Neoplastic diseases of the spermatic cord: an overview of pathological features, evaluation, and management
Introduction
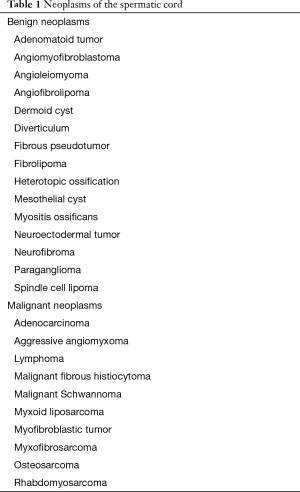
Neoplasms of the spermatic cord are very rare. These tumors are classified as extracellular and most are benign. They usually originate in the mesothelial layer. Along with benign neoplasms, malignant neoplasms are classified and listed on Table 1.
Full table
Diagnosing of the spermatic cord masses is critical during the clinical examination. This region is often overlooked and examination results are unclear. If mass suspicion is detected via palpation during a physical examination, the primary imaging modality used is ultrasonography (US) to visualize the mass. Other imaging modalities should be used to further visualize the mass and prepare for surgery to excise the mass.
Anatomy & embryology
Anatomy
The spermatic cord begins at the inferior abdomen and ends at the scrotum. The contents of the spermatic cord are bound together and covered by three fascial layers: external spermatic fascia, cremaster muscle and fascia, and internal spermatic fascia. All three fascial layers are covered by another layer, known as the superficial fascia, which is found directly below the scrotal skin. The spermatic cord contains many structures, vessels, and nerves which supply blood and signals to and from the testis. The major structure found in the spermatic cord, is the testicular artery, branching off the aorta, inferior to the renal arteries. Next is the artery and vein supplying blood to the cremasteric fascia and muscle, via the cremasteric artery and vein. The artery to the vas deferens is also found in the spermatic cord, branching off the inferior vesicle artery, which arises from the internal iliac.
Embryology
Formation of the spermatic cord is done at the opening of the inguinal canal, also known as the deep inguinal ring.
Benign neoplasms
Adenomatoid tumor of the spermatic cord
Adenomatoid tumor of the spermatic cord is a rare neoplasm, which is classified as a paratesticular tumor. These tumors originate in the mesothelium (1). There are very few cases of primary adenomatoid tumor of the spermatic cord in the literature. Miyoshi et al. presented a case of adenomatoid tumor of the spermatic cord. The tumor was asymatomatic and was untreated for years, after the patient had noticed an irregularity in the scrotum. Palpation was used to identify the presence of a mass. The tumor was removed surgically under local anesthesia. Histology of this tumor is very unique, presenting with lumens on the smooth muscles and vacuoles of lymphatic nodules (2).
Angiomyofibroblastoma of the spermatic cord
Angiomyofibroblastoma of the spermatic cord is a benign soft tissue tumor. There are only two reported cases of primary angiomyofibroblastoma of the spermatic cord. Tzanakis et al. presented a case of a man with an asymptomatic mass. A surgical procedure was done. The tumor consisted of spindle-shaped cells, uniquely differentiating it aggressive angiomyxoma and other malignant tumors (3).
Angioleiomyoma of the spermatic cord
Angioleiomyoma of the spermatic cord is a rare, benign lesion. Ghei et al. presented a case of this rare tumor. Using US and magnetic resonance imaging (MRI), the mass was identified. Scrotal exploration was conducted to learn more about the mass. Local excision was conducted to remove the tumor and is the accepted treatment option (4).
Angiofibrolipoma of the spermatic cord
Angiofibrolipoma of the spermatic cord consists of adipocytes, vascular tissue, and collagenous connective tissue, observed through pathological studies. Physical examination identified the presence of a mass in the right spermatic cord. Using US, a cystic mass was found. Under general anesthesia, the tumor was excised from the spermatic cord, with no reoccurrence in the follow-up (5).
Dermoid cyst of the spermatic cord
Dermoid cyst, also known as teratoma, arises in the epidermis. It can present itself in children (6) or adults (7). Dermoid cysts are common, but rare originating in the spermatic cord (6). Salemis et al. presented a rare case of a large cyst which presented as an incarcerated inguinal hernia. Lichtenstein polypropylene mesh repair was used to treat dermoid cyst of the spermatic cord (8). Skorniakov et al. presents a rare case of dermoid cyst of the spermatic cord. In this case, physical examination and US were inconclusive in identifying the mass, so a surgical exploration was conducted and excision was done to remove the mass (7).
Diverticulum of the spermatic cord
Diverticulum is an outpouching of a hallow structure in the body. A unique case of diverticulum that involved the spermatic cord was presented by Grigor et al. This case of diverticulum of the spermatic cord was presented as asymptomatic. The discovery was made during a repair of inguinal hernia. A nodule was found similar to a melanoma metastasis attached to the spermatic cord. Upon excision, histology report indicated a detached colonic diverticulum, which parasitized onto the spermatic cord (9). There is no report of primary diverticulum of the spermatic cord in the literature.
