Overactive pelvic floor muscles (OPFM): improving diagnostic accuracy with clinical examination and functional studies
Introduction
Undiagnosed lower urinary tract symptoms (LUTS) and pelvic pain remain a challenge to medical practitioners. Many of these patients were provisionally diagnosed with chronic pelvic pain, chronic non-bacterial prostatitis, chronic orchialgia and overactive bladder, and have not improved despite multiple regimens of antibiotics, anticholinergics and antispasmodics (1). We believe a majority of these patients have chronically raised pelvic muscle tone, known as overactive pelvic floor muscles (OPFM). Various terms have been used to describe this condition, including hyperactive pelvic floor disorder, pelvic floor tension syndrome, levator ani syndrome and proctalgia fugax.
To date, there is no clear diagnostic criterion or definition for OPFM. According to the International Continence Society, symptoms of OPFM can be broadly divided into categories of lower urinary tract, gastrointestinal, sexual and pain symptoms. LUTS include frequency, urgency, urge incontinence, poor stream and incomplete voiding. Gastrointestinal symptoms include obstructed defecation, anorectal pain, prolapse and incontinence. Sexual symptoms include dyspareunia in females, ejaculatory dysfunction and erectile dysfunction in males, and orgasmic dysfunction in both genders. Pain symptoms are largely localised in the perineum and anterior vaginal wall (2).
OPFM is a diagnosis of exclusion. This condition is diagnosed when patients have symptoms of OPFM outlined above, and were found to have trigger point tenderness on palpation of the pelvic floor muscles and anterior vaginal wall on clinical examination (3-5). However, as most symptoms of OPFM are largely non-specific, the diagnosis of this condition remains a challenge. Whilst pelvic floor palpation may afford the clinician information on the presence of trigger point tenderness and the tone of pelvic floor muscles, it is not possible to objectively quantify muscle tone, and determine what constitutes a normal versus abnormal tone. This leads to poor reproducibility and large inter-observer variability in the diagnosis of OPFM.
Hence, one of the target for future research outlined by the ICS Committee is to identify a method to measure and quantify pelvic muscle tone.
Aims of study
To review the current terminology and diagnostic criteria of OPFM, and identify its functional correlation with cystoscopic and fluoroscopic urodynamic studies (FUDS) including urethral pressure measurements.
Methods
Patients with LUTS refractory to conservative therapy, including bladder retraining and medications for a variety of gamut of storage and voiding disorders were referred to a single, experienced, high-volume urologist in Melbourne, Australia. Patients of both genders were included.
Prospective data from 201 consecutive patients, who underwent flexible cystoscopy and FUDS between January 2014 and January 2016 were extracted. Using pelvic floor tenderness as a key distinguishing examination feature for OPFM, a comparative analysis was performed for patients with and without the examination finding. Pelvic floor muscles were palpated externally over the perineum around the imaginary numbers of a clock, known as the “around-the-clock technique”. The 12 o’clock position aligns with the pubic symphysis and clitoris, three and nine o’clock align with the patients’ ischial tuberosities, and six o’clock aligns with the coccyx.
Factors studied included the range of LUTS, voiding patterns, physical examination, post-void urine residuals, cystoscopic findings and urodynamics, including the maximum urethral closing pressure (MUCP) derived from urethral pressure profilometry. We used a triple-lumen transducer catheter, mounted to a mechanical withdrawal device. Saline was infused via this transurethral catheter at 0.5 mL/min during UPP recording and the catheter was simultaneously withdrawn at 1 mm/s during recording. Bladder pressure and urethral pressure values were digitized and recorded using urodynamic device software.
Statistical methods used for analysis were the Chi-squared test and Student t-test for mean.
This study complied with the principles of the Declaration of Helsinki. The study was approved by our local ethics committee. Informed consent was obtained from all participants.
Results
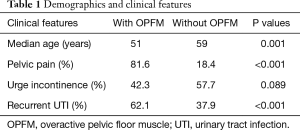
Of the 201 patients recruited, 85 patients were diagnosed with OPFM based on clinical presentation and presence of pelvic floor tenderness on examination (Table 1).
