIBC treated with radical cystectomy. Herr and Donat (19) reported on 84 patients with grossly positive (cN2-3) disease found at cystectomy, treated with extended lymph node dissection. At 10 years 20 patients (24%) were still alive. Clinical T2 UCB did better than higher cT stages. Tarin et al. (20) reported on the effect of the level of lymph node involvement and lymphadenectomy on recurrence-free survival and disease-specific survival in 114 UCB. Positive common iliac lymph nodes did not worse than those with positive lymph nodes restricted to the true pelvis. But the number of positive nodes was an independent predictor of worse outcome. The 42 pN3 UCB had a recurrence-free survival of 25% at 5 years.
Herr et al. (21) reported on 80 cT3-4, N2-3, M0 BC treated with induction chemotherapy followed by radical cystectomy and lymphadenectomy. No viable tumor was present at post chemotherapy surgery in 30% (24/80), pathologically confirming a complete response to the chemotherapy. Residual viable cancer was completely resected in 49 patients, resulting in a final response after surgery and 20 of them survived for a minimum of 5 years. The post-chemotherapy surgery did not benefit those who failed complete or partial response to chemotherapy. Meijer et al. (22) reported on 114 node positive BC patients treated with induction chemotherapy followed by surgery. In case of complete pathological response to the induction chemo, present in 35%, the median cancer-specific survival (CSS) was 127 months and 5 years CSS was 63.5%. For the whole group of patients this was only 29.2%. Recent results of induction chemotherapy followed by radical cystectomy and lymphadenectomy, comes from a large multicenter study (23). A series of 304 cN1-3 is described. Complete pN0 was obtained in 14.5%. This was correlated with the best OS. Negative surgical margins and the removal of at least 15 lymph nodes were good prognostic parameters. Other recent results on clinically node-positive UCB come from MD Anderson cancer center (24). In 55 patients with clinically pelvic or retroperitoneal lymph nodes, the median CSS was 26%. But the 5-year CSS for those patients who were rendered pN0 by chemotherapy became 66% while it was only 12% for the pN+. In a series of 60 urothelial carcinomas with lymph node metastasis Urakami et al. (25) found at a multivariate analysis, clinical tumor response to preoperative chemotherapy an independent prognostic factor for OS. They also found pathological negative lymph nodes, negative resection margins, more nodes removed and no lymphovascular invasion to be independent post-surgical prognostic parameters.
Azuma et al. (26) published the results of a bladder preservation therapy in 34 cT2-4, N1-2 UCB treated with balloon-occluded intra-arterial infusion with cisplatin and gemcitabine along with 60Gy of irradiation. The progression free survival at 5 years with intact bladder was 37.5% in the N2 disease and OS was 30.6%. In N1 tumors the progression free survival and OS were 65.8 and 71.8% respectively.
From all these data, the following can be concluded. Historically, nodal involvement was considered as non-curable disease and it was common to abort a planned cystectomy, with however very bad outcomes (27). All the above-mentioned results demonstrate that some nodal involvement, even grossly, can be cured in selected patients. The removal of more lymph nodes during surgery gives longer disease-free survival and cure. Good prognosis is linked to T stage, the volume and the number of the nodal invasion, R0 resection and above all the response to neoadjuvant cisplatin based multi agent chemotherapy. Alternatives to surgery, with combination of chemo and irradiation, are possible.
mUCB
A recent interesting observational study (28) based on US National Cancer Data Base, identified 3,753 sufficiently documented patients who received multi agent systemic chemotherapy. Of them, 248 received cystectomy and 49 were treated with high intensity local radiotherapy of more than 50 Gy (median dose 59.4 Gy). The 3,456 other patients received no local treatment (22.66%), TURBT alone (68.75%) or <50 Gy of radiotherapy to the bladder (8.59%). They were called the “conservative group” and compared to the 248 cystectomy or 49 high intensity local radiotherapy patients for overall survival. To account for selection bias observed differences in baseline characteristics of the patients and tumors between both groups a weighted propensity score analysis was used for the comparison. The median follow-up in the weighted population was about 65 months. Median overall survival was significantly longer after cystectomy or high intensity local RT than in the conservative group, 14.92 versus 9.95 months respectively (P<0.01). There was not differentiated between cystectomy and radiotherapy treated patients for this analysis. In multivariable analysis, OS was particularly negatively influenced by advanced local disease (cT3 and more), age and non-academic center. Further analysis of their data demonstrated that OS was 17.71 months when the systemic chemotherapy preceded the local therapy, while it was only 12.42 months when the systemic therapy followed the cytoreductive therapy (P<0.001). The burden of the metastasis was not available in the data used in this study and it is likely that the 297 patients treated with aggressive local treatment are highly selected. In spite of these limitations this article remains an important support for the hypothesis of the usefulness of cytoreduction in mUCB.
