Erectile dysfunction therapy in countries where implant is economically not feasible
Introduction
Erectile dysfunction (ED), a common complaint of male sexual medicine, is defined as the inability to attain and/or maintain an adequate penile erection for successful sexual intercourse (1). It is estimated, that by 2025 the worldwide prevalence of ED will be of approximately 322 million patients, with the largest projected increase being in the developing world (2). ED is classified as psychogenic and/or organic, the latter being responsible for over 80% of cases and it is divided into endocrine and non-endocrine etiologies (3). Age is the most important risk factor for ED. Data from two key epidemiological studies report a prevalence of mild to moderate ED in 30–52% of men aged 40–79 years (4,5). There is a clear association between vasculogenic ED, the leading cause of this disease, and other cardiovascular risk factors. Recent data has linked ED with endothelial dysfunction and cardiovascular disease (CVD); additionally, an Asian study even proposed that it should be considered a surrogate marker for coronary artery disease (CAD) in young patients (6).
The most important risk factors reported in a European cross-sectional study of 2,869 consecutive men were age (>50 years, OR 1.7–3.32), physical activity (OR 1.35), psychological stress (OR 1.68), hypertension (OR 2.05), diabetes mellitus (DM) (OR 3.0), hyperlipidemia (OR 2.29) and lower urinary tract symptoms (OR 2.2) (7). Social (partner availability) and psychogenic factors appear to play an important role in ED in younger patients (<40 years of age) (8).
The aim of this review is to discuss the non-surgical management of ED with a focus on risk factor assessment and lifestyle modification.
Obesity
Obesity is a major global public health concern with colossal economic implications. It is estimated that at least 1 billion people worldwide are overweight or obese and current epidemiological trends indicate that the prevalence of this disease is increasing at an alarming rate in Latin American countries (9,10). In 2010, 68% of the Mexican male population was estimated to be overweight or obese and this rate is expected to increase to 88% by 2050 (11). Obesity is associated with arteriosclerosis and endothelial dysfunction as well as elevated cholesterol and a pro-inflammatory state which results in a decrease in the availability and activity of nitric oxide (NO) (12,13). Furthermore, obesity is also associated with reduced circulating testosterone levels and the metabolic syndrome (insulin resistance and endothelial dysfunction) leading to an increased prevalence of ED in this population (13). Data from prospective observational studies report that overweight to obese individuals have an increased risk of ED (OR 1.4–2.46) (13). A cross-sectional study of 256 consecutive patients with ED in Brazil demonstrated that central obesity was associated with the presence of ED in men older than 60 years. The presence of any of the following commonly used anthropometric indicators was independently associated with the presence of ED: waist-hip index >0.91 (OR 8.56, 95% CI: 1.44–50.73) and waist circumference >102 cm (OR 19.37, 95% CI: 1.15–326.55) (14).
DM
DM, mainly type 2 DM, is a systemic disease associated with a wide array of chronic micro and macrovascular complications that generate a major economic burden. The global prevalence of diabetes is increasing and the total number of people with diabetes worldwide is projected to rise from 171 million in the year 2000 to 366 million in 2030 (15). The estimated prevalence in Latin American countries is expected to increase by 56% (over 32 million individuals) (15). Genitourinary complaints, primarily ED, are common, have an earlier onset and are more severe in this population (16). These are mainly related to chronic vasculopathy or neuropathy. However, hypogonadism is more common in diabetics and it may also contribute to ED by several mechanisms, such as decreased libido, fatigue, mood swings, decreased body and bone mass (17). Men with DM are 3 times more likely to report ED than non-diabetics with a reported prevalence that ranges from 25–75% (18,19). In addition, men with type 1 DM (RR =3, 95% CI: 1.5–5.9) have a significantly higher risk than men with type 2 DM (RR =1.3, 95% CI: 1.1–1.5) and non-diabetic men (18). Moreover, disease onset also occurs up to 15 years earlier compared with non-diabetic subjects (20).
Risk factors for ED in men with diabetes include: age (>50 years), smoking, younger age at diagnosis, poor glycemic control, drug use (antihypertensives and/or hormones), and the presence of late complications (neuropathy and vasculopathy) (19). There is also increased risk of ED with regard to the pharmacological treatment of diabetes: oral hypoglycemic agents (OR 2.14, 95% CI: 1.87–2.46), insulin use (OR 3.07, 95% CI: 3.13–4.40) and both oral hypoglycemic agents and insulin (OR 4.14, 95% CI: 3.42–5.02) (19).
