Peyronie’s penile plication
Introduction
Peyronie’s disease (PD), an acquired deformity of the penis was first described nearly three centuries ago, however a complete understanding of the etiology or pathophysiology remains elusive. Despite this, many treatments have emerged to correct PD. As new treatments have been developed, awareness of the condition both in the medical and lay public has increased. Both non-operative and surgical treatments are available. Penile plication has become the preferred surgical technique for PD as it can be performed efficiently, safely, with a high success rate, low morbidity, and a low complication rate (1). Various surgical treatments of plication have evolved over the years many times borrowing from prior techniques.
Here in we describe two modern penile plication techniques in detail. Furthermore, we discuss patient selection and will review lessons learned from reviewing a large number of plications.
Evolution of technique
Nesbit described the original plication technique (2), however the modern era of penile plication began with the 16-dot plication described by Gholami et al. (3). The two techniques that follow below both have taken the 16-dot plication and added further modifications. In the Kiel Knots plication by Dr. Osmonov (4) the procedure is modified by burying the knots in a shallow trough of tunica to improve final outcomes by reducing patient discomfort due to palpable sutures. Sutures are also spaced closer together to minimize penile shortening. The penoscrotal plication by Dr. Morey (5) was developed to decrease surgical trauma by avoiding degloving and circumcision. This technique has now been successfully applied to severe curvatures, as well as complex multiplanar deformities. The goal of a penile plication is not to correct the penis to zero degrees, but to make it functional which has been loosely defined as 20 degrees or less by expert opinion (6).
Kiel Knots plication technique
Patient selection
The Kiel Knots plication has successfully been applied for both congenital curvature or PD (4). PD should be stable for at least one year prior to intervention. The extent of curvature should not exceed 60 degrees and there should be no hinge defect or hourglass deformities.
Surgery is performed under general anaesthesia. A 16 French silicone transurethral catheter is placed in the bladder. After circumcision and degloving, a tourniquet is placed around the penile base and 60 cc NaCl 0.9% solution is injected into the corpus cavernosum through a 21-gauge needle. This enables a detailed examination under a simulated full erection. The degree of deviation is measured and the tourniquet is then removed.
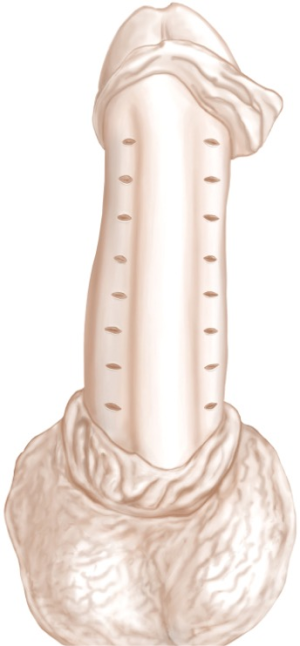
Dorsal curvature (Figure 1)
Buck’s fascia is dissected bilaterally, parallel to the urethra. Incision of the fascia is performed with subsequent dissection up to the tunica albuginea, which is then completely exposed. Using a surgical pen we mark 8 dots bilaterally (16 in total) on the albuginea, beginning from the sulcus coronarius to the penile base. We put the dots in the same place and the same distance between the dots. This helps standardize the “kiel knots” procedure and makes it easier. In case of “over correction” we release one or two knots, till the straightness of the penis is acceptable. Additionally, we try to get at least one set of sutures above and below the level of a maximal curve.The distance between marked dots is approximately 5 mm.
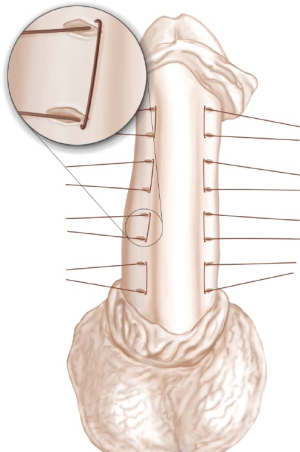
A transverse incision of 5 mm is performed along the marks with a fine knife, without cutting into the corpus cavernosum (Figure 2). This is done to prepare a cavity for the inverted knots. A double-armed 4-0 Gore-Tex suture is placed through the exterior edges of the two adjacent incisions. The double-armed needle is guided from outside to inside on either side so that the knot can be tied inside the incision (Figure 3).
