A review of penile elongation surgery
Penile anatomy
To fully understand limitations of small penis size and the surgical correction possibilities, we must review the relevant basic penile anatomy. The penis is composed of three large cylinders—two corpora cavernosa dorsally, which contain the erectile tissue, and the corpus spongiosum which constitutes the urethra. The main components of the penis are surrounded by areolar tissue and peripherally encased with skin. Each layer of the penis plays a significant role in the function and dynamics of the penis during sexual activity and voiding (1).
Skin plays an important role in protecting the penile tissues from trauma during intercourse and as a barrier from bacterial infection. If infection or trauma do occur, the skin can impair intracavernosal functioning and result in a contained abscess or hematoma formation, respectively. The skin is firmly attached to the glans and only loosely attached to the shaft, allowing for mobility during intercourse. Deep to the skin lies the superficial (dartos) and deep (Bucks’) fascia, which supply additional structural support (2). At the base of the penis, the dartos fascia combines with smooth muscle fibres and creates a well-defined penoscrotal angle between the scrotal wall and the skin. The deep fascia adheres to the tunica albuginea (1).
The base of the penis is firmly attached to the pubic rami by penile ligaments composed of connective tissue. The ligaments arise from the external oblique aponeurosis and are fixed to the symphysis pubis. The suspensory ligament arises from the linea alba and provides dorsal support and stabilization of an erection by attaching midline to the penile root (2). This ligament also helps cover the neurovascular bundle of the penis and protects it during repetitive sexual trauma. The ligament of Luschka or fungiform ligament consist of dartos fibers and extends from the abdominal Scarpa’s fascia onto the penile shaft. The fungiform ligament attaches to the pubis and fans laterally and ventrally to the encircle the entire penile root, acting like a sling for support (1).
Penis development/embryology
During embryologic development, gender remains indifferent until approximately seventh week of gestation. From the eighth week onward, male and female developmental pathways diverge. In males, maternal chorionic gonadotropins from the placenta stimulate growth and development of the testicular Leydig cells, which eventually produce their own testosterone for further development (3). The development of the external genitalia in males is dependent on the conversion of testosterone to the active component dihydrotestosterone (DHT). Testosterone is converted to DHT locally by 5 α-reductase and then directly acts on androgen receptors to initiate cell signaling pathways (3,4).
The genital tubercle enlarges to form both the shaft and glans of the penis. The urogenital folds fuse along the midline to become the penile urethra and the glans invaginates to create the glandular urethra. The labioscrotal folds fuse to create the scrotum. Complete penile differentiation should be complete by the end of the first trimester. Penile length and size increase during development in proportion to other fetal development (5). The average penile length increases by a mean of approximately 2 cm between 14 weeks and term. Penile elongation in utero is complete by androgens produced by the fetus. After the first trimester, the fetus depends on his own hypothalamic-pituitary axis for gonadotropin production. Any abnormality resulting in hypogonadism in utero can result in an underdeveloped penis, and therefore congenital or ‘true’ micropenis (5,6).
After normal development, there is an LH surge at birth which stimulates an increase in testosterone production and penile growth. This surge only lasts about 12 h and subsequently hormone levels drop quite low. Slowly, gonadotropin and androgen levels begin to rise and peak again. This rise in levels lasts for approximately 6 months and allows for continued penile growth (7). Ongoing penile growth occurs throughout development, without the need for surges, but rather as a result of normal growth. At puberty, the HPG axis gets activated and stimulates testicular testosterone production, which subsequently leads to further penile growth into adulthood (7,8).
Penile length
Normal penile length
Accurate measurement of penile length is important for both clinical and academic purposes. For this reason, a standard practice for measurement has been defined to maintain consistency. Rather than measuring a flaccid penis, which offers limited clinical significance, stretched penile length (SPL) measurement is considered best practice for adult men as it most closely replicates normal erect penile length (9). SPL is the maximum length of the penis while stretched, measured from the base of the penis, under the pubic symphysis to the tip of the glans and is thought to approximate erect penile length within 10% (10). For accurate clinical assessment, SPL needs to be measured by a clinician. Studies have demonstrated that men who are satisfied with their penile length overestimate their size, whereas men who are dissatisfied consistently underestimate (11).