CVD, hypertension and smoking
A strong association between ED and CVD has been well established in epidemiological studies. It has similar predictive value than traditional CVD risk factors, including family history and is now considered an independent marker for overall coronary heart disease (RR 1.46, 95% CI: 1.31–1.63, P<0.001), stroke (RR 1.35, 95% CI: 1.19–1.54, P<0.001) and all-cause mortality (RR 1.19, 95% CI: 1.05–1.34, P=0.005) (21). This association naturally occurs because these two conditions share common cardiovascular risk factors and essentially the same pathophysiology. The lifetime risk of atherosclerotic CVD in men over 50 years of age is greater than 50% (22). ED has been identified as a sentinel symptom of men with subclinical or occult vascular disease and this can be explained by the “artery size” hypothesis; the smaller penile atherosclerotic arteries (1–2 mm diameter) are obstructed earlier than the larger coronary arteries (3–4 mm diameter) (23). For this reason, ED is now considered a harbinger of CAD; the time interval between the onset of ED and the occurrence of symptomatic CAD or a CVD event is 2–3 years and 3–5 years, respectively (24). An estimated 1.5 billion people are expected to suffer from hypertension worldwide and ED is twice as common in hypertensive patients compared to normal subjects (25). The prevalence of this disorder has increased to 30% in Mexico and it is responsible for 14% ($1.8 billion) of the countries total annual healthcare expenditure (26). Antihypertensive therapy (mainly thiazide diuretics, aldosterone antagonists and β-blockers) is also associated with this disorder and a detailed medical history should rule them out. Angiotensin receptor blockers (ARBs) potentially enhance erectile function and are considered first line treatment in men with hypertension and concomitant ED (25). PDE-5 inhibitors are safe and effective in these patients even with simultaneous multidrug antihypertensive therapy. However they are contraindicated in patients treated with short or long acting nitrates and caution is advised with simultaneous alpha-blocking agents (orthostatic hypertension) (27).
Smoking
Cigarette smoking is the leading preventable cause of mortality in the world causing an estimated 6 million deaths per year. The global number of smokers is expected to increase by 10% to 872 million by 2030 and data from the WHO suggest that nearly 80% of active smokers live in low and middle-income countries (28). It is considered an independent risk factor for atherosclerosis and CVD and it has been linked with ED in large epidemiological studies (4,5,29). Pooled data from a meta-analysis of 3819 impotent men revealed that impotent men were more likely to be smokers than men in the general population (40% vs. 28%, P<0.05) (30). An Italian cross sectional study of 2010 men observed that current smokers (OR 1.7, 95% CI: 1.2–2.4) and ex-smokers (OR 1.6, 95% CI: 1.1–2.3) were more likely to have ED than non smokers and that this association was present even without a history of other CVDs (31). Condra et al. observed that mean penile blood pressure was abnormally low among smokers (20.9%) when compared with non-smokers (8.8%) and suggested that cigarette smoking was a significant risk factor for ED (32). Furthermore, this habit appears to amplify the risk in patients with other cardiovascular disorders. This risk has also been found to be dose-dependent and that among ex-smokers the risk decreases with increasing number of years of tobacco cessation (33). Smoking affects sexual function by multiple mechanisms: centrally (by neuroregulatory effects in the CNS) (34), peripherally (chronic sympathetic activation and heart rate variability) (35) and biochemically (by impairment of NO synthesis and endothelium dependent smooth muscle relaxation) (36).