All sutures are knotted after placement of 4 pairs of sutures. All of the sutures are thus tied with 8 knots. The inverted knot technique allows the surgeon to sink the knots into the transverse incision which was made earlier in the corpus cavernosum. If knots remain on the surface, they can be pushed into the incision line with forceps. Finally, the tourniquet is placed on the penis base again to assess the straightness of the penis after injection of additional 60 cc mL NaCl 0.9% into the corpus cavernosum (Figure 4). In case of over-correction, it is possible to undo one of the knots. In case of under-correction, a further knot can be added.
Ventral curvature
Buck’s fascia is dissected longitudinally from the sulcus coronarius to the base of the penis above the neurovascular bundle. Incision of the fascia is made with subsequent dissection up to the tunica albuginea, which is then completely exposed. Hence, we carefully mobilize the dorsal neurovascular bundle. We completely mobilize the dorsal neurovascular bundle to place our inverted knots as medial as possible. We invest time for the subtle mobilization of the bundle to avoid injury to the neurovascular bundle and to reach a maximal surgical benefit. In our experience, there is less shortening and better straightening of the penis with less knots when mobilizing the neurovascular bundle in comparison to lateral positioning of the knots if no neurovascular mobilization is performed. Once again a surgical pen is used to mark 8 dots bilaterally (16 in total) on the albuginea. An incision of 5 mm is made along the marks with a fine scalpel without cutting into the Corpus cavernosum. The distance between the marked dots is again approximately 5 mm and inverted plication sutures are placed with 4-0 Gore-Tex sutures. 8 suture knots are done in total (Figure 3). The straightness of the penis is then re-evaluated as described above (Figure 4).
Finally, Buck’s fascia and the dartos fascia are both closed using 5-0 Vicryl suture, and the skin is closed using 4-0 Vicryl suture. The penis is wrapped. The catheter is removed on the first postoperative day and the patient discharged from the hospital.
In cases with lateral curves we perform the “Kiel knots” stiches on the opposite corporal body, monolaterally. In most of these cases however, there is a combination of dorsal and lateral penile deviation, and for that reason stiches are placed parallel to the urethra. In cases of complex torsion we perform a grafting procedure.
Results
In a series of 20 patients, the average operation time was 64 minutes (4). All patients underwent follow-up examinations at 6 monthly intervals in our outpatient clinic. The follow-up time was at least 26 months.
In the first 8 months none of the patients reported recurrence of PD. Two out of 20 patients (10%) reported a mild recurrence of PD after 24 months. Three patients (15%) showed moderate erectile dysfunction one year postoperatively in an IIEF questionnaire. However, whether the penile plication was the cause of the PD or whether these patients merely had PD with concomitant ED could not be delineated.
A total of 18 patients (90%) were satisfied with the cosmetic result. Penile shortening was the most frequent complication in the first 6 months, reported by 7 patients (35%). All of these patients had PD of less than 60°. One of these 7 patients found that sexual activity was affected by loss of penile length. After 6 months, however, penile shortening was no longer reported. Objectively stretched penile length before and after surgery was compared. After 26 months, penile shortening was observed in 6 patients (30%). Loss of penile length ranged from 0.5 to 1 cm. None of the patients reported bothersome sensations due to suture knots. No patients developed buckling intraoperatively nor during follow-up.
One of the 2 patients with mild PD recurrence underwent salvage surgery by Schroeder Essed technique. The other is under treatment with a vacuum device. In the group of 6 patients with penile shortening, one patient underwent scrotoplasty, and the remaining 5 are currently undergoing treatment with a vacuum device. In general, we recommend low dose phosphodiesterase-5 inhibitor therapy (Sildenafil 25 mg/day), which is started at 4 weeks postoperatively and continued for 3 months. Additionally, we recommend use of a vacuum device every day 3–5 min for 12 weeks.
Benefits of Kiel Knot technique
Avoidance of palpable suture knots
Often palpable suture knots may cause discomfort during sexual intercourse (3).
We were able to significantly decrease a number of patients with bothersome sensations due to suture knots with our modified Schroeder-Essed technique (7). We recommend using non-absorbable Gore-Tex sutures, which are significantly softer than 2-0 Ticron (Davis and Geck, Wayne, NJ, USA) previously used for 16-dot technique.
Avoidance of penile shortening
The distance between the suture knots in the 16 dots-procedure can be up to 1.5 cm. Our own experience has led us to minimize this distance. We therefore propose to reduce the maximum distance to 5 mm, which also means that we propose more plications instead of greater distance between dots. This has helped us to reduce the extent of penile shortening. As a further benefit, we did not record paraesthesia of the penis, especially in the glans, due to the kinking of nerve fibbers in patients with ventral curvatures.