Can metastasis-directed therapy (metastasectomy or stereotactic body radiotherapy) improve survival in mUCB?
Metastasectomy or SBRT is mostly performed after cisplatin based chemotherapy with only few reports of up front metastasectomy.
Surgery for metastasis
The first reports on surgical resection of residual disease, including distant metastasis after chemotherapy already date from 1993 (29). Since then several studies were published evaluating the role of surgical resection of metastases in the setting of mUCB. An overview of the results of these trials is presented in Table 1.
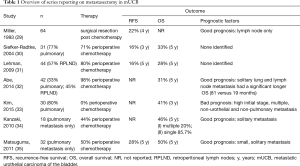
Full table
Radiotherapy for metastasis
Shah et al. (36) radiated metastasis after partial response to chemotherapy in 22 patients (13 with regional lymph nodes) with urothelial carcinoma. The median OS was 49 months, but 8 patients (36%) with nodal or single metastasis were still disease free at 6 years.
Manig et al. (37) explored the predicting factors for survival after irradiated metastasis of UCB in 63 patients. On univariate analysis survival was negatively influenced by the Karnofsky performance score, initial N-category and a low radiation dose (i.e., doses <20 Gy in 2 Gy fractions. The latter remained significant in multivariate analysis.
From all these data, one can conclude that single and small metastasis had a better survival than large and multiple. R0 resection and response to chemotherapy were also independent prognostic factors. If irradiation is used higher doses are recommended. By the lack of a randomized clinical trial one cannot conclude that these patients live longer than when only chemotherapy should have been used. The above-mentioned good results are only hypothesis generating in that direction.
An interesting phase I/II trial (NCT02826564) uses the combination of pembrolizumab with stereotactic body radiotherapy in mUCB and investigates a possible synergistic anti-cancer immune effect (38).
Which clinical trial(s) must be performed?
The small number of reports on local treatment of mUCB clearly demonstrate that this treatment is mainly applied in highly selected cases and/or in few centers. It does not reflect what can be obtained by this approach on a large scale. Since many years it is suggested that only a randomized clinical trial can provide the necessary evidence to defend a more general application of cytoreduction and local treatment of metastasis in mUCB.
Although the scientific proof with a randomized trial of the usefulness of cystectomy in node positive disease, but M0, is not delivered there are multiple observational studies that deliver many arguments in this direction. In our view, it would be ethically incorrect to propose a possible randomization to not performing cystectomy and lymph node ablation after neoadjuvant chemotherapy.
The real unsolved questions are in the setting of mUCB whether one should do a cystectomy in case of a synchronic metastasis or metastasis ablation if it appears after cystectomy.
In the first condition, one should perform a randomized trial in which we propose cystectomy + lymphadenectomy only in those with minimal or no disease left after induction chemotherapy, non-responders to chemotherapy having a very bad prognosis. This implies that patients are sufficiently fit for both therapies and that it is technically possible to obtain a R0 resection after surgery. Unfit patients or patients refusing cystectomy and urinary diversion can be offered a combination with radiotherapy. If it concerns a single metastasis local treatment can be proposed. In the conservative arm cystectomy + lymphadenectomy is not performed, only systemic therapy and palliation are given according to symptoms.
In a second randomized trial, the usefulness of metastasis ablation after chemotherapy can be explored. Distant, visceral metastasis should be restricted to one. The non-responders to the chemo are excluded for further aggressive treatment. The velocity of the disease progression was not addressed in any of the reports discussed in this paper but undoubtedly plays a role in the selection of the patients who can benefit from this treatment. Initial T4 tumors should be excluded because this was an independent bad prognostic factor. The control arm will consist of systemic treatment alone.
The recent research on tumor biology to define its aggressiveness and metastatic potential can become the most important factor in selecting patients. This was not yet addressed in any of the publications referred in this article.
Whether cytoreductive therapy provokes also better quality of live has been explored scarcely. Only one study addressed this question (39). It appeared that symptomatic patients had a better life afterwards, but asymptomatic patients often had a worse quality of life after the treatment. This aspect should certainly be taken into consideration in any future study on the treatment of mUCB.
