Does the number of veins ligated during microsurgical subinguinal varicocelectomy impact improvement in pain post-surgery?
Introduction
Varicocele is clinically defined as a distended and tortuous testicular pampiniform plexus of veins in the spermatic cord. Varicocele is present in up to 20% of the general adult male population, and is more prevalent in men with primary (40%) or secondary infertility (80%) (1). This clinical condition is mostly asymptomatic but can present with persistent scrotal pain in about 10% of cases (2). The pain is typically dull aching or dragging in character, aggravated by prolonged standing or by physical activity and relieved by rest or lying down (3,4). Chronic scrotal pain can be a nuisance for its sufferer affecting his daily activities on so many levels (5).
Conservative measures including anti-inflammatory medicines, scrotal support, and restriction of physical activity are usually first line therapies in patients with symptomatic varicocele (4,6). When such measures fail, and only when other etiologies have been ruled out, varicocelectomy is indicated (7). However, surgery may not result in pain resolution, even with documented absence of recurrence postoperatively (6). Generally, up to 20% of patients undergoing varicocelectomy may experience partial or no improvement in their symptoms after surgery (8). In attempt to improve the surgical outcome, several factors have been investigated in the literature to predict success in pain relief after surgery. These included varicocele grade (8-13), pain quality and intensity (8,10-13), duration of pain (8,10-13), varicocele recurrence (11,12,14), external spermatic vein ligation (5,15), method of varicocele ligation (11,15-17), body mass index (8,10,12), and semen quality, pH and volume (10). While the extent of intraoperative vein ligation was sparsely evaluated in terms of its influence on semen parameter results postoperatively, this study is the first of its kind to explore the influence of the number of veins ligated during microsurgical subinguinal varicocelectomy on pain relief.
Methods
This is a retrospective study conducted at the male infertility unit at Hamad Medical Corporation, a teaching hospital in Qatar. Between November 2008 and June 2014, the medical records of 675 patients (mean age =35.3±9.2) who underwent microsurgical subinguinal varicocelectomy were reviewed. Diagnosis and grading of varicocele was conducted clinically by experienced male infertility specialists and according to the Dubin-Amelar criteria (18). Patients who underwent left microsurgical subinguinal varicocelectomy for pain were included in the study, while patients were excluded when surgery was done for another indication or for a recurrent varicocele. Moreover, patients known to have a history of painful scrotal conditions such as orchitis/epididymitis or spermatocele, history of genitourinary surgery such as vasectomy, orchiopexy or hydrocelectomy and history of medical treatment for infertility were also excluded. Two hundred and seven patients out of the 675 patients performed varicocelectomy for pain as the only indication. One hundred and one patients didn’t have a complete pre- and post-operative pain assessment. The final data set included only 106 patients.
The following demographic and clinical data were collected: age, varicocele grade, indication of varicocelectomy (pain/other), type of varicocelectomy and duration/quality of pain. Patients were categorized into three groups according to the number of spermatic veins ligated during varicocelectomy (<5 veins, 5–10 veins and >10 veins). The variables which were tested pre- and post-surgery included pain, semen data and hormonal assay. A waiver of signed informed consent was obtained and the study design was approved by our institute’s local ethics committee (approval number 11252/11). Study procedures were performed according to the Declaration of Helsinki.
Pain assessment
The presence of pain was assessed subjectively at pre- and post-operative surgery (at 3 and 6 months). Data regarding pain were extracted from medical records which contain information about laterality, type, degree and duration of pain as well as aggravating factors.
Microsurgical varicocelectomy
Microsurgical subinguinal varicocelectomy was performed in all patients by the same team. After signing an appropriate surgical consent, patients received 2 g of cefazolin intravenously on induction. All surgeries were performed under general anesthesia. Patients were placed in supine position and were properly draped. A 2 to 3 cm subinguinal incision was then performed and followed by delivery of the spermatic cord that was held using ring forceps. The cord was inspected and all dilated external spermatic veins were ligated. After opening the external spermatic fascia, the surgical microscope (Zeiss®, Carl Zeiss Meditec Inc., California, USA) was utilized. Under 18× magnifications, the internal spermatic veins were carefully dissected, ligated using titanium clips (Premium Surgiclip™, Covidien, Minnesota, USA) and cut. All identified lymphatics were spared. The vas deference was identified during surgery and left intact in its sheath together with vasal vessels. Arterial flow was checked using Doppler at the beginning of surgery and at the end. After achieving hemostasis, closure in two layers using Polyglactin absorbable sutures (Ethicon, USA) was done.