Micropenis
True micropenis is defined as a normally formed penis that has an SPL that falls below two standard deviations of normal for a patient’s age and race (12). Wiygul outlined the mean SPL in children as well as the diagnostic length for micropenis at each age (13). Normal values for preterm infants born between the 24th and 36th week of gestation can be calculated using the formula: (0.16 × weeks of gestation) – 2.27 (14).
As mentioned, micropenis develops as a result of a central or local hormonal imbalance during fetal development. True micropenis is a congenital anomaly and is different from acquired penile length abnormalities such as buried penis or trapped penis. Based on the etiology of the hormonal dysfunction, micropenis can be divided into three broad categories: hypogonadotropic hypogonadism, hypergonadotropic hypogonadism, and idiopathic. Other, less common causes of micropenis have been documented and are listed in Table 1. Disorders of sexual differentiation may present with micropenis, although hypospadias is more common (13). The coexistence of micropenis and hypospadias is termed “microphallus” (1).
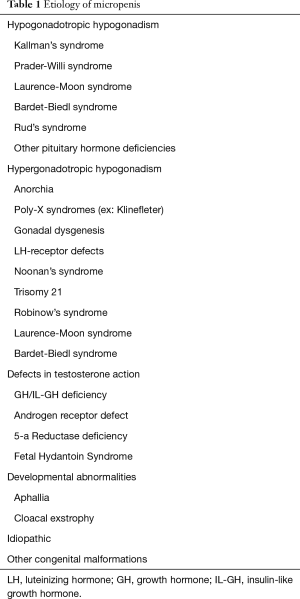
Full table
Penile dysmorphophobia
The majority of men seeking penile elongation treatment have a normal penile size, which is functionally adequate for sexual activity and micturition (14,15). Men complaining of small penis, despite adequate length, typically suffer from either penile dysmorphophobia disorder (PDD) or small penis anxiety (SPA). In both of these disorders, men consistently underestimate the size of their own penis and overestimate the mean size for other men (16). PDD lies within the body dysmorphic disorder (BDD) spectrum, which is defined in the Diagnostic and Statistical manual of Mental Disorder, Fifth edition as a ‘somatoform disorder presented by preoccupation with an imaginary or trivial flaw in the physical appearance that causes impairment in various areas of functioning’ (17). Men are so preoccupied with their penis size and length, they may develop depressive episodes associated with social, occupational, and sexual dysfunction. There is a high prevalence of psychogenic erectile dysfunction and lack of sexual satisfaction in men with BDD, despite their normal libido (11).
In comparison, SPA is an anxiety syndrome pertinent to the genital organs being observed, directly or indirectly while clothed, due to concern that the flaccid penis length and/or girth is less than the expected normal for an adult male. Patient anxiety persists despite evidence from a clinical examination to negate their concern (18). SPA may be an obsessive rumination or an aspect of psychosis which results in significant emotional distress and behavioral impairment (19). Multiple scales and nomograms have been created by researchers to reassure patients that their length is normal. Unfortunately, due to the nature of their anxieties, results of these studies are only minimally helpful to this patient population (9,20).
Non-surgical management
The idea of treating actual and perceived penile shortening with intervention is controversial. Most academic urologists have moved away from treatments such as penile elongation and therefore this has become strictly a market in the private sector (14). Wessells created guidelines for penile elongation in 1996, and not much has changed since. At that time, it was felt that only men with a flaccid length of less than 4 cm or a SPL of less than 7.5 cm should be considered candidates for penile lengthening (10). Nowadays, it is likely that men with normal penis size are undergoing interventions due to PDD or SPA. An ethical review on penile elongation procedures did report that after clearly hearing and understanding the risks and complications associated with each procedure, most men with a normal penis size will decline. All men undergoing penile elongation surgery with an SPL within normal limits, should undergo psychiatric evaluation (21).
Testosterone
In cases of true micropenis, the goal of treatment should be restoration of a functional penis size in order to improve body image and self-esteem, allow normal standing micturition and enable satisfying sexual intercourse. In children with true micropenis, the first step in management is always the least invasive, which includes the application of exogenous testosterone.