Minimally invasive penoscrotal plication technique
Patient selection
Patients may have mild to severe curvature and/or a wide array of deformities including multiplanar complex deformities (5).
Prior to draping the patient, an intracavernosal injection is performed using 20 mcg of alprostadil (PGE1). The base of the penis is then shaved and the patient is prepped and draped in the usual sterile fashion. The penis is now gripped aggressively at the base to evaluate the extent, direction, and location of the penile deformity. This will determine the location of the skin incision and helps in planning plication suture location. If a poor erection has been induced, additional 20 mcg of alprostadil may be administered or an artificial erection may be induced using injectable saline with a butterfly needle.
For dorsal deformities, necessitating ventrally placed plicating sutures a 14 F Foley catheter is placed to aid in urethral identification and prevent urethral injury.
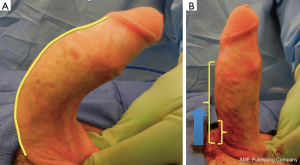
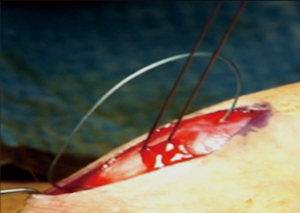
A 2 to 3 cm longitudinal incision is made along the proximal or mid shaft. After the initial dissection is carried through the dartos and Buck’s fascia Senn retractors are used to enable further proximal, distal and rotational penile exposure of the tunica albuginea. A circumscribing and degloving incision is not performed (Figure 5). The depicted example in Figure 5 was a patient with congenital penile curvature that had previously undergone two prior failed plications at an outside institution via circumscribing incisions. Figure 5 demonstrates that the entire shaft can be accessed via a 2 to 3 cm proximal shaft incision. Once exposed, the tunica albuginea is then repeatedly corrected with short plication sutures spanning 15 to 20 mm while retracting the incision over areas of greatest convexity. Non-absorbable 2-0 Ethibond braided sutures are placed in an inverted mattress “near to far, far to near,” configuration (Figure 6) and tied down using 4 knots. The penis is re-examined after each suture by gripping the base and additional sutures placed until satisfactory correction of the deformity. We do not have a maximum number of sutures. The most sutures ever placed during a plication was 21. Once the deformity has adequately been corrected the wound is closed in 3 layers. Buck’s fascia is closed in running fashion using 3-0 Monocryl suture. One must adequately reach under the dartos in closing Buck’s as the tissue will retract. The second layer is brought together by closing the Dartos in similar running fashion using 3-0 Monocryl. Finally the skin is closed in subcuticular fashion with 4-0 Monocryl and then Dermabond applied. During the closure if the retracted edges are not adequately brought together the penile skin and underlying Dartos will seem to become adherent, fixed and less mobile on the shaft.
Patients with torsion are seemingly more complex deformities to correct. However, torsion patients essentially have a multiplanar deformity on a high number of planes. In these cases, sutures are placed in a similar fashion to the previously discussed curvatures, however we strongly stress placing sutures proximally first before placing your more distal sutures. This will allow the deformity to untwist as one moves along the shaft finding areas of convexity to correct. These cases may require a greater number of sutures and/or a shorter length to each plicating suture.
Results
This minimally invasive technique for penile plication has been used successfully for mild to severe curvatures as well as for complex multiplanar deformities. In a recent retrospective review of 340 minimally invasive penile plications, the success rate was 98%, giving a failure rate of 2% (n=7) (8). This rate of success compares favorably with that reported in the literature, which is often above 90% (9). In this review, we paid particular attention to the failures. Under-correction seems to be the most common reason for failures. The time to revision surgery supports this notion given that the median time to revision plication was 6 months (range, 3–24 months) after failure. Typically patients know immediately when their penile defect has been under-corrected. Other studies corroborate these findings. Hsieh et al. reported a median time to failure of 38.5 days in a series of 114 patients (10) and Andrews et al. reported that cases having persistent deformity >30 degrees presented at a mean of 2.5 months (11).