Semen and sperm DNA fragmentation analysis
Semen samples were collected by masturbation following 3–5 days abstinence from intercourse. The sample was left to liquefy after which analysis of the semen samples was conducted according to WHO 2010 protocols for semen examination and processing (19). SDF was measured using Halosperm G2 Test kit. This kit determines the degree of DNA damage of a human sperm through a process called sperm chromatin dispersion (SCD), which is responsible for male infertility. This process “involves the denaturation and controlled lysis of the sample in an appropriate medium and can be used with both fresh and frozen samples. Sperm with intact DNA produce a dispersion halo as a result of the chromatin released from proteins that can be easily analyzed using fluorescence or bright field microscopy. In contrast, sperm with fragmented DNA will not produce this halo. The technique is as easy as a routine leukocyte count (20). SDF level cut off taken as high was SDF ≥30% using Fernandez protocol (21).
Hormonal assay
Hormonal profile was recorded including FSH (n=1–19 IU/L), LH (n=1–9 IU/L), prolactin (n=73–407 mIU/L), total testosterone (n=10.4–35 nmol/L) and estradiol (n=73–275 pmol/L). Hormonal levels recorded were that of the initial visit to the hospital without any hormonal treatment in the past 3 months.
Statistical analysis
Descriptive statistics were used to summarize all demographic and clinical characteristics of patients. Results are presented as a percentage frequency of patients having the variable tested, except for age which is presented as mean ± standard deviation. An appropriate statistical test was used to assess the relationship of various clinical characteristics with outcome. A paired ‘t’ test was used to compare means of all quantitative variables, while a Kruskal-Wallis test (K) and a chi-square test was used to compare qualitative variables. In all statistical tests, a value of P<0.05 was considered significant. Statistical analysis of collected data was performed using SPSS version 20 (IBM, Armonk, NY, USA).
Results
In 207/675 (30.7%) patients, left microsurgical subinguinal varicocelectomy was performed for pain. Their mean age was 31.2±7.3 years, and the majority of them were non-smokers (61.4%). The average reported duration of pain was 11.2±6.4 months. Pain was assessed in 106/207 (51.2%) patients postoperatively, of whom 89 (84%) reported complete resolution of their symptoms. Analysis of the number of veins ligated intraoperatively revealed that <5, 5–10 and >10 veins were ligated in 20, 65 and 21 patients, respectively. While pain relief was reported in all study groups (<5 veins: 90.0%, 5–10 veins: 81.5%, and >10 veins: 85.7%), no statistically significant influence was detected (Table 1).

Full table
Data regarding semen analysis, sperm DNA fragmentation and hormonal assay are reported in (Table 2).

Full table
Discussion
The effect of varicocele on male infertility is well documented. However, its contribution to chronic orchialgia is still not well defined. In fact, many other scrotal and non-scrotal conditions can present with chronic orchialgia. Scrotal injury, infection, cancer of the testes, epididymitis, hydrocele, inguinal hernia, and nerve entrapment are examples (6,22,23). When conservative measures fail to alleviate a symptomatic varicocele, surgery is often indicated. The fertility outcome of surgery has been assessed by several meta-analyses showing a significant improvement in semen parameters postoperatively and favoring microsurgical approaches over other surgical techniques (16). Microsurgical subinguinal varicocelectomy can be considered as the gold standard approach due to its superior fertility outcome and minimal post-operative morbidity. Nonetheless, such assumption cannot be withdrawn when pain is the studied outcome.