Management
ED is now considered an early clinical sign of a systemic CVD in young men. As such, the attending clinician must adopt a holistic approach in the treatment of these patients. Management should include an adequate treatment of non-modifiable risk factors (mainly, hypertension, dyslipidemia and diabetes) and the adoption of a healthy lifestyle (smoking cessation, weight loss, physical activity, and an appropriate diet). A large prospective study of risk factors for ED that included 22,086 subjects in the United States during a 14 year follow-up found that obesity (RR 1.9, 95% CI: 1.6–2.2) and smoking (RR 1.5, 95% CI: 1.3–1.7) were associated with increased risk of ED while physical activity (RR 0.7, 95% CI: 0.7–0.8) had a protective effect (37). Gupta et al. demonstrated that lifestyle modification and an adequate treatment of cardiovascular risk factors was associate with improvement in sexual function (measured by IIEF-5 scores): weighted mean difference, 2.66 (95% CI: 1.86–3.47) (38). A European cross sectional study of 1000 men with cardiovascular risk factors found that a high education level (OR 0.52; 95%, CI: 0.33–0.83, P=0.001), high-intensity physical activity (OR 0.50; 95% CI: 0.29–0.86, P=0.045) and a stable relationship (OR 0.43; 95% CI: 0.21–0.88, P=0.046) were associated with decreased risk of ED (39). Evidence may be contradictory in some aspects, for example: data analyzing modifiable risk factors and lifestyle changes from the MMAS longitudinal study after 8 years follow up in middle-aged men observed that: changes in obesity, smoking status or heavy drinking were not associated with ED risk and that men who initiated physical activity (adjusted OR 0.3) had decreased risk of ED (40). An Italian randomized, single-blind clinical trial of 110 obese men revealed that lifestyle changes (reducing caloric intake and increasing level of physical activity) was associated with improvement in sexual function (41). Weight loss appears to be a safe and effective method that mitigates the inflammatory response and improves endothelial function (42).
Asymptomatic men with a recent ED diagnosis require a cardiovascular risk assessment. The ACCF/AHA 2010 guidelines recommend the Framingham Risk Score (see http://www.cvriskcalculator.com) as an adequate tool for global cardiovascular risk assessment because it is highly predictive of cardiovascular events in men ≥40 years of age (43). This instrument considers the “classic” cardiovascular risk factors like: age, sex, race, total cholesterol, HDL, systolic and diastolic blood pressure, anti-hypertensive medicine use, the presence of diabetes and smoking status, and calculates the 10 year risk for a cardiovascular event (heart disease or stroke). Based on this assessment, early referral for a full cardiologic work-up is warranted in men with significant risk factors (21).
Smoking cessation
Smoking cessation is an imperative public health goal that prevents most excess cardiovascular mortality. Mortality risk is reduced by 50% if patients quit by the age of 50 and is avoided almost as a whole if they quit by the age of 30 (29). Diverse public health strategies (i.e., smoke-free environment, tobacco prices, taxes, policy and legislation) are being adopted worldwide along in order to achieve the WHO goal of a 25% reduction in the risk of deaths due to non-communicable diseases by 2025 (44). Multiple interventions in the primary care setting have also proven to be effective, such as: cognitive behavioral therapy, implementation of intensive smoking cessation centers and pharmacotherapy. First-line drugs recommended for smoking cessation include: nicotine replacement therapy, bupropion and varenicline (45). A randomized clinical trial of 697 patients compared gradual vs. abrupt smoking cessation and found that abrupt cessation was more likely to lead to long lasting abstinence (46). The effect of smoking cessation on erectile function has not been prospectively addressed and data from retrospective epidemiological studies is contradictory; however, we may infer from the available evidence that this intervention may reverse or at least halt disease progression (36). A multi-disciplinary approach in the primary care setting should be used to encourage patients to quit smoking.
Dietary patterns and the Mediterranean diet
A strong association between dietary patterns, endothelial and erectile has been established in observational studies. A high flavonoid diet intake has been linked to a reduced ED incidence in a recent prospective study of 25,096 men with 10 years follow up (47). The “Mediterranean diet” is among the healthiest of diets and it consists in a high intake of foods of vegetable origin (cereals, fruits, vegetables, legumes, nuts), olive oil as the main source of fat, a moderate consumption of alcohol (1–2 glasses of red wine per day) and a low consumption of meat (except fish) and dairy products. It is now considered more than a dietary pattern because it promotes the adoption physical activity and a healthy lifestyle (48). This diet appears to have a protective effect against type 2 DM and obesity because it prevents weight gain, insulin resistance and pancreatic beta cell dysfunction (49). Moreover, a randomized clinical study of 180 subjects demonstrated that a Mediterranean style diet was associated with improved endothelial function and a significantly reduced serum concentrations of high-sensitivity C-reactive protein (P=0.01), interleukin 6 (P=0.04) and decreased insulin resistance (P<0.001) in patients with the metabolic syndrome after two years follow up (50). It appears that close adherence to a Mediterranean diet improves endothelial function even in the short term (2 months) in patients with abdominal obesity (51). Based on this data, it is reasonable to assume that this dietary pattern has beneficial effects in erectile function. Evidence suggests that this diet ameliorates or even restores erectile function in men with obesity or the metabolic syndrome (52). This link was further demonstrated in an Italian study where the Mediterranean diet was found effective in reducing the prevalence of ED in men with the metabolic syndrome after two years follow up (53). This dietary pattern also appears to reduce systemic inflammation and improve sexual function in women with the metabolic syndrome (54).