Fibrous pseudotumor of the spermatic cord
Fibrous pseudotumor of the spermatic cord is classified as a rare benign tumor, which most commonly occurs in the paratesticular region, originating from the intrascrotal tissue. Dieckmann et al. presented two cases of fibrous pseudotumor of the spermatic cord. In both cases, the mass was painless. Original suspicion during the clinical examination was a malignant growth. US confirmed the mass on the spermatic cord in the first patient. MRI was used to confirm a mass in the second patient. Patients underwent local excision to remove the mass. Follow-ups indicated no recurrence in the patients. Histology found collagen-rich, fibrous tissue (10).
Fibrolipoma of the spermatic cord
Fibrolipomas are subtype of lipoma, which are benign neoplasms. Fibrolipoma of the spermatic cord is a rare entity. Terada et al. presented a case of an individual with fibrolipoma of the spermatic cord. The patient found a mass in the inguinal region. Tumorectomy and right orchiectomy was used to excise the tumor. Microscopic study showed the tumor composing of adipose tissue (11). Diagnoses can be done using US and computerized tomography (CT), which clearly identifies the mass (12).
Heterotopic ossification of the spermatic cord
Heterotopic ossification of the spermatic cord is a rare case of bone formation. The literature has reported very few cases of this pathology. Demirci et al. presented a case of a patient with bone development of the spermatic cord. The patient had a history of pain and swelling and scrotal tenderness. The patient tried self-medication using anti-inflammatory agents to reduce pain and swelling. A physical examination showed a long mass localized to the spermatic cord and laboratory studies were clean. US and MRI were used to diagnose the mass, with both depicting similar findings. The treatment approach for the patient was decided as a radical orchiectomy (13).
Mesothelial cyst of the spermatic cord
Mesothelial cyst of the spermatic cord is a rare pathology, and often misdiagnosed as cryptorchidism. Excision of the mass was done. Patient recovered normally without any complications. There was no retraction of the testis into the groin (14).
Myositis ossificans of the spermatic cord
Myositis ossificans is the calcification of the muscle, most commonly in the arms or quadriceps. Ozgür et al. presented a case of a patient admitted through outpatient clinical, because the patient noticed a mass growing in the inguinal region. Physical examination revealed a hard mass which was painless, combined with hydrocele. Imaging modalities, US and MRI, were used to locate the mass. Blunt and sharp dissection was used to separate the mass from surrounding structures and orchiectomy to remove the mass from the spermatic cord. Microscopic examination revealed bone structure with dense fibrous tissue (15).
Neuroectodermal tumor of the spermatic cord
Primary neuroectodermal tumor of the spermatic cord is a rare neoplastic manifestation. of a neoplasm. There are only two cases of this pathology in the literature. In both cases, the tumor was asymptomatic. The mass was palpable, and diagnostic studies such as US, MRI, and CT were used to confirm the mass. Surgical excision of the tumor was performed using radical orchiectomy. Histology and immunohistochemical staining was used in both cases to confirm the diagnosis of neuroectodermal tumor, which presented with small round cells. The immunohistochemical staining was inconclusive for CD99 (16) in one case but not the second case (17), but confirmed for vimentin and CD56 (17). In both cases, chemotherapy was advised to control the tumor reoccurrence (16,17).
Neurofibroma of the spermatic cord
Neurofibroma of the spermatic cord is a rare pathology. It is found on the peripheral nerve, composed of Schwann cells and fibroblasts. Though these lesions are benign, they have the potential to cause significant morbidity and psychological distress. US, MRI, CT, and positron emission tomography can all be used to identify the presence of the mass. Surgical resection is the best means of treatment and final diagnosis must be made using histopathology (18-21).
Paraganglioma of the spermatic cord
Presentation of paraganglioma of the spermatic cord is asymptomatic. Kwon et al. recently described a case of this pathology. US clearly identified the mass and orchiectomy was used to remove it. Histopathology showed features of malignancy, PET-CT was done on the whole body to determine metastasis of the tumor. PET-CT did not find any other lesions (22).
Spindle cell lipoma of the spermatic cord
Spindle cell lipoma commonly occurs as a solitary subcutaneous, circumscribed lesion in the back. Manifestation on the spermatic cord is an extremely rare occurrence. Ide et al. presented a case of a patient who was referred because of right scrotal mass. Using US, MRI, and CT, the mass was identified as a tumor. After local excision was requested by the patient, tumor was removed without rupture. Histopathology, showed the tumor with mature adipose tissue missed with spindle cells and collagen fibers. Histopathology showed the tumor with mature adipose tissue along with spindle cells and collagen fibers. A hallmark of spindle cell lipomas is a positive stain of CD34, which was confirmed with this patient, along with vimentin and bcl-2 combined, confirmed the diagnoses of spindle cell lipoma (23).