There are only few studies which compared different varicocelectomy methods done for pain resolution (16,17). Soylemez et al. compared two different spermatic vein ligation procedures: microsurgical subinguinal varicocelectomy and laparoscopic varicocelectomy. Following surgery, scrotal pain was assessed at post-operative days 1, 3, and 7 and was significantly reduced in the laparoscopic varicocelectomy group who had an earlier return to normal activity than the microsurgical subinguinal varicocelectomy group (17). Despite their significant results, the study was flawed by the early follow up design. On the other hand, Lv et al. compared postoperative complications between four different surgical ligation methods: laparoscopic varicocelectomy and microscopic subinguinal, inguinal, and retroperitoneal varicocelectomy. They reported a significantly higher success rate for microsurgical subinguinal varicocelectomy in decreasing scrotal pain (P<0.05), as well as reducing scrotal edema and testicular atrophy (16).
Shridharani et al. summarized pain resolution success rate according to microsurgical, non-microsurgical and laparoscopic approaches. The overall surgical success rate for alleviating pain in patients who underwent a microsurgical technique is estimated to be 85% for complete resolution, 6% for partial resolution, and 9% for failure of resolution of pain post-surgery. On the other hand, the mean success rate for the non-microsurgical technique was estimated to be 72% for complete resolution, 18% for partial resolution, and 10% for failure of resolution of pain post-surgery. Finally, the laparoscopic approach resulted in an overall success rate of 81% for complete resolution, 5% for partial resolution, and 14% for of resolution of pain post-surgery (22).
Other predictive factors for surgical success in resolving pain post-surgery have been also investigated. A study by Kim et al. reported a significant association between quality of pain and the success rate post-varicocelectomy. Pain resolution was 100% complete when pain was identified as dull vs. dragging in nature (8). Moreover, Altunoluk et al. found that the success rate was also higher in patient with longer duration of pain before surgery (98.6%) in comparison to patients with less pain duration (17.7%) (13). As such, pain quality and duration were both independent predictors of success in resolving pain post-surgery. Other independent factors such as the grade of varicocele (8,10,12,13), intensity of pain (10,13), recurrence of varicocele (12,14), BMI (8,10,12), sperm quality, semen pH, semen volume, FSH, LH, testosterone, maximum vein diameter, peak retrograde flow on Doppler, distance from renal hilum to center of scrotum, and scrotal temperature (10) were all not significantly associated with pain resolution after surgery. In Table 3, we present a summary of the different predictors assessed for pain improvement in most recent studies.
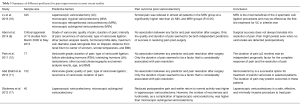
Full table
The effect of the number of veins ligated intraoperatively was never investigated in terms of pain resolution after surgery. Shindel et al. assessed the correlation between the extent of vein ligation during surgery and semen analysis outcomes. They found a significant positive correlation between the number of ligated veins and total sperm motility (P=0.017) (24). The number of veins encountered during surgery is variable among patients and is unrelated to the clinical grade. Newer ultrasound grading systems have incorporated the presence of a venous plexus and the total number of dilated veins in their criteria. Theoretically, the more veins present the more testicular congestion exist and consequently pain. In this study, while a significant improvement in postoperative pain was detected in patients undergoing microsurgical subinguinal varicocelectomy, no significant influence for the number of veins ligated intraoperatively was reported (P=0.81). Therefore, the number of veins ligated was not predictive of post-operative improvement of pain in our study population.
There are few limitations in the present study. The first limitation is that the study is retrospective with incomplete data. Another limitation is that the size of the veins ligated during varicocelectomy was not assessed and recorded which limits the analysis. And the last limitation is that no pain assessment scale was used to assess pain pre- and post-surgery, which may lead to bias in judgment of intensity and quality of pain.
Conclusions
The relationship between number of veins ligated during varicocelectomy and semen analysis outcomes, as well as the relationship between number of veins ligated and pain resolution post-surgery remain unclear. Additional studies about the predictive factors of success for pain relief post-varicocelectomy are still needed to serve better our community.
