A prospective evaluation of penile measures and glans penis sensory changes after penile prosthetic surgery
Introduction
With better designed devices and lower infection rates, satisfaction with inflatable penile prosthesis (IPP) placement for refractory erectile dysfunction (ED) is high, and increasing (1-5). Even though the overall satisfaction is high, subjective penile length reduction is still present (5,6). It seems that there was consensus that penile length will decrease after radical prostatectomy (7-9). However, there is disagreement regarding penile length change after implant, either decrease, no change, or increase (9-14). This uncertainty leads to a dilemma regarding the size of penile prosthesis to place to achieve optimal results and how best to counsel patients on their expected inflated penile length.
Attempting to avoid patient’s complaints of penile shortening after the IPP, some physicians have proposed a more aggressive approach to sizing the cylinder (15), while others have proposed different penile lengthening techniques to be performed concomitantly with the IPP placement (16-18). Obviously, an overly aggressive approach may lead to cylinder aneurysm or fluid loss, or S-shaped deformity (19). On the other hand, undersized IPP will lead to dissatisfaction. Likewise, there are case reports of penile sensation decrease after penile implantation (6,16). However, there was no well-designed research to further support the decrease of penile sensation after the IPP placement at the time of this study.
To better explore this, we carried out this observational study to evaluate changes in penile length, girth, and sensitivities after IPP placement.
Methods
After getting institutional ethics review board approval (URN 2012-04), patients undergoing IPP surgery from August 2012 to January 2013 were invited to participate. The aim of the study was to assess changes in glans penis sensation, erect penile length, and circumference at 6 weeks and 6 months after IPP. Only “de novo” IPP cases were included. Patients with Peyronie’s disease were excluded from the study. Ninety-nine patients underwent Coloplast IPP placement during this period, with 86 meeting inclusion criteria while 62 agreed to participate in this observational study.
The three-piece IPP placement was performed through penoscrotal approach using a lateral scrotal incision under general or regional anesthesia. The lateral incision we created was half the size of a regular penoscrotal approach incision to avoid excessive dissection during surgery and to reduce discomfort after surgery when the penile prosthesis is deflated and the penis falls down over the incision. The length of the implanted cylinders used was exactly matched to intracorporal measurements (10). The measurements for penile girth, length, and sensation were repeated twice every time to guarantee accuracy. Briefly, the length was defined as the distance from pubic symphysis from the tip of glans. The girth was defined as circumference along the mid-shaft of the penis. All patients were in supine position when the measurements were performed. All the procedures and measurements were performed by the same expert surgeon.
Main outcome measures
A week before surgery, erect penile length and circumference, and glans/elbow biothesiometer (Bio-medical Instrument CO., Newbury, OH, Figure 1) readings in amperage (20) were recorded 15 minutes after Trimix (150 mg of papaverine, 50 mcg of prostaglandin E1, and 5 mg of phentolamine in 5 mL solution) induced erection. Same measures were taken at postoperative week 6 and month 6. All measurement data with normal distribution were recorded as mean ± standard deviation (SD). The results were analyzed using paired two tailed tests for paired comparisons, whereby P<0.05 was considered statistically significant.
Results
The median patient age was 69 [66–73] years old. 82.3% of the patients have hypertension, 41.9% of the patients have diabetes, and 14.5% of the patients had radical prostatectomy while 8% of the patients had external beam radiation therapy for prostate cancer before the penile prosthetic surgery. Amperage from glans biothesiometer readings showed statistically significant shorter readings than elbow biothesiometer preoperatively, 6 weeks and 6 months after surgery (15.60±1.37, 14.52±0.49, and 15.16±0.91, respectively for glans biothesiometer readings, and 19.55±1.21, 22.10±0.48, and 17.68±0.65, respectively for elbow biothesiometer readings, P<0.001 each).
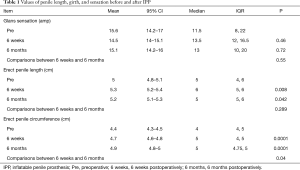
As shown in Table 1, no significant sensory difference in the glans penis after IPP placement was noted. However, compared to preoperative Trimix induced erections, penile length was statistically greater after IPP placement (P=0.01 and P=0.04, respectively). Also, compared to preoperative Trimix induced erections, penile circumference was statistically greater after IPP placement (P=0.0001 and P=0.0001, respectively). Interesting, there was a slight increase in penile circumference at 6 months after surgery as compared to 6 weeks after surgery with statistical difference (P=0.04).
