Pre-biopsy MRI as an adjunct for cancer detection in men with elevated PSA and no previous biopsy
Introduction
The classical pathway for the diagnosis of prostate cancer (PCa) is an elevated prostate-specific antigen (PSA) and/or a suspicious digital rectal examination (DRE) followed by a trans-rectal ultrasound guided biopsy (TRUS-GB) of the prostate. TRUS is performed mainly for anatomic guidance because ultrasound does not identify clinically significant cancer (CSC) with high accuracy. Biopsies are taken mainly from the peripheral zone, which have the majority of cancers.
Magnetic resonance imaging (MRI) is becoming increasingly used in clinical practice in the diagnostic pathway for prostate cancer. MRI can have different roles in this pathway, by influencing the decision for whether to perform a prostate biopsy, or influencing the chosen biopsy technique. Negative predictive values (NPV) of up to around 95% give MRI the potential to act as a triage test to influence a decision for whether a prostate biopsy is necessary (1,2).
A clinically insignificant prostate cancer is a cancer that is unlikely to progress and would not benefit from treatment. However, when diagnosed with insignificant cancer a large proportion of patients requires treatment in case a more CSC is present. A PCa detection pathway that finds CSC while avoiding the diagnosis of insignificant cancer is the ideal test, and is a situation that the MRI-influenced diagnostic pathway hopes to achieve.
In 2011, a study by Haffner et al. analysed retrospectively the results of targeted biopsy (TB) in naïve patients with suspicious MRI’s compared to 12-core systematic biopsy (SB) in all men independent of MRI result. In this series of 555 patients, MRI was suspicious in 63% (351/555), the overall cancer detection rate (CDR) was 54% (302/555). MRI sensitivity (Se) and specificity (Sp) for cancer detection were 83% and 61%, respectively. Clinically significant cancer was defined as >5 mm total cancer length on 1 or 2 cores and/or any Gleason pattern >3. Results showed that only 2% of CSC would be missed by a targeted-alone biopsy strategy. Only TB strategy without SB would have necessitated an average of 3.8 cores in only 63% of patients. If only targeted biopsy scheme were performed, it would have avoided 13% (53/302) of non-significant cancer and would have missed 2.3% (13/302) of significant cancers (3).
Importantly, it was the first study that showed the amount of cancer that would be missed in a group of men referred with clinical suspicion of prostate cancer if a targeted-alone approach were taken. This retrospective analysis where patient acts as their own control and has both SB and TB will be discussed later (4).
The National Institute for Health Research UK-HTA literature review suggests that the use of MRI first, plus targeted and standard biopsy, versus TRUS-GB schemes without pre-biopsy MRI could be cost-effective. The premise of cost-effectiveness relies on avoiding biopsy in men with non-suspicious MRIs (5). Although those considerations were done with complex statistical analysis projecting cost estimates based on meta-analyses and other data of the literature. These models included patients with previous negative prostate biopsy. Hutchinson et al. also carried out a review of the economic effect of MRI fusion TRUS-GB for prostate cancer diagnosis, concluding that this is an area of intense research looking for relevant evidence (6).
Compared with trans-rectal ultrasound guided biopsy, the MRI targeted biopsy pathway was shown to be a cost-effective strategy when the sensitivity of MRI-TB is >20%. These results suggest total costs of the MRI strategy are similar to the standard of care, while reduction of overdiagnosis and overtreatment with the MRI strategy may lead to an improvement in quality of life (7).
Unfortunately, there is a lack of well design prospective randomized studies comparing cohorts of patients under MRI schemes versus SB, against a reference standard of histopathological assessment of biopsied tissue obtained via saturation biopsy or transperineal template mapping biopsy (TTMB). However, higher quality studies are in progress.
There have been a number of recent developments in multi-parametric MRI, which may improve the generalizability and reliability of MRI in prostate cancer diagnosis. One pertinent example is the development of PIRADS V2 criteria. This publication provided guidelines on image acquisition, interpretation, reporting for clinical practice and data collection for research (8).
What is the accuracy of image-guided prostate biopsy using MRI–derived targets?