Full table
Younger patients appeared to be affected by OPFM more commonly, occurring at the median age of 51, compared to those without at the age of 59 (P=0.001). Patients with OPFM also have a significantly higher incidence of pelvic pain, 81.6% vs. 18.4% (P<0.001). There was only 1 male patient who were identified to have OPFM.
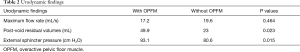
Patients with OPFM have a higher post-void residual volume, 49.9 vs. 23.0 mL (P=0.023), and a higher incidence of recurrent urinary tract infection (UTI), 62.1% vs. 37.9% (P<0.001).
Significant objective differences were also noted between the 2 groups of patients on functional studies with FUDS and urethral pressure measurement. Subjects with OPFM were found to have a higher (MUCP) at 93.1 cm H2O compared to 80.6 cm H2O (P=0.015) (Table 2).
Full table
No statistical differences were seen between the 2 groups with regards to incidence of urgency urinary incontinence (P=0.089), non-bacterial cystitis (P=0.201) and stress incontinence (P=0.78).
Discussion
OPFM implies a physical state of heightened activity within the pelvic floor muscles. Diagnostic criteria for this condition is being developed.
Muscle tone or tension, is measured by the change in resistance or force per unit change in length (6). Clinically, the tone of pelvic floor is assessed by palpation as the resistance is felt when passive stretch is applied to the muscles. Normal contraction refers to contractile activity that occurs in a normal muscle because it is not completely relaxed, but can be controlled voluntarily, or due to reflex activation. On the other hand, muscle spasm is defined as an abnormal/pathological (involuntary) contraction (7).
The relationships between the different sources of muscle tone (active and passive), and their relative contribution of different elements of OPFM remain under investigation. Although speculative, it is possible that in some cases, there is a sequential pattern to the relative contribution of different elements to OPFM (8). For example, a persistent lack of muscle relaxation and/or heightened (but normal) muscular activity may lead to involuntary muscle contraction. This may develop further into a pelvic pain syndrome, involving taut bands and trigger points (9,10). The pain associated with non-relaxing muscles may be caused by the shearing forces between the muscle fibres. In addition, pain can also occur if the muscle becomes ischaemic and releases pain-producing substances, which can occur if the muscle contracts forcefully for too long, and compresses its own blood vessels (9). Prolonged exposure to noxious stimuli may then lead to the up-regulation of nociceptive system. This dysregulation of both the peripheral and central mechanisms of sensory and pain processing consequently leads to hyperalgesia and allodynia (11,12).
Our study demonstrated that OPFM appears to affect younger patients. Not surprisingly, pelvic floor pain is significantly higher in this group, which prompted their initial consultation. OPFM leads to increased bladder outlet resistance, and this is consistent with our results that showed that this group had a higher post-void residual. This may also explain the higher incidence of UTIs seen in these patients.
By using urethral pressure profilometry, we have demonstrated that there is an objective difference in MUCP in patients with OPFM compared to those without. We have found that patients with OPFM have a significantly higher external sphincter pressure, and this appears to be statistically significant.
The systematic use of cystoscopy and urodynamics in the evaluation of OPFM allows the clinician to rapidly rule out other disorders of the bladder neck (e.g., bladder neck obstruction, detrusor sphincter dyssynergia) and storage disorders such as poor bladder compliance, symptoms of which may be identical.
Whilst profilometry has been used often in the evaluation of stress urinary incontinence (13), the systematic incorporation of urethral pressure profilometry in urodynamics remains academic to date. This is because the results obtained are extremely susceptible to artifacts and the degree of relaxation of the patient (14). However, the objective difference in MUCP seen in our study has shown that the option of urethral pressure profilometry should be explored further in the diagnosis of OPFM. Further attempts to standardise the techniques of profilometry, and more research to identify the normal ranges of muscle tone may increase the relevance of this functional study in the future.