The vast majority of the mUCB mentioned in the above publications have been treated with surgery but it seems highly probable that high dose radiation can achieve similar results. The choice among them can depend on the fact that the metastasis is easily resectable with low morbidity and negative margins. The need for more correct staging of the disease can also play role in favor of surgery, but with improved imaging this role is diminishing. Radiation therapy can eventually be combined with the chemotherapy in patients who refuse surgery or in whom surgery is technically difficult and with mayor risks. Possible side effects of radiation versus surgery should be taken into account and finally it is the informed patient who takes the decision. To obtain these goals, a well collaborating multidisciplinary team seems essential.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Milowsky MI, Rumble RB, Booth CM, et al. Guideline on Muscle-Invasive and Metastatic Bladder Cancer (European Association of Urology Guideline): American Society of Clinical Oncology Clinical Practice Guideline Endorsement. J Clin Oncol 2016;34:1945-52. [Crossref] [PubMed]
- Rosenberg JE, Hoffman-Censits J, Powles T, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 2016;387:1909-20. [Crossref] [PubMed]
- Bristow RE, Tomacruz RS, Armstrong DK, et al. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 2002;20:1248-59. [Crossref] [PubMed]
- Flanigan RC, Mickisch G, Sylvester R, et al. Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis. J Urol 2004;171:1071-6. [Crossref] [PubMed]
- Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol 2011;8:378-82. [PubMed]
- Ost P, Bossi A, Decaestecker K, et al. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol 2015;67:852-63. [Crossref] [PubMed]
- Decaestecker K, De Meerleer G, Ameye F, et al. Surveillance or metastasis-directed Therapy for OligoMetastatic Prostate cancer recurrence (STOMP): study protocol for a randomized phase II trial. BMC Cancer 2014;14:671. [Crossref] [PubMed]
- Poelaert F, Verbaeys C, Rappe B, et al. Cytoreductive Prostatectomy for Metastatic Prostate Cancer: First Lessons Learned From the Multicentric Prospective Local Treatment of Metastatic Prostate Cancer (LoMP) Trial. Urology 2017;106:146-52. [Crossref] [PubMed]
- Ahmed KA, Torres-Roca JF. Stereotactic Body Radiotherapy in the Management of Oligometastatic Disease. Cancer Control 2016;23:21-9. [Crossref] [PubMed]
- Tree AC, Khoo VS, Eeles RA, et al. Stereotactic body radiotherapy for oligometastases. Lancet Oncol 2013;14:e28-37. [Crossref] [PubMed]
- Tonyali S, Yazici S. Does solitary- and organ-confined metastasectomy really improve survival in advanced urologic malignancies? Int Urol Nephrol 2016;48:671-80. [Crossref] [PubMed]
- Abufaraj M, Gust K, Moschini M, et al. Management of muscle invasive, locally advanced and metastatic urothelial carcinoma of the bladder: a literature review with emphasis on the role of surgery. Transl Androl Urol 2016;5:735-44. [Crossref] [PubMed]
- Tyson MD, Chang SS, Keegan KA. Role of consolidative surgical therapy in patients with locally advanced or regionally metastatic bladder cancer. Bladder (San Franc) 2016.3. [PubMed]
- Patel V, Collazo Lorduy A, Stern A, et al. Survival after Metastasectomy for Metastatic Urothelial Carcinoma: A Systematic Review and Meta-Analysis. Bladder Cancer 2017;3:121-32. [Crossref] [PubMed]
- Zehnder P, Studer UE, Daneshmand S, et al. Outcomes of radical cystectomy with extended lymphadenectomy alone in patients with lymph node-positive bladder cancer who are unfit for or who decline adjuvant chemotherapy. BJU Int 2014;113:554-60. [Crossref] [PubMed]
- Mills RD, Turner WH, Fleischmann A, et al. Pelvic lymph node metastases from bladder cancer: outcome in 83 patients after radical cystectomy and pelvic lymphadenectomy. J Urol 2001;166:19-23. [Crossref] [PubMed]
- Steven K, Poulsen AL. Radical cystectomy and extended pelvic lymphadenectomy: survival of patients with lymph node metastasis above the bifurcation of the common iliac vessels treated with surgery only. J Urol 2007;178:1218-23; discussion 1223-4. [Crossref] [PubMed]
- Dhar NB, Klein EA, Reuther AM, et al. Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol 2008;179:873-8; discussion 878. [Crossref] [PubMed]
- Herr HW, Donat SM. Outcome of patients with grossly node positive bladder cancer after pelvic lymph node dissection and radical cystectomy. J Urol 2001;165:62-4; discussion 64. [Crossref] [PubMed]