Conclusions
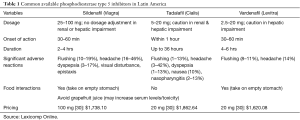
The management of patients with ED in low and middle-income countries is increasingly challenging. There is a high incidence of non-compliance to lifestyle modification habits and pharmacological treatment adherence of concomitant diseases. Moreover, widespread use of available phosphodiesterase type 5 inhibitors is limited in some areas due to high costs (see Table 1). Lack of efficacy from non-pharmacological and pharmacological interventions is also common and this is in part due to inadequate treatment of shared cardiovascular risk factors such as, obesity and advanced type 2 DM. This was illustrated in a prospective study of 511 PDE5 inhibitor naive Latin American men observed that two thirds of the patients were persistent and adherent to pharmacologic therapy after 6 months of follow up and that the main reasons for non persistence included medication cost and lack of efficacy (55). Surgical management of this disorder is not widely available in Latin America because it is not economically feasible in most countries. For this reason, patient management of ED in these countries must include non-pharmacological preventive measures, such as lifestyle modification including smoking cessation and an adequate treatment of concomitant CVDs.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA 1993;270:83-90. [Crossref] [PubMed]
- Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999;84:50-6. [Crossref] [PubMed]
- Yafi FA, Jenkins L, Albersen M, et al. Erectile dysfunction. Nat Rev Dis Prim 2016;2:16004. [PubMed]
- Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994;151:54-61. [PubMed]
- Corona G, Lee DM, Forti G, et al. Age-related changes in general and sexual health in middle-aged and older men: Results from the European Male Ageing Study (EMAS). J Sex Med 2010;7:1362-80. [Crossref] [PubMed]
- Dattatrya KY, Vedpalsingh TH, Gorakhnath WV, et al. Can Erectile Dysfunction in Young Patients Serve as a Surrogate Marker for Coronary Artery Disease? J Clin Diagn Res 2015;9:PC01-3. [PubMed]
- Ponholzer A, Temml C, Mock K, et al. Prevalence and risk factors for erectile dysfunction in 2869 men using a validated questionnaire. Eur Urol 2005;47:80-5; discussion 85-6. [Crossref] [PubMed]
- Villeda-Sandoval CI, Calao-Pérez MB, Herrera-Cáceres JO, et al. Erectile dysfunction and associated risk factors among young Mexican adults: The importance of partner availability. Rev Mex Urol 2015;75:260-5.