Malignant neoplasms
Adenocarcinoma of the spermatic cord
Adenocarcinoma of the spermatic cord, though rare, presents with groin discomfort and swelling. The mass is palpable in the scrotum and the inguinal area (24). The most common occurrence of adenocarcinoma of the spermatic cord is due to metastasis from the stomach due to gastric cancer (24-26). Prognosis of patients with adenocarcinoma of the spermatic cord tends to be poor. However, in two cases presented by Kim et al., the follow-up was proven to be favorable (24). Histopathology reveals signet ring cells to identify the adenocarcinoma. US, MRI, and CT were all done to develop a proper image of the mass and determine if metastasis had prevailed. Multiple cycles of adjuvant chemotherapy was used with folinic acid, fluorouracil, and oxaliplatin (24).
Aggressive angiomyxoma of the spermatic cord
Minagawa et al. presented a case of a 37-year-old man who presented with a left lower abdominal mass. Clinical interpretation believed it to be an inguinal hernia. MRI revealed an inguinal mass extending from the left spermatic cord (27). In another case, CT was used to identify the mass (28). Surgical intervention was used to excise the mass and no recurrence was observed following the surgery (27). Aggressive angiomyxoma is more common in females than in males. It is extremely rare in males, more so in the inguinal region. It is locally aggressive but non-metastasizing (29). Patients commonly present with inguinal and scrotal swelling (27,30). Immunohistochemical results show emphasis on hormone receptors for estrogen and progesterone (31).
Lymphoma of the spermatic cord
Lymphomas of the spermatic cord are a rare occurrence (32). They can present as unilateral or bilateral masses with or without pain. These non-Hodgkin lymphomas are primary tumors that can be confused with testicular tumors that have extended into the spermatic cord (33). The most common form is diffuse large B-cell lymphomas reported in patients over 60, with a few reported cases of Burkitt’s lymphoma presenting in a 4-year-old boy and a 20-year-old young man (32-37). A recent study utilized different imaging modalities to characterize a primary spermatic cord tumor and distinguish it from other tumors presenting similarly; they reported preservation of normal funicular vessels, lack of fat within the lesion, as well as homogenous enhancement and intensity on MRI (33). Imaging is typically followed by radical orchiectomy and immunohistochemistry is utilized to confirm the diagnosis. Non-Hodgkin lymphomas stain positive for CD20 among other markers and stain negative for CD3 and other markers (32-36). Generally spermatic cord lymphomas are known to have a poor prognosis but recent case studies show a good response to treatment (32). The patients were treated aggressively with multiple cycles of combination chemotherapy which includes rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone with some variation and additional therapy determined per case (32,34,35).
Malignant fibrous histiocytoma (MFH) of the spermatic cord
MFH is the most common soft tissue sarcoma in adults, however it is very rare for it to present as a primary spermatic cord tumor (38). It is generally a unilateral mass that is identified by imaging and requires a biopsy for a definitive diagnosis (39). Morphologically it is described to be a gray-yellow (sometimes white), elastic but hard mass (40-44). It is classified into four types based on microscopic examination: storiform-pleomorphic, giant cell, inflammatory, and myxoid of which the storiform-pleomorphic is the most common (42). The storiform-pleomorphic type is identified by abnormal spindle cells in a storiform or “star-like” pattern and giant cells with variation in size of nuclei (40-42,44). The inflammatory type shows tumor cells with neutrophils permeating the tissue (43). Immunohistochemistry for MFH is positive for CD68 and vimentin and negative for cytokeratin and desmin with certain variations between cases (40-42,44,45). These tumors have a high chance of reoccurrence in the same area and/or metastasis (41,42,46). One case showed reoccurrence after 8 years with metastasis to the liver, lung, adrenal gland, bone, and mesenteric lymph nodes (46). The most common and recommended treatment option is surgical removal of the tumor using a wide local excision which can be followed up with radiotherapy (38,40,47). In some cases, chemotherapy agents such as ifosfamide and doxorubicin are used (41,43).
Malignant schwannoma of the spermatic cord
Malignant schwannoma or a neurilemmoma arises from the Schwann cells within the peripheral nerve sheaths (48,49). Though it is of unknown etiology, it is seen in patients with von Recklinghausen’s disease which can present as a neurofibromatosis type II gene deletion or alteration (48,49). This rarely occurs in the male genital area and there are very few cases reported of malignant schwannoma in the spermatic cord (50-52). Jiang et al. reports a case in a 20-year-old man who presented with a unilateral mass emerging from the spermatic cord which was hypoechoic on US (50). A biopsy is done for a definitive diagnosis; in this case, histology demonstrated spindle-shaped cells with elongated polymorphic nuclei (50). Immunohistochemistry for malignant schwannoma is positive for vimentin and S-100 protein and negative for smooth muscle actin—this is used to assist diagnosing the tumor (48,50). These patients typically have the tumor resected surgically; reoccurrence was not reported in the cases we reviewed (51,53).