In the retrospective review by Cordon et al. (8) only 2 patients presented after 12 months and both of these patients had new deformities. Further evidence supporting the notion that these were under-corrected is that all failures had curvatures of greater than 35 degrees. That is to say patients were not looking to be perfect, they were looking to be functional which is generally regarded as less than 20 degrees (6). Additionally on revision surgery a greater number of plication sutures were used. The mean number of sutures during revision was 9 (range, 4–11) compared to 6 (range, 1–8) on the initial plication.
Factors leading to under-correction
Approximately one third of PD patients will have concomitant ED (12). For those who respond poorly to vasoactive substance intraoperatively, we recommend giving additional injections, or using saline to induce an adequate erection that will delineate the deformity well. We found that 71% (5/7) of failures had a poor intraoperative response to ICI. A poor intraoperative erection will lead to decreased appreciation of the deformity and risks under-correction.
In this series 71% (5/7) of failures had multiplanar deformities and 43% (3/7) severe deformities greater than 60 degrees. Although these clinical factors complicate the repair, we don’t believe these preclude an adequate repair as prior studies have shown high success rates for complex deformities (3,13). Hudak et al. (13) evaluated patient reported outcomes and showed that 95% of patients categorized as complex, (multiplanar deformity or greater than 60 degrees, n=57) reported having adequate straightening of their deformity after plication. In this earlier series, similarly only 3% of these complex deformities required a revision, which is comparable to our current overall revision rate of 2%. In the original 16-dot plication description by Dr. Lue in 2002 he included patients ranging from 30–120 degrees (average 64 degrees) and also reported a 3% failure rate (3). Our experience suggests that complex deformities will require more sutures and increased intraoperative decision-making, but does not predispose to high failure rates. In some, a slightly longer longitudinal incision or a circumcision approach may be reasonable to enable complete penile shaft exposure. Lastly, we strongly advocate sufficient exposure and correction of the entire span of the penile shaft for complex cases, beginning proximally near the penoscrotal junction and extending as distal as necessary to achieve straightening. The example discussed previously in Figure 5 also demonstrates the need for correcting the entire shaft.
Regardless of the specific technique of plication, we believe distributing the tension more evenly over a greater number of sutures leads to more durable correction, potentially less pain with erections in the postoperative period, and less penile shortening.
Conclusions
Penile plication has evolved into a preferred and reliable technique for a variety of penile deformities. A variety of techniques exist, most with high success rates. Failures present early in the postoperative period. Most failures are a result of under-correction. A poorly induced erection intraoperatively may lead to under-correction. Complex deformities do not preclude adequate correction. During revision, plication patients often require a greater number of sutures than their initial plication.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Oberlin DT, Liu JS, Hofer MD, et al. An Analysis of Case Logs From American Urologists in the Treatment of Peyronie's Disease. Urology 2016;87:205-9. [Crossref] [PubMed]
- Nesbit RM. Congenital Curvature of the Phallus: Report of Three Cases with Description of Corrective Operation. J Urol 1965;93:230-2. [Crossref] [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. [Crossref] [PubMed]
- Osmonov DK, Jünemann KP. The "Kiel Knots" Technique for Treatment of Congenital and Aquired Penile Deviation. Advances in Sexual Medicine 2013;3:19-23. [Crossref]
- Dugi DD 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int 2010;105:1440-4. [Crossref] [PubMed]
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- van der Horst C, Martinez Portillo FJ, Seif C, et al. Tunica plication with horizontal incisions of the tunica albuginea in the treatment of congenital penile deviations. Aktuelle Urol 2003;34:478-80. [PubMed]
- Cordon BH, Sundaram V, Hofer MD, et al. Penile Plication as Salvage Strategy for Refractory Peyronie’s Disease Deformities. Urol Pract 2017;4:149-54. [Crossref]
- Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl 2013;15:27-34. [Crossref] [PubMed]
- Hsieh JT, Liu SP, Chen Y, et al. Correction of congenital penile curvature using modified tunical plication with absorbable sutures: the long-term outcome and patient satisfaction. Eur Urol 2007;52:261-6. [Crossref] [PubMed]
- Andrews HO, Al-Akraa M, Pryor JP, et al. The Nesbit operation for Peyronie's disease: an analysis of the failures. BJU Int 2001;87:658-60. [Crossref] [PubMed]
- Bilgutay AN, Pastuszak AW. Peyronie's Disease: A Review of Etiology, Diagnosis, and Management. Curr Sex Health Rep 2015;7:117-31. [Crossref] [PubMed]
- Hudak SJ, Morey AF, Adibi M, et al. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol 2013;189:1019-24. [Crossref] [PubMed]