Multiple studies have explored intervention with testosterone replacement either early during development and/or at pubarche. If insufficient penile growth is not achieved with replacement, multiple courses of replacement can be considered without significant reduction in stature (22-24). In 2013, the beneficial effects of hormonal therapy on penile growth in children with micropenis was confirmed. In this study, prepubertal children were treated with 25 mg of exogenous parenteral testosterone enanthate once a month for 3 months, and pubertal or postpubertal children were treated with intramuscular hCG once a week for 6 weeks. Exogenous administration of hormone replacement in these boys resulted in a significant increase in SPL and suggests that these treatments could be the primary form of therapy for micropenis in paediatric patients (25). In addition to exogenous testosterone, topical applications have been studied in the micropenis population. Early studies revealed a 150% improvement in penile length with minimal side effects when DHT was applied locally (26).
The administration of exogenous testosterone in childhood does not compromise ultimate penile length increase in adulthood, however, the long-term effects of testosterone administration in childhood are still not fully understood and long-term data are needed (27). Although men on androgen deprivation therapy for prostate cancer have been observed to have a significant decline in penile length, there does not appear to be any beneficial effect in length with the use of testosterone in men without hypogonadal dysfunction (28). Further studies could be done to look at this potential application for local benefits in the aging population.
Traction devices
Penile traction devices (PTD) have been explored both as an independent strategy to help with penile elongation and as an augment to surgery. These devices cradle the penis and gently apply tension in attempt to stretch tissue and increase length. Multiple brands of these devices have been created and studied including: “FastSize”, and “Andro-Penis”. Prospective studies have looked at men complaining of a subjectively small penis. The duration of application of these devices has not been concluded, but usually ranges from 4–6 h per day (29,30). In one study, after 2 months, men were asked to leave the traction device on for 9 h per day (31). Compliance and patient selection is a significant issue given the time requirements for this minimally invasive treatment. Outcomes have been encouraging as patient satisfaction has unanimously improved after use for 3–6 months and flaccid or SPL has increased 1–3 cm in different studies (29-31). Oderda and Gontero conducted a review which aimed to explore whether nonsurgical methods of penile lengthening may have some scientific background. They concluded that penile extender devices seem to be non-inferior to surgery (32). Limitations of these studies included non-validated patient satisfaction questionnaires, small patient populations, and selection bias (14).
More recently traction devices are being studied for their pre-operative and post-operative use to augment outcomes from surgical procedures. Levine’s group has studied the use of traction devices in men with Peyronie’s disease and have shown improvement in patient satisfaction post-operatively after the use of PTD (33). Similarly, in early trials, pre-operative use of PTD has been shown to increase penile length prior to implantation of penile prosthesis and therefore allowing insertion of a larger caliber of cylinder (34). Although limited data exists, there appears to be a role for use of PTD both independently in men not interested in surgery, as well as an augment to other surgical procedures.
Surgical management
Penile augmentation
Different types of injectable materials have been used for penile augmentation including liquid silicone, polyacrylamide, hyaluronic acid and mineral-oil (35-37). However, there is a significant risk of foreign body reaction, swelling, penile distortion, granulomas and need for removal (36). Autologous fat grafting has been described to increase penile length and girth, which has no foreign body reaction as it is derived from the body’s own tissues. This is a much less invasive procedure compared to flap reconstruction or V-Y advancements. To obtain a fat graft, fat is liposuctioned from areas of excess, placed in 10 mL syringes and then centrifuged for 3 min at 300 g. The superior oil layer and lower aqueous layers are removed and the middle adipose layer is collected as the purified fat graft. The fat is transferred into smaller syringes for injected in multiple layers to improve fat graft survival. This technique has been refined by Sydney Coleman in recent years (38,39). The autologous fat graft will lose 20–80% of its volume over the first year of engraftment, and thus multiple procedures are sometimes necessary to achieve the desired result (40-42). Panfilov described his technique for penile augmentation with fat grafting in 88 patients. Incisions are made radially through the frenulum preputial and approximately 40–68 cc of fat is injected between the superficial penile fascia and the profunda, down to the root of the penis. The average length and circumference increase was 2.39 and 2.65 cm respectively, after 12 months (35). In one patient, the penis gained 3 cm in length at 6 months, but due to fat graft resorption, the stable length was 2 cm at 7 years. This technique can be combined with suspensory ligament release to further increase length. In Panfilov’s series approximately 1/3rd of patients had the ligament release in addition to autologous fat grafting. Unfortunately, it was not specified which patients had just the autologous fat grafting versus both procedures and the resulting gain in length. Penile augmentation with fat grafts also increase the weight of the penis, which can itself increase the length by 2–3 cm (35). Dermal fat grafting has also been described to increase girth and length of the penis, which may have better fat retention and decreased contour irregularities at the expense of a larger donor-site scar (37,43).