Full table
Discussion
IPP placement, as a treatment for refractory ED, carries a high satisfaction rate for patients and their partners (1,5). However, dissatisfaction is still present with disagreement regarding the length and sensation changes after the IPP placement. It would be of great benefit if both the surgeon and patient were being able to predict the erect penile length prior to IPP surgery. The surgery could be better planned if foreknowledge of the approximate cylinder size to use was known. For patients, estimation of the postoperative erect penile length is beneficial in matching their realistic expectations.
In Wang’s prospective and long-term follow-up comparison of erect penile length obtained with IPP to that induced by intracavernosal injection, penile length was found to be decreased after the IPP placement (10). Their data was based on 11 of 109 patients undergoing penile Doppler ultrasound because these were the only patients to have what they determined to be a “full erections”. However, not included in their study was the time from the penile Doppler exam to IPP placement, which can have a time correlated negative effect on intraoperative penile length. Osterberg et al. (13) also found that 70% of patients who underwent IPP surgery demonstrated a decrease in penile length (median loss 0.5±1.5 cm). Notably, only 43% of patients perceived this loss while some patients reported a subjective increase in size.
In Deveci’s prospective study with 56 patients, 40 (72%) reported a decrease in penile length, 10 (19%) reported no change, and 6 (9%) had a slight increase. Subjective penile length loss was found to be more common in patients who had undergone radical prostatectomy before the IPP surgery (32%). No statistical difference in EF (erectile function) domain scores was noted between patients who complained of penile length loss and those who did not; however, patients who complained of penile length loss had lower IIEF (The International Index of Erectile Function) satisfaction domain and EDITS (Erectile Dysfunction Inventory of Treatment Satisfaction Index) scores (9).
In Henry’s prospective, three-center study of 40 patients who underwent IPP placement with one year follow-up (11), patients were instructed to inflate the IPP daily for 6 months and then inflate maximally for 1–2 hours daily for 6–12 months. Penile measurement changes were significantly improved at 12 months as compared with immediately postoperative and at 6 months. Out of all the patients, 64.5% were satisfied with their length at 1 year, and 74.2% had perceived penile length that was longer (29%) or the same (45.2%) as compared with prior to the surgery; 61.3% and 16.1% of the patients had increased and unchanged satisfaction, respectively, with penile length as compared with prior to IPP surgery. All but two subjects (93.4%) were satisfied with the overall function and dimensions of their IPP. In his further study with 2 years’ follow-up (12), measurement changes were improved at 24 months as compared to immediately postoperative, and at 12 months with continued high satisfaction rate.
As described by previous studies (13,21), both preoperative flaccid stretch penile length and pharmacologically induced erection were appropriate measurements to utilize to set patient’s expectations prior to penile prosthetic surgery, even though these two studies were on two different populations from ours. In our study, we observed significant increments in penile length and girth after IPP placement, providing the prosthetic surgeon with several valuable expectations to pass on to patients: (I) penile prosthetic surgery did not decrease penile length in our study; (II) penile prosthetic surgery might be able to stop the process of atrophy the patient may or may not have perceived; (III) penile prosthetic surgery can maintain and actually increase penile girth.
The dorsal nerve of the penis innervates the glans, including the frenulum which is also innervated by a branch of the perineal nerve. Branches of the dorsal nerve of the penis extend through the glans ventrolaterally. Electrical representation of glandular innervation reveals the glans to be filled with nerve endings supporting its function as a sensory structure (22). Prosthetic surgery is not supposed to change the penile sensation since the surgery will not impair the innervations of the glans, as demonstrated in our study. In Sansalone’s study (16), 4 of his 20 subjects complained of diminished glans sensitivity after the IPP placement. However, their study subjects were a group of patients who had Peyronie’s disease, refractory ED, and severe penile shortening undergoing IPP placement when a concomitant penile lengthening with circumferential graft was performed.
There are several limitations of this study. One concentration of Trimix is unlikely to provide full erections for accurate measurement for every patient. Also, the follow-up of our study was relatively short which might not reflect the final changes of parameters from the surgery. Future study to obtain greater case number to investigate potential association of co-morbidities and prostate cancer treatment with postoperative changes on the penile length, girth, and sensation changes could be very valuable.
Conclusions
We observed statistically significant increase in penile length and girth after IPP placement without significant changes in sensory conduction.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics review board of Urological Research Network (URN 2012-04).