Myxoid liposarcoma of the spermatic cord
Myxoid liposarcoma is the most common type of liposarcoma named for its myxoid matrix; it is also characterized to be a vascular tumor with low amounts of fat (54). It usually presents as an inguinal mass that is often mistaken for an inguinal hernia (54-56). Due to its unclear presentation, Abete et al. looked into imaging modalities which would assist in diagnosis (57). Their pre-operative diagnosis was based on a combination of MRI and US imaging; while the tumor had a cyst-like appearance on MRI, the vascularity of the tumor mass can be visualized on US (57). The tumor can also be diagnosed from its distinct histologically appearance post-biopsy, as discussed earlier. There is variability in the immunohistochemistry reported for these tumors (54,55). In most cases, the tumor was encapsulated with regular borders and therefore it was surgically removed without recurrence (55,57-59). There is one report of reemergence of the myxoid liposarcoma and metastasis to the liver after surgery (60).
Myofibroblastic tumor of the spermatic cord
Myofibroblastic tumors of the spermatic cord are identified by different names in literature: inflammatory myofibroblastic tumor (IMT), pseudosarcomatous myofibroblastic proliferation, and proliferative funiculitis (61-63). Case reports describe it to be a “painless scrotal mass” where US imaging can help detection but insufficient for an accurate diagnosis (61). There is controversy between a few earlier papers which claim IMT to be a benign mass while others refer to it as a low-grade malignant tumor (64-66). Fine needle aspiration or tumor biopsy is used to examine the tumor histology and immunochemistry (61,64). Histologically, the tumor is a composed of myofibroblasts and fibroblasts which appear spindle-shaped along with permeating inflammatory cells (61,62,64,67,68). Coffin et al. described three different patterns which would present similar to a nodular fasciitis, a fibrous histiocytoma, or a desmoid (66). As a result, immunohistochemistry is very important in distinguishing the tumor from others on the differential diagnosis (61). While most tumors stain positive for vimentin and negative for S-100 protein, there is variation in markers such as SMA and ALK among cases (61). Coffin et al. stresses the importance of anaplastic lymphoma kinase (ALK) as a marker that assists in predicting the prognosis of the tumor—ALK is positively correlated with lower chances of metastasis (69). Patients were most frequently treated by wide surgical excision of the tumor and showed favorable results (61-64,67).
Myxofibrosarcoma (MFS) of the spermatic cord
MFS is also used for the myxoid type MFH (70,71). MFS in the spermatic cord is a soft tissue tumor that presents as a painful or painless scrotal mass (70,72). The tumor can be de novo or due to prior exposure to radiation (73). The tumor is composed of abnormal spindle cells within a myxoid background (70-73). Well-differentiated and dedifferentiated liposarcomas are often found to resemble MFS, however, they consist of lipoblasts which are absent in MFS, therefore immunohistochemistry can also be used to reach the correct diagnosis (74-76). MFS is similar to MFH as it is positive for vimentin and stains negative for S-100 and myogenin (71,73). Studies report high chances of recurrence as well as metastasis with MFS (71-73). These tumors are distinguished as high-grade or low-grade to determine prognosis and guide treatment recommendations (72,73). For all cases, surgical excision of the tumor is recommended. However, depending on the grade of the tumor, surgery will be preceded or followed by chemotherapy or radiotherapy (70,71,73).
Osteosarcoma of the spermatic cord
There are very few reported cases of primary extraskeletal osteosarcoma of the spermatic cord (77-79). Patients present with a painless mass that is generally calcified on a CT scan (77,78). The tumor is often described to have “bone trabecules” along with malignant cells, spindle cells, or giant cells which are multinucleated (77,78,80). In certain reported cases, this histologic appearance is combined with liposarcoma or other tumor types such as in cases of malignant mesenchymoma (80-82). There is no mention of immunohistochemistry of the tumor as it is distinguished histologically. The treatment for this tumor involves a wide surgical excision of the tumor along with tissues in nearby proximity; at times, this includes a radical orchiectomy and ligating the spermatic cord to prevent reoccurrence (77,78,80). In certain cases, the surgery is followed by radiotherapy or chemotherapy (77). Beiswanger et al. reports a patient with the combined presentation of osteosarcoma of the spermatic cord and renal cell carcinoma; the patient showed no recurrence after surgical excision of the osteosarcoma and partial bilateral nephrectomies (78).
Rhabdomyosarcoma of the spermatic cord
Rhabdomyosarcoma is different from the other spermatic cord malignancies as it commonly presents at an earlier age, typically around age 4 and 18Jeny (83-85). However, there are reports of rhabdomyosarcoma in the adult population (84,86,87). The tumor can arise from the normal muscle tissue in the male genital area or from mesoderm that has not differentiated (84,87,88). It is described to be a hard but painless mass found in the inguinal or scrotal region appearing grayish white and lobular when removed (84,85,88,89). Bouchikhi et al. discusses using imaging modalities to eliminate other possible tumors, however tumor histology is necessary for a definitive diagnosis (85). There are four histological types of rhabdomyosarcoma: embryonal, pleomorphic, alveolar, and mixed type (90). As the name suggests, histologically one would see rhabdomyoblast with multiple nuclei, mitotic activity, and other tumor cell characteristics (84,85). On immunochemistry, the tumor is identified by its positive staining for desmin and myogenin (84,85,88). These tumors are capable of metastasizing, therefore the abdomen and lungs are frequently examined upon diagnosis (85,86,88-90). The suggested treatment for this tumor in all cases has been a radical inguinal orchiectomy followed by cycles of chemotherapy—typically VAC which includes vincristine, actinomycin, and cyclophosphamide (84-91).