Suspensory ligament release
As discussed, the suspensory ligament anchors the penis to the pubic symphysis and while providing support, acts as the mobile point for the penis during erection. This attachment prevents the penis from moving further outward and creates an arched angle to the penile base (44). The suspensory ligament is composed of the suspensory ligament proper and the arcuate subpubic ligament that attaches the tunica albuginea to the midline of the pubic symphysis. Surgical release of this ligament changes the acute angle of the penis to the pubic symphysis to an obtuse angle which allows the penis to lie in a more dependant position and therefore gives the perception of lengthening (44). Division of the suspensory ligament, with or without bulking agent, fat pad excision or V-Y plasty is the most widely accepted surgical technique for penile elongation (45). The suspensory ligament can be accessed through a V-Y incision or a subcoronary circumcision technique (43). Complete release of the corpora from the pubic ramus has been described to further increase length, but is associated with significant risk to the neurovascular bundles of the penis, causing denervation and devascularisation of the penis (46).
Outcomes from suspensory ligament release have not consistently been favourable. Patient and partner satisfaction rates range from 30–65%. On average, the surgery increases flaccid penile length by 1–3 cm, especially with post-operative use of a PTD (45,47). Many patients in early studies had a recurrence following surgery, which resulted in penile shortening. Therefore, optimal surgical technique now involves placing a buffer in place of the ligament. Buffer options have included a vascularized flap from the lipomatous tissue of the spermatic cord or a small testicular prosthesis (45,48). Srinivas et al. have described the V-Y advancement with subsequent silicone sheath insertion between the pubis and the released suspensory ligament to prevent recurrence (49). After the inverted V-Y incision and suspensory ligament release, a silicone sheath from a penile prosthesis was inserted in the soft tissue defect created between the base of the penis and the symphysis pubis. They achieved a lengthening of 2.5 cm at 6 months, however, only one case is described with this short follow-up. Dermal fat grafts have also been described to fill this space (49).
Paradoxically, the main side effects of this procedure are recurrence, penile shortening, and the lack of penile support during erection, resulting difficulty with sexual intercourse and penetration (36). Poor satisfaction rates make this surgical technique not favourable for many patients.
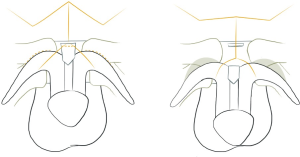
V-Y advancement
Penile elongation using a dorsal V-Y incision in the congenital or acquired short penis was first described over 40 years ago. A dorsal V-shaped incision was made, combined with partial detachment of the crura from the pubic ramis, which were then re-approximated in the midline and the dorsal incision was closed as a V-Y advancement flap. The V-Y incision and subsequent V-Y advancement is commonly used in conjunction with a suspensory ligament release. The incision is typically an upside down V, which is closed in an upside-down Y-shape, which lengthens the dorsal skin by bringing lateral tissue to the midline (Figure 1). The flap is distally based, and poor wound healing, flap dehiscence and distal flap loss can occur if the flaps blood supply is compromised during dissection (36). Bulging of the penoscrotal transition can also occur, which can be treated using bilateral Z-plasties (35). It is difficult to determine the average length achieved by V-Y advancement as it is typically combined with other procedures.

