Erectile dysfunction, masculinity, and psychosocial outcomes: a review of the experiences of men after prostate cancer treatment
Introduction
Globally, over one million new cases of prostate cancer (PC) were diagnosed in 2012 with incidence expected to increase to 1.7 million cases in 2030 (1,2). PC incidence is highest in western countries such as Australia/New Zealand, North America, and Europe (age standardised incidence rates per 100,000 range from 85.0 to 111.6) (1,2). Parallel to increasing incidence, survival has also increased in the UK, North America and Australia/New Zealand such that approximately 90% of men now survive their PC 5 or more years and over 80% survive at least 10 years (3-5). Although promising, extended survival means that many men live with high and enduring treatment side-effects that can persist for a decade or more (6,7). For instance, treatments such as surgery, radiation therapy, and androgen deprivation therapy (ADT) can have negative effects on urinary, bowel, hormonal, or sexual function (8,9). Regarding the latter, erectile dysfunction (ED) is the most common impact on sexual function and is often accompanied by a loss of sexual desire or difficulty reaching orgasm (10).
The exact incidence of ED following PC therapy is unknown with most epidemiological data derived from the post-radical prostatectomy (RP) cohort. While the exact recovery of erectile function is difficult to compare when reviewing clinical studies due to variables such as the definition of ED, the definition of return of erectile function, the use of erectogenic medication and the use of multimodal PC therapy, it is widely accepted that post-RP ED occurs for around 60–70% of men (11-15) despite advances in surgical techniques and technology. Factors such as the age of the patient, the level of pre-treatment erectile function, the extent of surgical neurovascular preservation, intraoperative changes on erectile haemodynamics, stage of disease and body mass index can contribute to the erectile outcome (13,15,16). In contrast to post-RP ED, radiation-induced ED usually develops later (usually 3-year post-radiation) with the actual rates of ED between RP and radiation groups similar (17). Several pathophysiological mechanisms for ED have been proposed that include cavernous nerve injury, vascular compromise (e.g., accessory pudendal artery ligation), damage to nearby structures, local inflammatory changes relating to surgical and radiation effects, cavernosal smooth muscle hypoxia with ensuing smooth muscle apoptosis and fibrosis, as well as corporal veno-occlusive dysfunction causing venous leakage (11-15).
In addition to physical treatment side-effects, for some men ED has quality of life (QoL) and psychosocial impacts including but not limited to depression, cancer-specific distress, self-esteem, relationship satisfaction, coping and adjustment (18-21). Masculinity (i.e., men’s identity or sense of themselves as being a man) may also be linked to how men respond to PC diagnosis and treatment including their experience of psychological and psychosexual distress and adjustment (22-28). Low masculine self-esteem has been shown to contribute to increased anxiety, depression and cancer-specific distress in men with PC (29). Masculinity has also been implicated in men’s reluctance to seek help for their emotional or sexual concerns after PC treatment (24,30,31). However, the exact nature of the impact of ED on psychosocial aspects of men’s experience after PC treatment and how masculinity may feed into this is unclear (20,32).
Thus, the aim of this review is to provide a snapshot of the current state of the evidence regarding ED, masculinity and psychosocial impacts after PC treatment. Our review considers three questions:
- How is masculinity described in the literature in relation to ED after PC treatment?
- Does masculinity moderate the effects of ED on men’s psychosocial or QoL outcomes after PC treatment?
- Is masculinity considered as a state of being that is affected by ED (i.e., masculinity is an outcome) after PC treatment?
Methods
Search strategy
The search strategy occurred in a two-step process. First, Medline and PsycINFO [via Ovid), CINAHL, and EMBASE databases were searched (January 1st, 1980 to January 31st, 2016] using the following keywords:
- (“prostat$ cancer” OR “prostat$ neoplasm$” OR “prostat$ carcinoma”);
- (masculine OR masculinity OR masculinities OR manhood OR man-hood OR “sex role” OR “sex-role” OR “male identity” OR “male identities” OR “gender identity” OR “gender identities” OR “sexual identity” OR “sexual identities”);
- 1 AND 2;
- 3 limit to Human AND English.