References
- Ji YS, Ko YH, Song PH, et al. Long-term survival and patient satisfaction with inflatable penile prosthesis for the treatment of erectile dysfunction. Korean J Urol 2015;56:461-5. [Crossref] [PubMed]
- Falcone M, Rolle L, Ceruti C, et al. Prospective analysis of the surgical outcomes and patients' satisfaction rate after the AMS Spectra penile prosthesis implantation. Urology 2013;82:373-6. [Crossref] [PubMed]
- Chung E, Solomon M, DeYoung L, et al. Clinical outcomes and patient satisfaction rates among elderly male aged ≥75 years with inflatable penile prosthesis implant for medically refractory erectile dysfunction. World J Urol 2014;32:173-7. [Crossref] [PubMed]
- Menard J, Tremeaux JC, Faix A, et al. Erectile function and sexual satisfaction before and after penile prosthesis implantation in radical prostatectomy patients: a comparison with patients with vasculogenic erectile dysfunction. J Sex Med 2011;8:3479-86. [Crossref] [PubMed]
- Otero JR, Cruz CR, Gómez BG, et al. Comparison of the patient and partner satisfaction with 700CX and Titan penile prostheses. Asian J Androl 2017;19:321-5. [Crossref] [PubMed]
- Levine LA, Becher E, Bella A, et al. Penile Prosthesis Surgery: Current Recommendations From the International Consultation on Sexual Medicine. J Sex Med 2016;13:489-518. [Crossref] [PubMed]
- Munding MD, Wessells HB, Dalkin BL. Pilot study of changes in stretched penile length 3 months after radical retropubic prostatectomy. Urology 2001;58:567-9. [Crossref] [PubMed]
- Savoie M, Kim SS, Soloway MS. A prospective study measuring penile length in men treated with radical prostatectomy for prostate cancer. J Urol 2003;169:1462-4. [Crossref] [PubMed]
- Deveci S, Martin D, Parker M, et al. Penile length alterations following penile prosthesis surgery. Eur Urol 2007;51:1128-31. [Crossref] [PubMed]
- Wang R, Howard GE, Hoang A, et al. Prospective and long-term evaluation of erect penile length obtained with inflatable penile prosthesis to that induced by intracavernosal injection. Asian J Androl 2009;11:411-5. [Crossref] [PubMed]
- Henry GD, Carrion R, Jennermann C, et al. Prospective evaluation of postoperative penile rehabilitation: penile length/girth maintenance 1 year following Coloplast Titan inflatable penile prosthesis. J Sex Med 2015;12:1298-304. [Crossref] [PubMed]
- Pryor MB, Carrion R, Wang R, et al. Patient satisfaction and penile morphology changes with postoperative penile rehabilitation 2 years after Coloplast Titan prosthesis. Asian J Androl 2016;18:754-8. [Crossref] [PubMed]
- Osterberg EC, Maganty A, Ramasamy R, et al. Pharmacologically induced erect penile length and stretched penile length are both good predictors of post-inflatable prosthesis penile length. Int J Impot Res 2014;26:128-31. [Crossref] [PubMed]
- Negro CL, Paradiso M, Rocca A, et al. Implantation of AMS 700 LGX penile prosthesis preserves penile length without the need for penile lengthening procedures. Asian J Androl 2016;18:114-7. [Crossref] [PubMed]
- Henry G, Houghton L, Culkin D, et al. Comparison of a new length measurement technique for inflatable penile prosthesis implantation to standard techniques: outcomes and patient satisfaction. J Sex Med 2011;8:2640-6. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie's disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316-21. [Crossref] [PubMed]
- Miranda-Sousa A, Keating M, Moreira S, et al. Concomitant ventral phalloplasty during penile implant surgery: a novel procedure that optimizes patient satisfaction and their perception of phallic length after penile implant surgery. J Sex Med 2007;4:1494-9. [Crossref] [PubMed]
- Borges F, Hakim L, Kline C. Surgical technique to maintain penile length after insertion of an inflatable penile prosthesis via infrapubic approach. J Sex Med 2006;3:550-3. [Crossref] [PubMed]
- Montague DK, Angermeier KW. Cylinder sizing: less is more. Int J Impot Res 2003;15 Suppl 5:S132-3. [Crossref] [PubMed]
- Breda G, Xausa D, Giunta A, et al. Nomogram for penile biothesiometry. Eur Urol 1991;20:67-9. [PubMed]
- Chen J, Gefen A, Greenstein A, et al. Predicting penile size during erection. Int J Impot Res 2000;12:328-33. [Crossref] [PubMed]
- Yang CC, Bradley WE. Innervation of the humanglans penis. J Urol 1999;161:97-102. [Crossref] [PubMed]