Suprapubic lipectomy
Suprapubic lipectomy has been performed to increase perceived penis length, particularly for patients with a buried penis. In these patients, weight loss does not always reduce the problem of a large overhanging fold, or mons pannus. These folds can cause problems with hygiene, directing the urine stream and sexual function (50). Removal of the skin and fat concealing the penis can be performed as a suprapubic lipectomy or limited panniculectomy. The skin is removed as a trapezoid incision. The inferior portion of the incision is marked 2 cm above the penis to allow closure of the base of the penis to the pubic symphysis periosteum, and the superior portion should not interfere with the waistline sulcus (50). This technique increases the exposed penile length. This can be combined with removal of diseased shaft skin, which may be inflammatory due to the buried condition and chronic infections. The shaft skin can be closed with a skin graft taken from the lateral thigh, or from the removed mons pubis skin to avoid a donor site (51). If there is need for further length, release of the suspensory ligament can be performed along with the suprapubic lipectomy (52). If the buried penis is secondary to cicatrix post circumcision, which is more common in children but can present in adults, either Z-plasties or removal of the entire penile skin with skin grafting and vacuum assisted closure with a negative pressure wound dressing can be performed. Suction lipectomy, or liposuction, is considered inadequate to treat a buried penis unless it is used in conjunction with suprapubic lipectomy (52). If no significant buried penis is present, but there is a moderate pubic fat pad, then liposuction may help to increase perceived penis length (53).
Sliding elongation
Sliding elongation has been described to lengthen the penis after significant penile shortening secondary to correction of Peyronie’s disease and severe therapy resistant erectile dysfunction (54,55). Some surgical treatments of Peyronie’s disease involve a plication on the contralateral side to correct penile curvature, which can lead to penile shortening of 3 cm or more. Rolle et al. first described this technique in three patients and gained on average 3.2 cm of penile length (54). Recently, Egydio and Kuehhas performed the sliding technique on 143 patients with severe therapy resistant erectile dysfunction with penile shortening with or without Peyronie’s disease to restore penis length and girth (55). The penis is degloved and the neurovascular bundle is mobilized. The corpus spongiosum is separated from the tunica albuginea and longitudinal incisions are made at the 3 and 9 o’clock positions, along with an incision proximal-dorsal and distal-ventral. After subtunical dissection, traction is applied to slide the distal penis away from the proximal shaft to perform the lengthening, the limit of which is the length of the urethra and neurovascular bundles (55) (Figure 2). A prosthesis is then inserted into the tunical defects that are created by this technique. The authors report an average penile lengthening of 3.1 cm and a 54% resolution of penile curvature in those that had Peyronie’s disease pre-operatively (55). The same group previously described this method of lengthening the penis with similar tunica incisions and subsequent pericardial grafting of the resulting tunical defect after lengthening, but felt that the grafting was time consuming and unnecessary (56). Rolle et al. performed a prospective study of the sliding elongation technique in 28 patients with Peyronie’s disease, and had an average 3.2 cm penile lengthening with no curvature recurrence at an average follow-up of 37 months (57).

Penile disassembly
Perovic and Djordjevic describe a technique similar to sliding elongation, which they have used to treat short penises and congenital penile anomalies. Their procedure involves separating the penis into the glans cap with neurovascular bundle dorsally, the corpora cavernosa, and the urethra ventrally. Thus, the corpora are separated completely from the surrounding structures. A space is created between the glans cap and the tip of the corpora cavernosa, on which an autologous rib cartilage graft is placed, and then the penis is reassembled (58) (Figure 3). The cartilage is covered with the glans cap and the urethra and neurovascular bundles are sutured to the tunica. This technique was performed on 19 patients with a short penis with an average increased length of 2–3 cm and 3–4 cm in 13 and 6 patients, respectively (58). There was no evidence of cartilage extrusion, erectile dysfunction or urethral damage at a mean follow-up of 3.3 years.