- Ford ES, Mokdad AH. Epidemiology of Obesity in the Western Hemisphere. J Clin Endocrinol Metab 2008;93:S1-8. [Crossref] [PubMed]
- Filozof C, Gonzalez C, Sereday M, et al. Obesity prevalence and trends in Latin-American countries. Obes Rev 2001;2:99-106. [Crossref] [PubMed]
- Rtveladze K, Marsh T, Barquera S, et al. Obesity prevalence in Mexico: impact on health and economic burden. Public Health Nutr 2014;17:233-9. [Crossref] [PubMed]
- Seifalian AM, Filippatos TD, Joshi J, et al. Obesity and arterial compliance alterations. Curr Vasc Pharmacol 2010;8:155-68. [Crossref] [PubMed]
- Esposito K, Giugliano D. Obesity, the metabolic syndrome, and sexual dysfunction in men. Clin Pharmacol Ther 2011;90:169-73. [Crossref] [PubMed]
- Riedner CE, Rhoden EL, Ribeiro EP, et al. Central obesity is an independent predictor of erectile dysfunction in older men. J Urol 2006;176:1519-23. [Crossref] [PubMed]
- Wild S, Roglic G, Green A, et al. Global Prevalence of Diabetes: Estimates for the year 2000 and projection for 2030. Diabetes Care 2004;27:1047-53. [Crossref] [PubMed]
- Goldstraw MA, Kirby MG, Bhardwa J, et al. Diabetes and the urologist: A growing problem. BJU Int 2007;99:513-7. [Crossref] [PubMed]
- Hijazi RA, Betancourt-Albrecht M, Cunningham GR. Gonadal and erectile dysfunction in diabetics. Med Clin N Am 2004;88:933-45. [Crossref] [PubMed]
- Bacon CG, Hu FB, Giovannucci E, et al. Association of Type and Duration of Diabetes With Erectile Dysfunction in a large cohort of men. Diabetes Care 2002;25:1458-63. [Crossref] [PubMed]
- Fedele D. Therapy Insight: sexual and bladder dysfunction associated with diabetes mellitus. Nat Clin Pract Urol 2005;2:282-90. [Crossref] [PubMed]
- Luthra A, Misra A. Erectile dysfunction in diabetic males: Plausible mechanisms and management strategies. Diabetes Metab Syndr Clin Res Rev 2008;2:81-6. [Crossref]
- Nehra A, Jackson G, Miner M, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc 2012;87:766-78. [Crossref] [PubMed]
- Nehra A, Jackson G, Miner M, et al. Diagnosis and treatment of erectile dysfunction for reduction of cardiovascular risk. J Urol 2013;189:2031-8. [Crossref] [PubMed]
- Montorsi P, Ravagnani PM, Galli S, et al. The artery size hypothesis: A macrovascular link between erectile dysfunction and coronary artery disease. Am J Cardiol 2005;96:19M-23M. [Crossref] [PubMed]
- Jackson G, Boon N, Eardley I, et al. Erectile dysfunction and coronary artery disease prediction: Evidence-based guidance and consensus. Int J Clin Pract 2010;64:848-57. [Crossref] [PubMed]
- Viigimaa M, Vlachopoulos C, Lazaridis A, et al. Management of erectile dysfunction in hypertension: Tips and tricks. World J Cardiol 2014;6:908-15. [Crossref] [PubMed]
- Garcia-Garcia G, Aviles-Gomez R, Luquin-Arellano VH, et al. Cardiovascular Risk Factors in the Mexican Population. Ren Fail 2006;28:677-87. [Crossref] [PubMed]
- Viigimaa M, Doumas M, Vlachopoulos C, et al. Hypertension and sexual dysfunction: time to act. J Hypertens 2011;29:403-7. [Crossref] [PubMed]
- Méndez D, Alshanqeety O, Warner KE. The potential impact of smoking control policies on future global smoking trends. Tob Control 2013;22:46-51. [Crossref] [PubMed]
- Herrington W, Lacey B, Sherliker P, et al. Epidemiology of Atherosclerosis and the Potential to Reduce the Global Burden of Atherothrombotic Disease. Circ Res 2016;118:535-46. [Crossref] [PubMed]
- Tengs TO, Osgood ND. The link between smoking and impotence: two decades of evidence. Prev Med 2001;32:447-52. [Crossref] [PubMed]
- Mirone V, Imbimbo C, Bortolotti A, et al. Cigarette smoking as risk factor for erectile dysfunction: Results from an Italian epidemiological study. Eur Urol 2002;41:294-7. [Crossref] [PubMed]
- Condra M, Morales A, Owen JA, et al. Prevalence and significance of tobacco smoking in impotence. Urology 1986;27:495-8. [Crossref] [PubMed]
- Bortolotti A, Fedele D, Chatenoud L, et al. Cigarette smoking: A risk factor for erectile dysfunction in diabetics. Eur Urol 2001;40:392-6; discussion 397. [Crossref] [PubMed]