Summary
Evidently, neoplasms are rare occurrences within the spermatic cord. Understanding the significance in rare findings are crucial factors in order for an accurate and timely diagnosis. Although the classifications of tumors appear to be painless and ignorable, a proper analysis may reveal possible linkages to other sources of irregularity such as discomfort or carcinoma. Therefore, emphasizing further research on some of these overlooked results would lead to advancements in diagnostic and management strategies.
Acknowledgements
The authors are thankful to Drs. Kelly Warren, Todd Miller, and Peter Brink for departmental support, as well as Mrs. Wendy Isser and Ms. Grace Garey for literature retrieval.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Liu W, Wu RD, Yu QH. Adenomatoid tumor of the testis in a child. J Pediatr Surg 2011;46:E15-7. [Crossref] [PubMed]
- Miyoshi N, Noda S, Eto K, et al. Adenomatoid tumor of the spermatic cord. Kurume Med J 1980;27:97-100. [Crossref] [PubMed]
- Tzanakis NE, Giannopoulos GA, Efstathiou SP, et al. Angiomyofibroblastoma of the spermatic cord: a case report. J Med Case Rep 2010;4:79. [Crossref] [PubMed]
- Freeman SS, Udomphorn Y, Armstead WM, et al. Young age as a risk factor for impaired cerebral autoregulation after moderate to severe pediatric traumatic brain injury. Anesthesiology 2008;108:588-95. [Crossref] [PubMed]
- Liu QL, Tian B, Zhang H, et al. Angiofibrolipoma of the spermatic cord. Asian J Androl 2009;11:746-7. [Crossref] [PubMed]
- Prada-Arias M, Ortiz-Rey JA, Fernández-Eire P, et al. Dermoid cyst of the spermatic cord in children. J Pediatr Surg 2010;45:2058-60. [Crossref] [PubMed]
- Skorniakov MS, Ramírez AC, Delgado MS, et al. Spermatic cord dermoid cyst as paratesticular mass. Case report and bibliographic review. Arch Esp Urol 2011;64:991-4. [PubMed]
- Salemis NS, Karagkiouzis G, Sambaziotis D, et al. Large dermoid cyst of the spermatic cord presenting as an incarcerated hernia: a rare presentation and literature review. Hernia 2010;14:321-3. [Crossref] [PubMed]
- Grigor T, Ahmad S. Parasitised large intestinal diverticulum of the spermatic cord. BMJ Case Rep 2014;2014. pii: bcr2014206115.
- Dieckmann KP, Struss WJ, Frey U, et al. Paratesticular fibrous pseudotumor in young males presenting with histological features of IgG4-related disease: two case reports. J Med Case Rep 2013;7:225. [Crossref] [PubMed]
- Terada T. Giant fibrolipoma of the spermatic cord. Pathol Int 2010;60:330-2. [Crossref] [PubMed]
- Hegele A, Olbert P, Roessler M, et al. Inguinal fibrolipoma of the spermatic cord: discrepancies between clinical and histopathological findings. Urol Int 2003;71:435-6. [Crossref] [PubMed]
- Demirci D, Ekmekçioğlu O, Inci M, et al. Heterotopic ossification of the spermatic cord. Int Urol Nephrol 2003;35:513-4. [Crossref] [PubMed]
- Vaos G, Zavras N, Velaoras K, et al. Muesothelial cyst of the spermatic cord as a cause of acquired cryptorchidism. Hernia 2009;13:439-41. [Crossref] [PubMed]
- Ozgür A, Tarcan T, Simsek F, et al. An unusual tumor of the spermatic cord: myositis ossificans. Arch Esp Urol 2003;56:1072-4. [PubMed]
- Matsumoto H, Inoue R, Tsuchida M, et al. Primitive neuroectodermal tumor of the spermatic cord. J Urol 2002;167:1791-2. [Crossref] [PubMed]
- Gurung P, Attar K, Peters J. Primitive neuroectodermal tumor of the spermatic cord. Int J Urol 2010;17:679-80. [Crossref] [PubMed]
- Boto J, Boudabbous S, Lobrinus JA, et al. Solitary Neurofibroma Of The Spermatic Cord: A Case Report. J Radiol Case Rep 2015;9:19-28. [Crossref] [PubMed]
- Kishimoto N, Iwanishi T, Matsuzaki K, et al. A case of solitary neurofibroma of spermatic cord. Hinyokika Kiyo 2014;60:245-7. [PubMed]
- Hosseini MM, Geramizadeh B, Shakeri S, et al. Intrascrotal solitary neurofibroma: A case report and review of the literature. Urol Ann 2012;4:119-21. [Crossref] [PubMed]
- Milathianakis KN, Karamanolakis DK, Mpogdanos IM, et al. Solitary neurofibroma of the spermatic cord. Urol Int 2004;72:271-4. [Crossref] [PubMed]