Moore et al., based partly on Haffner et al. study methodology and results, published a systematic review in 2013. They found 60–70% of all naïve patients had a suspicious area identified on MRI. When subjected to a targeted biopsy, 66% had prostate cancer detected versus 50% of cancer detected in the same group under SB. Both targeted and standard biopsy detected clinically significant cancer in 43% and 45%, respectively. Conclusion was that MRI-guided biopsy detected clinically significant prostate cancer in an equivalent number of men versus standard biopsy (9). This was achieved using fewer biopsies (2-4) in fewer men (only 70%), with a 10% reduction in the diagnosis of clinically insignificant cancer. Variability in study methodology limited the strength of recommendation that can be made.
Kasivisvanathan et al. demonstrated that there was no statistically significant difference in the detection rate of clinically significant cancer when comparing TB alone and transperineal template guided biopsy (10).
START consortium
An International Working Group published Standards of Reporting for MRI-targeted Biopsy Studies (START) of the Prostate. Following the recommendations according to the START checklist, would improve the quality of reporting and facilitate a comparison between standard biopsy and MRI-targeted approaches (11). Collection of data from studies fulfilling the START criteria may facilitate the evaluation of MRI-TB as a diagnostic strategy for the detection of clinically significant cancer. Since the publication of this topic paper, authors studying MRI-TB use these criteria to present their results. It was helpful subsequently for systematic reviews which have demonstrated good accuracy for the detection of CSC.
Can clinically significant prostate cancer be detected with MRI?
In a systematic review of the literature Fütterer et al. showed that the detection of clinically significant disease using MRI ranged from 44% to 87% in biopsy naïve males and from 35% to 50% in men with prior negative biopsies. They used prostate biopsy or definitive pathology of the radical prostatectomy specimen as reference standard. The NPV for exclusion of significant disease ranged from 63–98% (12). The negative predictive value of MRI is important for clinicians because MRI could be used to rule out significant disease. This may result in fewer biopsies or a delay in performing SB in naïve patients with raised PSA under suspicion of prostate cancer.
Can MRI–TB enhance the diagnostic accuracy of significant prostate cancer detection compared to TRUS-GB?
In a systematic review and meta-analysis, Schoots et al. looked for evidence regarding the diagnostic benefits of MRI-TB versus TRUS-GB in detection of overall PCa and significant/insignificant prostate cancer. The reports included (16 studies) including both MRI-TB and TRUS-GB for prostate cancer detection. A cumulative total of 1,926 men with positive MRI were included, with PCa prevalence of 59%.
MRI-TB and TRUS-GB did not significantly differ in overall prostate cancer detection (sensitivity 85% and 81%, respectively). MRI-TB had a higher rate of detection of significant prostate cancer compared to TRUS-GB (sensitivity 91% vs. 76%) and a lower rate of detection of insignificant prostate cancer (sensitivity 44% vs. 83%). Subgroup analysis revealed an improvement in CSC detection by MRI-TB in men with previous negative biopsy, rather than in men with initial biopsy (relative sensitivity: 1.54; 95% CI: 1.05–2.57 vs. 1.10; 95% CI: 1.00–1.22).
In conclusion, in men with clinical suspicion of prostate cancer and a subsequent positive MRI, MRI-TB and TRUS-GB did not differ in overall prostate cancer detection. However, MRI-TB had a higher rate of detection of significant prostate cancer and a lower rate of detection of insignificant prostate cancer compared with TRUS-GB (13).
Since the publication of these reviews, several key studies have been published and some of them will be discussed below.
Study by Pokorny et al. (14)
In this study, all participants underwent MRI and TRUS-GB. Men with equivocal or suspicious lesions on MRI also underwent MRI-TB. Patients acted as their controls. A total of 223 consecutive biopsy-naive men referred to a urologist with elevated PSA participated in a single-institution, prospective and investigator blinded diagnostic study from July 2012 through January 2013. Of 223 men, 142 (63.7%) had PCa. TRUS-GB detected 126 cases of PCa in 223 men (56.5%) including 47 (37.3%) classed as low risk. MRI-TB detected 99 cases of PCa in 142men (69.7%) with equivocal or suspicious MRI, of which 6 (6.1%) were low risk.