- Pomerleau OF. Nicotine and the central nervous system: Biobehavioral effects of cigarette smoking. Am J Med 1992;93:2S-7S. [Crossref] [PubMed]
- Harte CB, Meston CM. Association between Cigarette Smoking and Erectile Tumescence: The Mediating Role of Heart Rate Variability. Int J Impot Res 2013;25:155-9. [Crossref] [PubMed]
- McVary KT, Carrier S, Wessells H. Smoking and Erectile Dysfunction: Evidence Based Analysis. J Urol 2001;166:1624-32. [Crossref] [PubMed]
- Bacon CG, Mittleman MA, Kawachi I, et al. A Prospective Study of Risk Factors for Erectile Dysfunction. J Urol 2006;176:217-21. [Crossref] [PubMed]
- Gupta BP, Murad MH, Clifton MM, et al. The Effect of Lifestyle Modification and Cardiovascular Risk Factor Reduction on Erectile Dysfunction: A Systematic Review and Meta-analysis. Arch Intern Med 2011;171:1797-803. [Crossref] [PubMed]
- Ettala OO, Syvänen KT, Korhonen PE, et al. High-Intensity Physical Activity, Stable Relationship, and High Education Level Associate with Decreasing Risk of Erectile Dysfunction in 1,000 Apparently Healthy Cardiovascular Risk Subjects. J Sex Med 2014;11:2277-84. [Crossref] [PubMed]
- Derby CA, Mohr BA, Goldstein I, et al. Modifiable Risk Factors and Erectile Dysfunction: Can Lifestyle Changes Modify Risk? Urology 2000;56:302-6. [Crossref] [PubMed]
- Esposito K, Giuglano F, Di Palo C, et al. Effect of Lifestyle Changes on Erectile Dysfunction in Obese Men. JAMA 2004;291:2978-84. [Crossref] [PubMed]
- Ziccardi P, Nappo F, Giugliano G, et al. Reduction of inflammatory cytokine concentrations and improvement of endothelial functions in obese women after weight loss over one year. Circulation 2002;105:804-9. [Crossref] [PubMed]
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2010;56:e50-103. [Crossref] [PubMed]
- Carroll AJ, Labarthe DR, Huffman MD, et al. Global tobacco prevention and control in relation to a cardiovascular health promotion and disease prevention framework: A narrative review. Prev Med 2016;93:189-97. [Crossref] [PubMed]
- Shaik SS, Doshi D, Bandari SR, et al. Tobacco use cessation and prevention – A review. J Clin Diagn Res 2016;10:ZE13-7. [PubMed]
- Lindson-Hawley N, Banting M, West R, et al. Gradual versus abrupt smoking cessation a randomized, controlled noninferiority trial. Ann Intern Med 2016;164:585-92. [Crossref] [PubMed]
- Cassidy A, Franz M, Rimm EB. Dietary flavonoid intake and incidence of erectile dysfunction. Am J Clin Nutr 2016;103:534-41. [Crossref] [PubMed]
- Bach-Faig A, Berry EM, Lairon D, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr 2011;14:2274-84. [Crossref] [PubMed]
- Schröder H. Protective mechanisms of the Mediterranean diet in obesity and type 2 diabetes. J Nutr Biochem 2007;18:149-60. [Crossref] [PubMed]
- Esposito K, Marfella R, Ciotola M. Effect of a Mediterranean-Style Diet on Endothelial Dysfunction and Markers of Vascular Inflammation in the Metabolic Syndrome: A Randomized Trial. JAMA 2004;292:1440-6. [Crossref] [PubMed]
- Rallidis LS, Lekakis J, Kolomvotsou A, et al. Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am J Clin Nutr 2009;90:263-8. [Crossref] [PubMed]
- Esposito K, Giugliano F, Maiorino MI, et al. Dietary Factors, Mediterranean Diet and Erectile Dysfunction. J Sex Med 2010;7:2338-45. [Crossref] [PubMed]
- Esposito K, Ciotola M, Giugliano F, et al. Mediterranean diet improves erectile function in subjects with the metabolic syndrome. Int J Impot Res 2006;18:405-10. [Crossref] [PubMed]
- Esposito K, Ciotola M, Giugliano F, et al. Mediterranean diet improves sexual function in women with the metabolic syndrome. Int J Impot Res 2007;19:486-91. [Crossref] [PubMed]
- Rubio-Aurioles E, Reyes L, Borregales L, et al. A 6-month, prospective, observational study of PDE5 inhibitor treatment persistence and adherence in Middle Eastern and North African men with erectile dysfunction. Curr Med Res Opin 2013;29:695-706. [Crossref] [PubMed]