Flap reconstruction
Local, regional and free flap options exist to lengthen the penis. These have typically been described for penile lengthening if the penis is shortened due to epispadias and exstrophy, where a lack of soft tissue and dorsal skin or tethering of the penis to the pubic bone from fibrous bands (46). Kramer and Jackson describe the use of local rhomboid flaps, based laterally, for dorsal skin coverage combined with partial release of the corpora cavernosa from the pubic ramus in 10 patients. These local flaps are necessary due to the lack of dorsal coverage once the corpora are released from the penis and advanced through an inverted V-shaped incision (Figure 4). This technique is described for both congenital and acquired short penis. They state that most patients obtained a doubling in their penile length. Other local flap options are lateral superiorly based scrotal flaps that are rotated onto the dorsal penis (59). Dorsal Z and W-plasties may also be performed as local skin flaps, but may bring hair bearing skin onto the penis (36).
Conclusions
Men complaining of short penis need to be clinically assessed for evidence of true micropenis and screened for PDD. Patients should first be treated conservatively with testosterone therapy, PTD, and a psychiatric assessment if applicable. There are no current guidelines on the best surgical management for men requesting penile elongation. Multiple surgical techniques have been developed each with their own limitations and have been reviewed above. Further work in this field is required to devise the optimal surgical procedure with the smallest complication profile and the highest patient satisfaction.
Acknowledgements
The authors would like to thank Alison Wong, MD for preparing the diagrams to supplement the surgical descriptions within this manuscript. The authors would also like to thank Dr. Gerald Brock, MD for his support in preparing this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cimador M, Catalano P, Ortolano R, et al. The inconspicuous penis in children. Nat Rev Urol 2015;12:205-15. [Crossref] [PubMed]
- Kureel SN, Gupta A, Sunil K, et al. Surgical anatomy of the penis in hypospadias: magnetic resonance imaging study of the tissue planes, vessels, and collaterals. Urology 2015;85:1173-8. [Crossref] [PubMed]
- Johnson P, Maxwell D. Fetal penile length. Ultrasound Obstet Gynecol 2000;15:308-10. [Crossref] [PubMed]
- Zalel Y, Pinhas-Hamiel O, Lipitz S, et al. The development of the fetal penis--an in utero sonographic evaluation. Ultrasound Obstet Gynecol 2001;17:129-31. [Crossref] [PubMed]
- Hughes IA. The testes: disorders of sexual differentiation and puberty in the male. In: Sperling MA. editor. Pediatric Endocrinology. 3rd edition. Philadelphia, PA: Saunders; 2008; 662-85.
- Kousta E, Papathanasiou A, Skordis N. Sex determination and disorders of sex development according to the revised nomenclature and classification in 46,XX individuals. Hormones (Athens) 2010;9:218-131. [Crossref] [PubMed]
- Achermann JC, Hughes IA. Endocrinology of fetal development. In: Melmed S, Polonsky K, Larsen PR, et al. editors. Williams Textbook of Endocrinology. 12th edition. Philadelphia, PA: Sounders, 2011; 868-934.
- Grumbach MM. A window of opportunity: the diagnosis of gonadotropin deficiency in the male infant. J Clin Endocrinol Metab 2005;90:3122-7. [Crossref] [PubMed]
- Veale D, Miles S, Bramley S, et al. Am I normal? A systematic review and construction of nomograms for flaccid and erect penis length and circumference in up to 15,521 men. BJU Int 2015;115:978-86. [Crossref] [PubMed]
- Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol 1996;156:995-7. [Crossref] [PubMed]
- Veale D, Miles S, Read J, et al. Sexual Functioning and Behavior of Men with Body Dysmorphic Disorder Concerning Penis Size Compared with Men Anxious about Penis Size and with Controls: A Cohort Study. Sex Med 2015;3:147-55. [Crossref] [PubMed]
- Aaronson IA. Micropenis: medical and surgical implications. J Urol 1994;152:4-14. [PubMed]
- Wiygul J, Palmer LS. Micropenis. ScientificWorldJournal 2011;11:1462-9. [Crossref] [PubMed]