The MRI-TB pathway reduced the need for biopsy by 51%, decreased the diagnosis of low-risk PCa by 89.4%, and increased the detection of intermediate/high-risk PCa by 17.7%. The estimated NPVs of TRUS-GB and MRI-TB for intermediate/high risk disease were 71.9% and 96.9%, respectively. They found that MRI followed by MRI-TB reduces the detection of low-risk PCa and reduces the number of men requiring biopsy while improving the overall rate of detection of intermediate/high-risk PCa.
Study by Baco et al. (15)
This randomized clinical trial (RCT) included 175 biopsy-naive patients with suspicion for PCa, randomized to an MRI group (n=86) and a control group (n=89). In the MRI group, two-core MRI-TB guided by computer-assisted fusion of MRI-suspicious lesions was followed by 12-core SB. In the control group, two-core TB for abnormal digital rectal examination (DRE) and/or TRUS-suspicious lesions and 12-core SB were performed. In patients with normal MRI or DRE/TRUS, only 12-core SB was performed. The detection rates for any cancer and CSC were compared between the two groups and between TB and SB. The CDR for any cancer (MRI group 51/86, 59%; control group 48/89, 54%; P=0.4) and CSC (38/86, 44% vs. 44/89, 49%; P=0.5) did not significantly differ between both groups. Detection of CSC was comparable between two-core MRI-TB (33/86, 38%) and 12-core SB in the control group (44/89, 49%; P=0.2). In a subset analysis of patients with normal DRE, CSC detection was similar between two-core MRI-TB (14/66, 21%) and 12-core SB in the control group (15/60, 25%; P=0.7). Among biopsy-proven CSCs in MRI group, 87% (33/38) were detected by MRI-TB. The definition of CSC was based only on biopsy outcomes.
In conclusion they showed that overall CSC detection was similar between the MRI-TB and control groups. Two-core MRI-TB was comparable to 12-core SB for CSC detection.
Study by Porpiglia et al. (4).
This RCT included 212 biopsy-naive patients with suspected PCa (PSA level <15 ng/mL and negative DRE results). Patients were randomized into a prebiopsy MRI group (arm A, n=107) or a systematic biopsy group (arm B, n=105). In arm A, patients with MRI evidence of lesions suspected for PCa underwent MRI-TB (n=81). The remaining patients in arm A (n=26) with negative MRI results and patients in arm B underwent 12-core SB. The primary end point was to compare the detection rate of PCa and CSC between the two arms of the study. The secondary end point was to compare the CDR between TB alone and SB.
The overall detection rates were higher in arm A versus arm B for PCa (50.5% vs. 29.5%, respectively; P=0.002). The same was found for CSC PCa (43.9% vs. 18.1%; arm A vs. arm B; P<0.001).
Concerning the biopsy approach, the overall detection rates were significantly different for PCa (60.5% vs. 19.2% vs. 29.5%, TB in arm A vs. SB in arm A vs. SB in arm B; P<0.001) and for CSC PCa (56.8% vs. 3.8% vs. 18.1%, respectively; P<0.001). The reproducibility of the study could have been affected by the single-centre nature. They concluded that a diagnostic pathway based on MRI had a higher detection rate than the standard pathway in both PCa and CSC. The comparative results of reviewed series are summarized in Table 1.
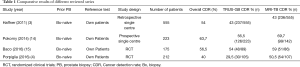
Full table
PROMIS study (Ahmed et al. ASCO abstract 2016)
Ahmed et al. proposed that in men with clinical suspicion of prostate cancer, those with favourable MRI results could safely avoid unnecessary biopsy. The inclusion criteria were patients with no prior biopsy referred with clinical suspicion of prostate cancer. It was a non-randomised study where each patient received pre-biopsy MRI followed by 5 mm TTMB and TRUS-GB of the prostate. To make comparison each patient acts as their own control.