- Kwon AY, Kang H, An HJ, et al. Spermatic Cord Paraganglioma With Histologically Malignant Features. Urology 2016;93:e7-8. [Crossref] [PubMed]
- Ide H, Nakagawa T, Kamiyama Y, et al. Spindle cell lipoma of the spermatic cord. Int J Urol 2007;14:1046-7. [Crossref] [PubMed]
- Kim JH, Kim DS, Cho HD, et al. Late-onset metastatic adenocarcinoma of the spermatic cord from primary gastric cancer. World J Surg Oncol 2014;12:128. [Crossref] [PubMed]
- Kanazawa Y, Kato S, Fujita I, et al. Spermatic cord tumor metastatic from stomach cancer 1 year after curative gastrectomy. J Nippon Med Sch 2013;80:318-23. [Crossref] [PubMed]
- Watanabe R, Inada K, Yamashita Y, et al. A case of metastatic tumor of the spermatic cord from gastric cancer. Hinyokika Kiyo 2013;59:195-9. [PubMed]
- Minagawa T, Matsushita K, Shimada R, et al. Aggressive angiomyxoma mimicking inguinal hernia in a man. Int J Clin Oncol 2009;14:365-8. [Crossref] [PubMed]
- Madrigal B, Veiga M, Vara A, et al. An aggressive inguinal (parafunicular) angiomyxoma in a male patient. Arch Esp Urol 1999;52:785-8. [PubMed]
- Tsang WY, Chan JK, Lee KC, et al. Aggressive angiomyxoma. A report of four cases occurring in men. Am J Surg Pathol 1992;16:1059-65. [Crossref] [PubMed]
- Malik A, Singh KJ, Mehta A. Aggressive angiomyxoma of the spermatic cord: A rare entity. Indian J Urol 2009;25:137-9. [Crossref] [PubMed]
- Idrees MT, Hoch BL, Wang BY, et al. Aggressive angiomyxoma of male genital region. Report of 4 cases with immunohistochemical evaluation including hormone receptor status. Ann Diagn Pathol 2006;10:197-204. [Crossref] [PubMed]
- Taguchi S, Takahashi S, Iida K, et al. Spermatic cord lymphoma: a case report and literature review. Case Rep Med 2012;2012:513707.
- Bertolotto M, Borsato A, Derchi LE. Lymphoma of the spermatic cord: sonographic appearance. J Clin Ultrasound 2014;42:509-12. [Crossref] [PubMed]
- Diakatou E, Haramis G, Kostopoulou A, et al. Primary lymphoma of the spermatic cord: a case report and review of the literature. Indian J Pathol Microbiol 2011;54:588-90. [Crossref] [PubMed]
- Natsuizaka M, Kudo M, Suzuki M, et al. Diffuse large B-cell lymphoma with massive portal vein tumor thrombosis in a patient with alcoholic cirrhosis: a case report and literature review. Intern Med 2009;48:805-8. [Crossref] [PubMed]
- Zhou Q, Leng DN, Zhang ZX, et al. Burkitt's lymphoma of the spermatic cord: a case report and review of the literature. Zhonghua Nan Ke Xue 2008;14:624-7. [PubMed]
- Zwanger-Mendelsohn S, Shreck EH, Doshi V. Burkitt lymphoma involving the epididymis and spermatic cord: sonographic and CT findings. AJR Am J Roentgenol 1989;153:85-6. [Crossref] [PubMed]
- Abou-Jaoude M, El Ali M. Malignant fibrous histiocytoma: a case report and literature review. Int Surg 2009;94:196-200. [PubMed]
- Carrión López P, Pastor Navarro H, Martínez Ruiz J, et al. Spermatic cord sarcomas: current status and report of four cases. Arch Esp Urol 2009;62:242-6. [PubMed]
- Xu LW, Yu YL, Li GH. Malignant fibrous histiocytoma of the spermatic cord: case report and literature review. J Int Med Res 2012;40:816-23. [Crossref] [PubMed]
- Demir L, Can A, Dirican A, et al. Malignant fibrous histiocytoma of the spermatic cord in a patient with polycystic kidney disease; review of the literature. Clin Genitourin Cancer 2012;10:280-3. [Crossref] [PubMed]
- Lin BT, Harvey DA, Medeiros LJ. Malignant fibrous histiocytoma of the spermatic cord: report of two cases and review of the literature. Mod Pathol 2002;15:59-65. [Crossref] [PubMed]
- Sekine Y, Ohki K, Okamoto K, et al. Malignant fibrous histiocytoma of the right spermatic cord: a case report. Int J Urol 2001;8:581-4. [Crossref] [PubMed]
- Bosch-Príncep R, Martínez-González S, Alvaro-Naranjo T, et al. Fine needle aspiration and touch imprint cytology of a malignant fibrous histiocytoma of the spermatic cord. Case report. Acta Cytol 2000;44:423-8. [Crossref] [PubMed]