- Ghanem H, Glina S, Assalian P, et al. Position paper: Management of men complaining of a small penis despite an actually normal size. J Sex Med 2013;10:294-303. [Crossref] [PubMed]
- Mondaini N, Ponchietti R, Gontero P, et al. Penile length is normal in most men seeking penile lengthening procedures. Int J Impot Res 2002;14:283-6. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
- Veale D, Miles S, Read J, et al. Relationship between self-discrepancy and worries about penis size in men with body dysmorphic disorder. Body Image 2016;17:48-56. [Crossref] [PubMed]
- Wylie KR, Eardley I. Penile size and the 'small penis syndrome'. BJU Int 2007;99:1449-55. [Crossref] [PubMed]
- Fox C. Sizing up the man: how important is penis size to men? Sexologies 2006;15:S1, S30
- Veale D, Miles S, Read J, et al. Penile Dysmorphic Disorder: Development of a Screening Scale. Arch Sex Behav 2015;44:2311-21. [Crossref] [PubMed]
- Vardi Y. Is penile enlargement an ethical procedure for patients with a normal-sized penis? Eur Urol 2006;49:609-11. [Crossref] [PubMed]
- Bin-Abbas B, Conte FA, Grumbach MM, et al. Congenital hypogonadotropic hypogonadism and micropenis: effect of testosterone treatment on adult penile size why sex reversal is not indicated. J Pediatr 1999;134:579-83. [Crossref] [PubMed]
- Burstein S, Grumbach MM, Kaplan SL. Early determination of androgen-responsiveness is important in the management of microphallus. Lancet 1979;2:983-6. [Crossref] [PubMed]
- Choi SK, Han SW, Kim DH, et al. Transdermal dihydrotestosterone therapy and its effects on patients with microphallus. J Urol 1993;150:657-60. [PubMed]
- Nerli RB, Guntaka AK, Patne PB, et al. Penile growth in response to hormone treatment in children with micropenis. Indian J Urol 2013;29:288-91. [Crossref] [PubMed]
- Ben-Galim E, Hillman RE, Weldon VV. Topically applied testosterone and phallic growth. Its effects in male children with hypopituitarism and microphallus. Am J Dis Child 1980;134:296-8. [Crossref] [PubMed]
- Sutherland RS, Kogan BA, Baskin LS, et al. The effect of prepubertal androgen exposure on adult penile length. J Urol 1996;156:783-7; discussion 787. [Crossref] [PubMed]
- Park KK, Lee SH, Chung BH. The effects of long-term androgen deprivation therapy on penile length in patients with prostate cancer: a single-center, prospective, open-label, observational study. J Sex Med 2011;8:3214-9. [Crossref] [PubMed]
- Gontero P, Di Marco M, Giubilei G, et al. A pilot phase-II prospective study to test the 'efficacy' and tolerability of a penile-extender device in the treatment of 'short penis'. BJU Int 2009;103:793-7. [Crossref] [PubMed]
- Levine LA, Newell MM. FastSize Medical Extender for the treatment of Peyronie's disease. Expert Rev Med Devices 2008;5:305-10. [Crossref] [PubMed]
- Nikoobakht M, Shahnazari A, Rezaeidanesh M, et al. Effect of penile-extender device in increasing penile size in men with shortened penis: preliminary results. J Sex Med 2011;8:3188-92. [Crossref] [PubMed]
- Oderda M, Gontero P. Non-invasive methods of penile lengthening: fact or fiction? BJU Int 2011;107:1278-82. [Crossref] [PubMed]
- Levine LA, Newell M, Taylor FL. Penile traction therapy for treatment of Peyronie's disease: a single-center pilot study. J Sex Med 2008;5:1468-73. [Crossref] [PubMed]
- Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. [Crossref] [PubMed]
- Panfilov DE. Augmentative phalloplasty. Aesthetic Plast Surg 2006;30:183-97. [Crossref] [PubMed]
- Vardi Y, Har-Shai Y, Gil T, et al. A critical analysis of penile enhancement procedures for patients with normal penile size: surgical techniques, success, and complications. Eur Urol 2008;54:1042-50. [Crossref] [PubMed]
- Xu L, Zhao M, Yang Z, et al. Modified Penile Augmentation by Dermal-Fat Graft in Post-Hypospadias Adults. Aesthetic Plast Surg 2016;40:120-9. [Crossref] [PubMed]
- Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg 1997;24:347-67. [PubMed]
- Coleman SR. Hand rejuvenation with structural fat grafting. Plast Reconstr Surg 2002;110:1731-44; discussion 1745-7.