The aim of this investigation was to define the proportion of men who could safely avoid biopsy and the rate of men correctly identified to have CSC. Another objective was to reduce over-diagnosis of clinically insignificant cancer. In this trial the use of MRI as a tool in the diagnosis of prostate cancer pretend to detect as well as rule-out clinically significant cancer and the TTMB was used as a reference test. A total of 6 centres recruiting up to 714 men to have all 3 tests to assess the ability of MRI to identify men who can safely avoid unnecessary biopsy. They also tried to estimate the cost-effectiveness of an MRI based diagnostic pathway and implications of alternative diagnostic strategies for NHS cost and men’s quality-adjusted survival duration. The histological definition of clinically significant cancer included Gleason score > 4+3 and/or maximum cancer core length >6 mm. Both radiologists and urologists were blinded to MRI results.
The diagnostic accuracy for CSC at MRI (PIRADS scores 3, 4, 5) in 576 patients were Se 93%, Sp 41%, PPV 51%, NPV 89%. The diagnostic accuracy for CSC at TRUS-GB were Se 48% Sp 96%, PPV 90%, NPV 74%. The high NPV of prostate MRI at 1.5 Tesla justify its use as a triage test to identify those men who might avoid a primary biopsy.
They concluded TRUS-GB has poor attributes for a diagnostic test. Otherwise, MRI prior to TRUS-GB can identify at least one quarter of men presenting with an elevated PSA who might safely avoid prostate biopsies. Furthermore, MRI followed by biopsy can reduce the over-diagnosis of clinically insignificant prostate cancer and it could identify over 90% of men with CSC.
The evidence produced by PROMIS will aid current research interest investigating the possibility of directing biopsies only to the suspicious areas on MRI without deploying SB. PROMIS did not include targeting of biopsies to MRI-suspicious regions, so whilst the performance of MRI against a good reference standard was assessed, the question of whether an MRI-targeted biopsy approach would be better than TRUS-GB in clinically significant cancer detection is not answered by this trial. Other important limitations in this type of paired cohort design are that performance of the TRUS-GB, which was performed after a lengthy detailed intensive mapping biopsy. It may be compromised in a swollen gland, when the operating surgeon was tired and when conscious or unconscious bias in TRUS-GB performance cannot be ruled out.
Much research has focused on developing and validating novel imaging and tissue biomarkers for early detection of clinically significant prostate cancer. These programmes of research have used TRUS-GB as the reference test with any volume, grade and risk of cancer taken as a ‘positive’. PROMIS aims to overcome the problems of TRUS-GB as a reference test by using TTMB that have a very high degree of accuracy and can be applied to all eligible men. It therefore represents an opportunity to develop and validate numerous imaging and tissue biomarkers in their performance characteristics to discriminate between men at risk who have absence of clinically significant cancer and those men who have clinically significant cancer.
Is it necessary to validate prospectively this diagnostic pathway? Is an International RCT where TB only versus SB were compared necessary? The answer may be yes as shown by ongoing investigations.
Tonttila et al. demonstrated contradictory results when they performed a randomized prospective blinded controlled trial, where they didn’t find an improvement on the prostate cancer detection rate between the group with multi-parametric MRI (mpMRI) target biopsy and the control group respectively (63% vs. 57%, P=0.5) (16).
The use of MRI before biopsies in routine for all patients is effective in Lille center (A.Villers) since 2004 (same day outpatient procedure). Targeted biopsies are performed in case of lesion sore 3, 4 or 5 at MRI. However, 12 systematic biopsies are still routinely performed in addition to targeted biopsies in case of lesion PI-RADS ≥ 3 at mpMRI.
At University College Hospital London, pre-biopsy MRI is carried out in the majority of patients with exception of those who are have contraindications for MRI or those within specific clinical trials. There is a one-stop service, where men with raised PSAs will have a multi-parametric MRI in the morning, which is reported by a radiologist within 3 hours. The result of the MRI is discussed with patients in the afternoon. Decisions on whether to proceed to biopsy are made as a joint decision by the patient and clinician after presenting them with their approximate likelihood of clinically significant cancer being identified based on institutional data. For patients with an MRI that score 3, 4 or 5, the majority will have a MRI targeted-only transperineal biopsy on the same day, under local anaesthetic, with around 3-5 biopsy cores taken per lesion. Patients with non-suspicious MRIs will generally not undergo biopsy but will be followed up with PSA surveillance.