- Ruiz Liso JM, Ruiz García J, Pardo López ML, et al. Inflammatory malignant fibrous histiocytoma of the spermatic cord infiltrating an inguinal leiomyoma. Case report with conceptual and bibliographic reviews. Arch Esp Urol 2008;61:485-98. [PubMed]
- Kamei J, Kume H, Suzuki M, et al. Eight-year postsurgery recurrence of malignant fibrous histiocytoma of the left spermatic cord. Nihon Hinyokika Gakkai Zasshi 2012;103:18-21. [Crossref] [PubMed]
- Rodríguez D, Olumi AF. Management of spermatic cord tumors: a rare urologic malignancy. Ther Adv Urol 2012;4:325-34. [Crossref] [PubMed]
- Giglio M, Giasotto V, Medica M, et al. Retroperitoneal ancient schwannoma: case report and analysis of clinico-radiological findings. Ann Urol (Paris) 2002;36:104-6. [Crossref] [PubMed]
- Sordillo PP, Helson L, Hajdu SI, et al. Malignant schwannoma--clinical characteristics, survival, and response to therapy. Cancer 1981;47:2503-9. [Crossref] [PubMed]
- Jiang R, Chen JH, Chen M, et al. Male genital schwannoma, review of 5 cases. Asian J Androl 2003;5:251-4. [PubMed]
- Pellice C, Cosme M, Casalots J. Schwannoma of the spermatic cord. Actas Urol Esp 1994;18:328-30. [PubMed]
- Corredera Zambrana M, Galbis Palau F, Cáceres Gómez F. Schwannoma of the spermatic cord. Report of a case. Actas Urol Esp 1983;7:485-8. [PubMed]
- Wagner RF, Beiden SV, Metz CE. Continuous versus categorical data for ROC analysis: some quantitative considerations. Acad Radiol 2001;8:328-34. [Crossref] [PubMed]
- Hsu YF, Chou YY, Cheng YH. Spermatic cord myxoid liposarcoma presenting as an incarcerated inguinal hernia: report of a case and review of literatures. Hernia 2012;16:719-22. [Crossref] [PubMed]
- Panagis A, Karydas G, Vasilakakis J, et al. Myxoid liposarcoma of the spermatic cord: a case report and review of the literature. Int Urol Nephrol 2003;35:369-72. [Crossref] [PubMed]
- McFadden DW. Myxoid liposarcoma of the spermatic cord. J Surg Oncol 1989;40:132-4. [Crossref] [PubMed]
- Abete L, Simonato A, Toncini C, et al. Myxoid liposarcoma of the spermatic cord: US and MR imaging findings. J Clin Ultrasound 2014;42:96-9. [Crossref] [PubMed]
- Lipset RE, Kirpekar M, Cooke KS, et al. US case of the day. Myxoid liposarcoma of the spermatic cord. Radiographics 1997;17:1316-8. [Crossref] [PubMed]
- Ikinger U, Westrich M, Pietz B, et al. Combined myxoid liposarcoma and angiolipoma of the spermatic cord. Urology 1997;49:635-7. [Crossref] [PubMed]
- Kashid YS, Bakshi GK, Joshi AS, et al. Myxoid liposarcoma of the spermatic cord. J Postgrad Med 2001;47:52-3. [PubMed]
- Rafeek N, Joseph LD, Rajendiran S, et al. Inflammatory myofibroblastic tumor of spermatic cord. Int J Surg Case Rep 2012;3:618-21. [Crossref] [PubMed]
- Shintaku M, Ukikusa M. Proliferative funiculitis with a prominent infiltration of mast cells. Pathol Int 2003;53:897-900. [Crossref] [PubMed]
- Hollowood K, Fletcher CD. Pseudosarcomatous myofibroblastic proliferations of the spermatic cord ("proliferative funiculitis"). Histologic and immunohistochemical analysis of a distinctive entity. Am J Surg Pathol 1992;16:448-54. [Crossref] [PubMed]
- Chakrabarti N, Shetty R. Inflammatory myofibroblastic sarcoma of the spermatic cord. Indian J Surg 2010;72:152-4. [Crossref] [PubMed]
- Fisher C. Myofibroblastic malignancies. Adv Anat Pathol 2004;11:190-201. [Crossref] [PubMed]
- Coffin CM, Watterson J, Priest JR, et al. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 1995;19:859-72. [Crossref] [PubMed]
- Yee CH, To KF, Hou SM, et al. Inflammatory myofibroblastic tumor of spermatic cord in undescended testis. Urology 2009;73:1423.e9-12. [Crossref] [PubMed]
- Michal M, Hes O, Kazakov DV. Mesothelial glandular structures within pseudosarcomatous proliferative funiculitis--a diagnostic pitfall: report of 17 cases. Int J Surg Pathol 2008;16:48-56. [Crossref] [PubMed]
- Coffin CM, Hornick JL, Fletcher CD. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol 2007;31:509-20. [Crossref] [PubMed]
- Patrick N, Iskander M, Brougham K, et al. A right inguinoscrotal swelling: the importance of histological analysis. BMJ Case Rep 2012;2012. pii: bcr2012006658.