Acknowledgements
Authors would like to acknowledge Ms. Marwa Adawi for participating in manuscript writing and Mr. Hazim Miqdad for participating in data collection.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: A waiver of signed informed consent was obtained and the study design was approved by our institute’s local ethics committee (approval number 11252/11). All procedures performed in this study involving human participants were in accordance with the ethical standards of the local national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
References
- Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy. A critical analysis. Urol Clin North Am 1994;21:517-29. [PubMed]
- Peterson AC, Lance RS, Ruiz HE. Outcomes of varicocele ligation done for pain. J Urol 1998;159:1565-7. [Crossref] [PubMed]
- Kass EJ, Marcol B. Results of varicocele surgery in adolescents: a comparison of techniques. J Urol 1992;148:694-6. [PubMed]
- Marmar JL, Kim Y. Subinguinal microsurgical varicocelectomy: a technical critique and statistical analysis of semen and pregnancy data. J Urol 1994;152:1127-32. [PubMed]
- Karademir K, Senkul T, Baykal K, et al. Evaluation of the role of varicocelectomy including external spermatic vein ligation in patients with scrotal pain. Int J Urol 2005;12:484-8. [Crossref] [PubMed]
- Abrol N, Panda A, Kekre NS. Painful varicoceles: Role of varicocelectomy. Indian J Urol 2014;30:369-73. [Crossref] [PubMed]
- Schwentner C, Oswald J, Lunacek A, et al. Optimizing the outcome of microsurgical subinguinal varicocelectomy using isosulfan blue: a prospective randomized trial. J Urol 2006;175:1049-52. [Crossref] [PubMed]
- Kim HT, Song PH, Moon KH. Microsurgical ligation for painful varicocele: effectiveness and predictors of pain resolution. Yonsei Med J 2012;53:145-50. [Crossref] [PubMed]
- Yaman O, Ozdiler E, Anafarta K, et al. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology 2000;55:107-8. [Crossref] [PubMed]
- Chen SS. Factors predicting symptomatic relief by varicocelectomy in patients with normospermia and painful varicocele nonresponsive to conservative treatment. Urology 2012;80:585-9. [Crossref] [PubMed]
- Abd Ellatif ME, Asker W, Abbas A, et al. Varicocelectomy to treat pain, and predictors of success: a prospective study. Curr Urol 2012;6:33-6. [Crossref] [PubMed]
- Park HJ, Lee SS, Park NC. Predictors of pain resolution after varicocelectomy for painful varicocele. Asian J Androl 2011;13:754-8. [Crossref] [PubMed]
- Altunoluk B, Soylemez H, Efe E, et al. Duration of preoperative scrotal pain may predict the success of microsurgical varicocelectomy. Int Braz J Urol 2010;36:55-9. [Crossref] [PubMed]
- Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth 2008;101:17-24. [Crossref] [PubMed]
- Chawla A, Kulkarni G, Kamal K, et al. Microsurgical varicocelectomy for recurrent or persistent varicoceles associated with orchalgia. Urology 2005;66:1072-4. [Crossref] [PubMed]
- Lv JX, Wang LL, Wei XD, et al. Comparison of Treatment Outcomes of Different Spermatic Vein Ligation Procedures in Varicocele Treatment. Am J Ther 2016;23:e1329-e1334. [Crossref] [PubMed]
- Söylemez H, Penbegül N, Atar M, et al. Comparison of laparoscopic and microscopic subinguinal varicocelectomy in terms of postoperative scrotal pain. JSLS 2012;16:212-7. [Crossref] [PubMed]
- Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril 1970;21:606-9. [Crossref] [PubMed]
- World Health Organization (WHO). WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th edition. Geneva: WHO Press, 2010.
- Chohan KR, Griffin JT, Lafromboise M, et al. Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl 2006;27:53-9. [Crossref] [PubMed]
- Fernández JL, Muriel L, Goyanes V, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril 2005;84:833-42. [Crossref] [PubMed]
- Shridharani A, Lockwood G, Sandlow J. Varicocelectomy in the treatment of testicular pain: a review. Curr Opin Urol 2012;22:499-506. [Crossref] [PubMed]
- Christiansen CG, Sandlow JI. Testicular pain following vasectomy: a review of postvasectomy pain syndrome. J Androl 2003;24:293-8. [Crossref] [PubMed]
- Shindel AW, Yan Y, Naughton CK. Does the number and size of veins ligated at left-sided microsurgical subinguinal varicocelectomy affect semen analysis outcomes? Urology 2007;69:1176-80. [Crossref] [PubMed]