Ongoing studies
MRI-FIRST-01 study (17)
The study included French centres and started in 2015. In this study they compare the percentage of patients with PCa Gleason score ≥7 detected by SB and TB. The secondary outcome is to compare the percentage of patients with CSC (defined as any Gleason ≥7 cancer or Gleason 6 cancer with at least one sample with ≥6 mm of cancer) detected by SB and TB.
All patients undergo a prostate MRI and SB. The patient acts as their own control. The suspicion of malignancy of each focal lesion is evaluated using Likert scale (from 1=definitely benign to 5=definitely malignant). SB and TB are performed during the same procedure. SB are performed by an operator blinded to mpMRI results. Twelve samples are obtained. The operator is free to obtain two additional biopsies to target any hypo-echoic lesion that would not have been sampled by SB. A second operator performs TB based on MRI findings. Only lesions with a subjective Likert score ≥3/5 are targeted. A maximum of two lesions are targeted. In case of more than two lesions with a subjective Likert score ≥3/5, the operator chose the most suspicious ones. Three samples are obtained from each targeted lesions. Thus, the patient has a maximum of 6 targeted samples. If MRI does not show any lesion with a subjective Likert score ≥3/5, only SB are obtained.
PRECISION study
This international multi-centre randomised controlled trial aims to assess the detection rate of cancer of MRI-TB compared to 12-core SB in naïve men referred with clinical suspicion of prostate cancer. Hypothesis is that the proportion of men with clinically significant cancer detected by MRI-TB will be no less than that detected by SB. Study was designed by the START consortium (18), started in 2015 and will end in 2017.
PRECISION study is the first randomised study in biopsy-naïve men in which men are randomised to an MRI targeted-alone biopsy arm (no biopsies of MRI-normal areas of prostate and no biopsy at all if the MR is non-suspicious) or a standard 12-core TRUS biopsy arm. This will allow evaluation of the efficacy of the MRI-TB approach in the detection of CSC. In order to evaluate a biopsy technique that could replace standard of care, the standard of care test, i.e., TRUS biopsy, must be included in one of the arms to allow a direct comparison.
The potential implications of this trial include: a redefining of the prostate cancer diagnostic pathway, a reduction in the number of patients undergoing prostate biopsy, a reduction in the number of biopsy cores taken per patient, a reduction in biopsy-related sepsis, pain and other side effects, a reduction in the over-diagnosis of clinically insignificant prostate cancer, a reduction of the economic burden of diagnosing and treating prostate cancer.
In the MRI arm, areas of the prostate are scored on a 5 point scale of suspicion for clinically significant cancer: Each suspicious area will be given a separate score as described by consensus meeting recommendations (8,18). Areas scoring 3, 4 or 5 will undergo targeted biopsy using the information from the MRI to influence biopsy conduct. Up to three suspicious areas will be targeted with a maximum of 4 cores per target leading to a maximum of up to 12 cores per patient. In the control arm, patients will undergo a 12 core SB.
The aim of this study is to assess the DR of men with CSC detected, evaluated according to two definitions: definition 1: a single core containing Gleason Grade 3+4 disease or greater; definition 2: a single core containing Gleason Grade 4+3 disease or greater. The secondary outcomes will include: proportion of men with clinically insignificant cancer detected, proportion of men in MRI arm who avoid biopsy, proportion of men in whom MRI score for suspicion of CSC is 3, 4 or 5 but no CSC is detected, cancer core length (CCL) of the most involved biopsy core.
Conclusions
Despite the diagnosis of many other solid organs cancers such as breast and colorectal cancer is based on image-guided biopsy, the targeted biopsy approach is not part of the traditional prostate cancer diagnostic pathway. Implementing this approach may improve our ability to diagnose CSC and our ability to avoid detecting clinically insignificant cancer. However, robust comparative evidence from randomised controlled trials is needed.
In the near future it may be possible to postpone the initial biopsy in naïve patients with non-suspicious prostate MRI, taking in consideration other parameters like family history of prostate cancer, race, PSA kinetics, available before the diagnostic procedure. The decision about when and how to perform a prostate biopsy continues being a urologic craft process.