- Takezawa K, Matsuoka Y, Takao T, et al. Myxofibrosarcoma of the spermatic cord: a case report. Nihon Hinyokika Gakkai Zasshi 2008;99:555-9. [Crossref] [PubMed]
- Ozkan B, Ozgüroğlu M, Ozkara H, et al. Adult paratesticular myxofibrosarcoma: report of a rare entity and review of the literature. Int Urol Nephrol 2006;38:5-7. [Crossref] [PubMed]
- Tearada H, Nagata M, Mugiya S, et al. High-grade myxofibrosarcoma presenting at the spermatic cord after radiotherapy for prostate cancer. BMJ Case Rep 2012;2012. pii: bcr0320126082.
- Tajima S, Koda K. Paratesticular dedifferentiated liposarcoma with prominent myxoid stroma: report of a case and review of the literature. Med Mol Morphol 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Kryvenko ON, Rosenberg AE, Jorda M, et al. Dedifferentiated liposarcoma of the spermatic cord: a series of 42 cases. Am J Surg Pathol 2015;39:1219-25. [Crossref] [PubMed]
- Sioletic S, Dal Cin P, Fletcher CD, et al. Well-differentiated and dedifferentiated liposarcomas with prominent myxoid stroma: analysis of 56 cases. Histopathology 2013;62:287-93. [Crossref] [PubMed]
- Stella M, Di Somma C, Solari N, et al. Primary osteosarcoma of the spermatic cord: case report and literature review. Anticancer Res 2007;27:1605-8. [PubMed]
- Beiswanger JC, Woodruff RD, Savage PD, et al. Primary osteosarcoma of the spermatic cord with synchronous bilateral renal cell carcinoma. Urology 1997;49:957-9. [Crossref] [PubMed]
- Spirtos G, Abdu RA, Schaub CR. Osteosarcoma of the spermatic cord. J Urol 1991;145:832-3. [PubMed]
- Ugidos L, Suárez A, Cubillo A, et al. Mixed paratesticular liposarcoma with osteosarcoma elements. Clin Transl Oncol 2010;12:148-9. [Crossref] [PubMed]
- Sano M, Takagi Y, Kimura M, et al. Malignant mesenchymoma in the scrotum. A case report. Nihon Hinyokika Gakkai Zasshi 1998;89:903-6. [Crossref] [PubMed]
- Fujita T, Akino H, Suzuki Y, et al. Malignant mesenchymoma of the spermatic cord: a case report. Hinyokika Kiyo 1994;40:165-8. [PubMed]
- Rodríguez D, Barrisford GW, Sanchez A, et al. Primary spermatic cord tumors: disease characteristics, prognostic factors, and treatment outcomes. Urol Oncol 2014;32:52.e19-25. [Crossref] [PubMed]
- Prabhu R, Natarajan A, Shenoy R, et al. Rhabdomyosarcoma of spermatic cord in a 65-year-old man presenting as a groin swelling. BMJ Case Rep 2013;2013. pii: bcr2013010499.
- Bouchikhi AA, Mellas S, Tazi MF, et al. Embryonic paratesticular rhabdomyosarcoma: a case report. J Med Case Rep 2013;7:93. [Crossref] [PubMed]
- Shimamoto K, Tanji N, Ozaw A, et al. Intrascrotal rhabdomyosarcoma in adult: a case report. Nihon Hinyokika Gakkai Zasshi 2009;100:545-9. [Crossref] [PubMed]
- Rodríguez García N, Llanes González L, Pascual Mateo C, et al. Spermatic cord rhabdomyosarcoma in an adult. Arch Esp Urol 2005;58:956-9. [Crossref] [PubMed]
- Marwah N, Marwah S, Gill M, et al. Adult paratesticular rhabdomyosarcoma presenting as acute intestinal obstruction-a case report. Indian J Surg 2013;75:143-4. [Crossref] [PubMed]
- Zamolo G, Coklo M, Stifter S, et al. Solid variant of alveolar rhabdomyosarcoma of the spermatic cord. Wien Klin Wochenschr 2005;117:323. [Crossref] [PubMed]
- Haga K, Kashiwagi A, Nagamori S, et al. Adult paratesticular rhabdomyosarcoma. Nat Clin Pract Urol 2005;2:398-402. [Crossref] [PubMed]
- Ozeki Z, Kobayashi S, Machida T, et al. Alveolar rhabdomyosarcoma originating in spermatic cord: a case report. Hinyokika Kiyo 2004;50:653-5. [PubMed]