Early recognition of OPFM allows earlier tailored intervention for patients. Down-training physiotherapy is an emerging concept for the management of this complex condition, with emphasis on pelvic floor muscle awareness, relaxation exercises, trigger point release techniques, and/or manual stretches (15). For patients undergoing surgery for stress incontinence, the identification of concomitant OPFM and early physiotherapy may reduce risks of post-operative voiding difficulties. Long-term follow-up of these patients is needed to assess their responses to down-training physiotherapy.
When OPFM and detrusor overactivity co-exist, OPFM may be the driving factor. As such, combination therapy with pelvic floor relaxation and pharmaceuticals (anticholinergics/Botox injections) may yield better results than medications alone. Sexual dysfunction such as dyspareunia caused by OPFM may also be amenable to physiotherapy.
Conclusions
Our study has shown that there are distinct characteristics of OPFM on clinical examination and functional studies. In patients with LUTS refractory to conservative treatments, specific urodynamics tests may be useful in sub-categorising patients. When OPFM is diagnosed, the impact on patient management is significant, and targeted intervention with pelvic floor physiotherapy is central in the multimodal approach of this complex condition.
Acknowledgements
We thank Ms. Dawn Hewey for collecting and collating the data from the research participants.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study complied with the principles of the Declaration of Helsinki. The study was approved by our local ethics committee. Informed consent was obtained from all participants.
References
- Loving S, Thomsen T, Jaszczak P, et al. Pelvic floor muscle dysfunctions are prevalent in female chronic pelvic pain: a cross-sectional population-based study. Eur J Pain 2014;18:1259-70. [Crossref] [PubMed]
- Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn 2005;24:374-80. [Crossref] [PubMed]
- Montenegro ML, Mateus-Vasconcelos EC, Rosa e Silva JC, et al. Importance of pelvic muscle tenderness evaluation in women with chronic pelvic pain. Pain Med 2010;11:224-8. [Crossref] [PubMed]
- Fitzgerald CM, Neville CE, Mallinson T, et al. Pelvic floor muscle examination in female chronic pelvic pain. J Reprod Med 2011;56:117-22. [PubMed]
- Dietz HP, Shek KL. The quantification of levator muscle resting tone by digital assessment. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1489-93. [Crossref] [PubMed]
- Simons DG, Mense S. Understanding and measurement of muscle tone as related to clinical muscle pain. Pain 1998;75:1-17. [Crossref] [PubMed]
- Basmajian JV. New views on muscular tone and relaxation. Can Med Assoc J 1957;77:203-5. [PubMed]
- Butrick CW. Pathophysiology of pelvic floor hypertonic disorders. Obstet Gynecol Clin North Am 2009;36:699-705. [Crossref] [PubMed]
- Simons DG, Travell JG, Simons LS, et al. editors. Myofascial Pain and Dysfunction. The Trigger Point Manual. Baltimore: Williams & Wilkins, 1999.
- Doggweiler-Wiygul R. Urologic myofascial pain syndromes. Curr Pain Headache Rep 2004;8:445-51. [Crossref] [PubMed]
- Wright A. editor. Neurophysiology of pain and pain modulation. Pain: a textbook for therapists. London: Churchill Livingston, 2002.
- Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil 1998;79:863-72. [Crossref] [PubMed]
- McGuire EJ, Fitzpatrick CC, Wan J, et al. Clinical assessment of urethral sphincter function. J Urol 1993;150:1452-4. [Crossref] [PubMed]
- Tanagho EA. Membrane and microtransducer catheters: their effectiveness for profilometry of the lower urinary tract. Urol Clin North Am 1979;6:110-9. [PubMed]
- Lukban J, Whitmore K, Kellogg-Spadt S, et al. The effect of manual physical therapy in patients diagnosed with interstitial cystitis, high-tone pelvic floor dysfunction, and sacroiliac dysfunction. Urology 2001;57:121-2. [Crossref] [PubMed]