Acknowledgements
Thanks are due to H. Joaquin Alvarez Garzón, MD (from Privado Hospital University Medical Center, Cordoba, Argentine) for his valuable contribution.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Villers A, Puech P, Mouton D, et al. Dynamic contrast enhanced, pelvic phased array magnetic resonance imaging of localized prostate cancer for predicting tumor volume: correlation with radical prostatectomy findings. J Urol 2006;176:2432-7. [Crossref] [PubMed]
- Hoeks CM, Vos EK, Bomers JG, et al. Diffusion-weighted magnetic resonance imaging in the prostate transition zone: histopathological validation using magnetic resonance-guided biopsy specimens. Invest Radiol 2013;48:693-701. [Crossref] [PubMed]
- Haffner J, Lemaitre L, Puech P, et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int 2011;108:E171-8. [Crossref] [PubMed]
- Porpiglia F, Manfredi M, Mele F, et al. Diagnostic Pathway with Multiparametric Magnetic Resonance Imaging Versus Standard Pathway: Results from a Randomized Prospective Study in Biopsy-naïve Patients with Suspected Prostate Cancer. Eur Urol 2016. pii: S0302-2838(16)30509-7.
- Mowatt G, Scotland G, Boachie C, et al. The diagnostic accuracy and cost-effectiveness of magnetic resonance spectroscopy and enhanced magnetic resonance imaging techniques in aiding the localisation of prostate abnormalities for biopsy: a systematic review and economic evaluation. Health Technol Assess 2013;17:vii-xix, 1-281. [Crossref] [PubMed]
- Hutchinson RC, Costa DN, Lotan Y. The economic effect of using magnetic resonance imaging and magnetic resonance ultrasound fusion biopsy for prostate cancer diagnosis. Urol Oncol 2016;34:296-302. [Crossref] [PubMed]
- de Rooij M, Crienen S, Witjes JA, et al. Cost-effectiveness of magnetic resonance (MR) imaging and MR-guided targeted biopsy versus systematic transrectal ultrasound-guided biopsy in diagnosing prostate cancer: a modelling study from a health care perspective. Eur Urol 2014;66:430-6. [Crossref] [PubMed]
- Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. Eur Urol 2016;69:16-40. [Crossref] [PubMed]
- Moore CM, Robertson NL, Arsanious N, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol 2013;63:125-40. [Crossref] [PubMed]
- Kasivisvanathan V, Dufour R, Moore CM, et al. Transperineal magnetic resonance image targeted prostate biopsy versus transperineal template prostate biopsy in the detection of clinically significant prostate cancer. J Urol 2013;189:860-6. [Crossref] [PubMed]
- Moore CM, Kasivisvanathan V, Eggener S, et al. Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: recommendations from an International Working Group. Eur Urol 2013;64:544-52. [Crossref] [PubMed]
- Fütterer JJ, Briganti A, De Visschere P, et al. Can Clinically Significant Prostate Cancer Be Detected with Multiparametric Magnetic Resonance Imaging? A Systematic Review of the Literature. Eur Urol 2015;68:1045-53. [Crossref] [PubMed]
- Schoots IG, Roobol MJ, Nieboer D, et al. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 2015;68:438-50. [Crossref] [PubMed]
- Pokorny MR, de Rooij M, Duncan E, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol 2014;66:22-9. [Crossref] [PubMed]
- Baco E, Rud E, Eri LM, et al. A Randomized Controlled Trial To Assess and Compare the Outcomes of Two-core Prostate Biopsy Guided by Fused Magnetic Resonance and Transrectal Ultrasound Images and Traditional 12-core Systematic Biopsy. Eur Urol 2016;69:149-56. [Crossref] [PubMed]
- Tonttila PP, Lantto J, Pääkkö E, et al. Prebiopsy Multiparametric Magnetic Resonance Imaging for Prostate Cancer Diagnosis in Biopsy-naive Men with Suspected Prostate Cancer Based on Elevated Prostate-specific Antigen Values: Results from a Randomized Prospective Blinded Controlled Trial. Eur Urol 2016;69:419-25. [Crossref] [PubMed]
- Assessment of Prostate MRI Before Prostate Biopsies (MRI-FIRST01). 2016. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02485379?term=MRI+first&rank=1
- Dickinson L, Ahmed HU, Allen C, et al. Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting. Eur Urol 2011;59:477-94. [Crossref] [PubMed]