- Gir P, Oni G, Brown SA, et al. Human adipose stem cells: current clinical applications. Plast Reconstr Surg 2012;129:1277-90. [Crossref] [PubMed]
- Locke MB, de Chalain TM. Current practice in autologous fat transplantation: suggested clinical guidelines based on a review of recent literature. Ann Plast Surg 2008;60:98-102. [Crossref] [PubMed]
- Smith P, Adams WP Jr, Lipschitz AH, et al. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg 2006;117:1836-44. [Crossref] [PubMed]
- Mertziotis N, Kozyrakis D, Bogris E. Is V-Y plasty necessary for penile lengthening? Girth enhancement and increased length solely through circumcision: description of a novel technique. Asian J Androl 2013;15:819-23. [Crossref] [PubMed]
- Hoznek A, Rahmouni A, Abbou C, et al. The suspensory ligament of the penis: an anatomic and radiologic description. Surg Radiol Anat 1998;20:413-7. [Crossref] [PubMed]
- Li CY, Kayes O, Kell PD, et al. Penile suspensory ligament division for penile augmentation: indications and results. Eur Urol 2006;49:729-33. [Crossref] [PubMed]
- Kramer SA, Jackson IT. Bilateral rhomboid flaps for reconstruction of the external genitalia in epispadias-exstrophy. Plast Reconstr Surg 1986;77:621-31. [Crossref] [PubMed]
- Protogerou V, Anagnostopolou S, Venierates D, et al. Penis ligaments: their use in "increasing" the size of the penis in penile augmentation procedures. Anatomical description in human cadavers and clinical results of a phalloplasty series. Ann Ital Chir 2010;81:199-204. [PubMed]
- Alter GJ, Jordan GH. Penile elongation and girth enhancement. AUA Update Series 2007;26:229-37.
- Srinivas BV, Vasan SS, Mohammed S. Penile lengthening procedure with V-Y advancement flap and an interposing silicone sheath: A novel methodology. Indian J Urol 2012;28:340-2. [Crossref] [PubMed]
- Figler BD, Chery L, Friedrich JB, et al. Limited Panniculectomy for Adult Buried Penis Repair. Plast Reconstr Surg 2015;136:1090-2. [Crossref] [PubMed]
- Lorca-García C, Pérez-García A. Limited Panniculectomy for Adult Buried Penis Repair. Plast Reconstr Surg 2016;137:1065e. [Crossref] [PubMed]
- Pestana IA, Greenfield JM, Walsh M, et al. Management of "buried" penis in adulthood: an overview. Plast Reconstr Surg 2009;124:1186-95. [Crossref] [PubMed]
- Alter GJ, Salgado CJ, Chim H. Aesthetic surgery of the male genitalia. Semin Plast Surg 2011;25:189-95. [Crossref] [PubMed]
- Rolle L, Ceruti C, Timpano M, et al. A new, innovative, lengthening surgical procedure for Peyronie's disease by penile prosthesis implantation with double dorsal-ventral patch graft: the "sliding technique". J Sex Med 2012;9:2389-95. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified 'sliding' technique. BJU Int 2015;116:965-72. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE, Sansalone S. Penile length and girth restoration in severe Peyronie's disease using circular and longitudinal grafting. BJU Int 2013;111:E213-9. [Crossref] [PubMed]
- Rolle L, Falcone M, Ceruti C, et al. A prospective multicentric international study on the surgical outcomes and patients' satisfaction rates of the 'sliding' technique for end-stage Peyronie's disease with severe shortening of the penis and erectile dysfunction. BJU Int 2016;117:814-20. [Crossref] [PubMed]
- Perovic SV, Djordjevic ML. Penile lengthening. BJU Int 2000;86:1028-33. [Crossref] [PubMed]
- Xiao K, Cheng K, Song N. A new surgical procedure for phallic reconstruction in partial penis necrosis: penile elongation in combination with glanuloplasty. Ann Plast Surg 2014;72:638-42. [Crossref] [PubMed]