- Tarin TV, Power NE, Ehdaie B, et al. Lymph node-positive bladder cancer treated with radical cystectomy and lymphadenectomy: effect of the level of node positivity. Eur Urol 2012;61:1025-30. [Crossref] [PubMed]
- Herr HW, Donat SM, Bajorin DF. Post-chemotherapy surgery in patients with unresectable or regionally metastatic bladder cancer. J Urol 2001;165:811-4. [Crossref] [PubMed]
- Meijer RP, Mertens LS, van Rhijn BW, et al. Induction chemotherapy followed by surgery in node positive bladder cancer. Urology 2014;83:134-9. [Crossref] [PubMed]
- Zargar-Shoshtari K, Zargar H, Lotan Y, et al. A Multi-Institutional Analysis of Outcomes of Patients with Clinically Node Positive Urothelial Bladder Cancer Treated with Induction Chemotherapy and Radical Cystectomy. J Urol 2016;195:53-9. [Crossref] [PubMed]
- Ho PL, Willis DL, Patil J, et al. Outcome of patients with clinically node-positive bladder cancer undergoing consolidative surgery after preoperative chemotherapy: The M.D. Anderson Cancer Center Experience. Urol Oncol 2016;34:59.e1-8. [Crossref] [PubMed]
- Urakami S, Yuasa T, Yamamoto S, et al. Clinical response to induction chemotherapy predicts improved survival outcome in urothelial carcinoma with clinical lymph nodal metastasis treated by consolidative surgery. Int J Clin Oncol 2015;20:1171-8. [Crossref] [PubMed]
- Azuma H, Inamoto T, Takahara K, et al. The novel bladder preservation therapy BOAI-CDDP-radiation (OMC-regimen): a new treatment option for invasive bladder cancer patients with lymph node metastasis. Int J Oncol 2014;44:1895-903. [Crossref] [PubMed]
- Guzzo TJ, Rogers CG, Deng CY, et al. Outcomes of patients after aborted radical cystectomy for intraoperative findings of metastatic disease. BJU Int 2008;102:1539-43. [Crossref] [PubMed]
- Seisen T, Sun M, Leow JJ, et al. Efficacy of High-Intensity Local Treatment for Metastatic Urothelial Carcinoma of the Bladder: A Propensity Score-Weighted Analysis From the National Cancer Data Base. J Clin Oncol 2016;34:3529-36. [Crossref] [PubMed]
- Miller RS, Freiha FS, Reese JH, et al. Cisplatin, methotrexate and vinblastine plus surgical restaging for patients with advanced transitional cell carcinoma of the urothelium. J Urol 1993;150:65-9. [Crossref] [PubMed]
- Siefker-Radtke AO, Walsh GL, Pisters LL, et al. Is there a role for surgery in the management of metastatic urothelial cancer? The M. D. Anderson experience. J Urol 2004;171:145-8. [Crossref] [PubMed]
- Lehmann J, Suttmann H, Albers P, et al. Surgery for metastatic urothelial carcinoma with curative intent: the German experience (AUO AB 30/05). Eur Urol 2009;55:1293-9. [Crossref] [PubMed]
- Abe T, Kitamura H, Obara W, et al. Outcome of metastasectomy for urothelial carcinoma: a multi-institutional retrospective study in Japan. J Urol 2014;191:932-6. [Crossref] [PubMed]
- Kim T, Ahn JH, You D, et al. Pulmonary Metastasectomy Could Prolong Overall Survival in Select Cases of Metastatic Urinary Tract Cancer. Clin Genitourin Cancer 2015;13:e297-304. [Crossref] [PubMed]
- Kanzaki R, Higashiyama M, Fujiwara A, et al. Outcome of surgical resection of pulmonary metastasis from urinary tract transitional cell carcinoma. Interact Cardiovasc Thorac Surg 2010;11:60-4. [Crossref] [PubMed]
- Matsuguma H, Yoshino I, Ito H, et al. Is there a role for pulmonary metastasectomy with a curative intent in patients with metastatic urinary transitional cell carcinoma? Ann Thorac Surg 2011;92:449-53. [Crossref] [PubMed]
- Shah S, Zhang CA, Hancock S, et al. Consolidative Radiotherapy in Metastatic Urothelial Cancer. Clin Genitourin Cancer 2017;15:685-8. [Crossref] [PubMed]
- Manig L, Kasmann L, Janssen S, et al. Predicting Survival After Irradiation of Metastases from Transitional Carcinoma of the Bladder. Anticancer Res 2016;36:6663-5. [Crossref] [PubMed]
- Sundahl N, De Wolf K, Rottey S, et al. A phase I/II trial of fixed-dose stereotactic body radiotherapy with sequential or concurrent pembrolizumab in metastatic urothelial carcinoma: evaluation of safety and clinical and immunologic response. J Transl Med 2017;15:150. [Crossref] [PubMed]
- Otto T, Krege S, Suhr J, et al. Impact of surgical resection of bladder cancer metastases refractory to systemic therapy on performance score: a phase II trial. Urology 2001;57:55-9. [Crossref] [PubMed]