Second, targeted searches on Google Scholar were conducted with the terms “prostate cancer” AND (masculinity OR masculine OR hegemonic). Duplicates were removed prior to examining article titles and abstracts. Cited reference searches of articles which met final inclusion criteria for review were conducted on Web of Science, Google Scholar, and via hand searches of article reference lists. For retrieval and eligibility of articles and data extraction, one author and a research assistant independently completed each stage and consulted with a third independent reviewer to resolve differences in decision-making.
Eligibility criteria
Potential articles were identified initially by examining the title and abstract and were then retrieved for more detailed evaluation against the apriori inclusion criteria. Peer-reviewed quantitative or qualitative journal articles containing primary data were included if they met the pre-determined eligibility criteria below:
- Participants were men (or a sub-group of men) who had been diagnosed with and received treatment for any stage of PC;
- Included a measure of ED or sexual function/dysfunction;
- Included a measure of masculinity in quantitative studies or masculinity emerged as a key theme in qualitative studies;
- Included masculinity or psychosocial (e.g., distress, social support, adjustment) or QoL outcome(s);
- Published in English language;
- Published after January 1st, 1980 and prior to January 31st, 2016.
Reviews, meta-analyses, editorials, commentaries, books or book chapters, guidelines, position statements, conference proceedings, abstracts and dissertations were excluded.
Data extraction
A data extraction form was created prior to the review to identify key characteristics of studies which met criteria for inclusion: source (author, year and country of publication); study design; participants (age, sexual orientation, disease stage, treatment type, time since treatment, ED score); masculinity measure; results corresponding to masculinity outcomes and masculinity as a contributor to (correlate) or moderator of psychosocial or QoL outcomes. Characteristics of included studies are summarised in Tables S1,S2.
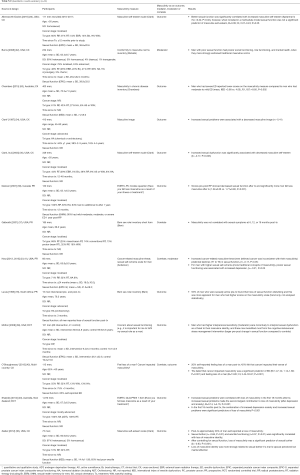
Full table

Full table
Results
Search results
Systematic search
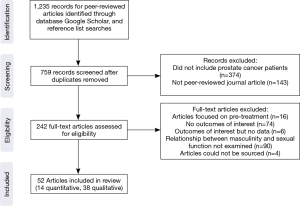
The systematic search identified 759 records for review after duplicates were removed. Of these, 242 underwent full-text review. One hundred and ninety articles were excluded because they focused on pre-treatment decision-making, had no outcomes of interest, or the relationship between masculinity and sexual function was not examined (Figure 1). The remaining 52 articles were reviewed and these included 14 quantitative and 38 qualitative studies. Quantitative research comprised 7 studies that were cross-sectional, 5 prospective, and 2 randomised controlled trials (RCT). Qualitative research included 35 cross-sectional and 3 prospective studies. Studies were published from 1995 to 2016 and most were conducted in the USA (39%), Australia (23%), Canada (14%), Europe (10%), or the UK (8%).
Sample characteristics
Sample sizes ranged from 3 to 1,070 (median =20); 68% of studies had less than 50 participants. Twenty-four studies provided a mean age for men and this ranged from 57.0 to 76.2 years. Most studies did not report the sexual orientation of the sample (65%) and where this did occur almost all sampled exclusively heterosexual men (33%); only one study focused on the experience of homosexual men (33). Of the 26 studies reporting disease stage, most men had localised PC (69%) and were treated with RP (45% of studies included mostly men receiving RP, 23% radiation therapy, and 23% hormonal ablation therapy; 9% of studies did not report treatment type). Less than half (45%) of studies reviewed reported time since treatment and this ranged from 0 to 60 months. Nine studies (17%) reported ED scores from validated measures and of these most used the sexual function subscale from the Expanded Prostate cancer Index Composite.
Masculinity measures
Measures most often used to assess masculinity in quantitative studies were the masculine self-esteem scale (33-36), Bem Sex-Role Inventory (37,38), or the single item EORTC-QLQ-PR25 measure (‘Have you felt less masculine as a result of your illness or treatment?’) (39,40). Other measures used in a single study were the Sexual Self-Schema scale for Men (41), the Conformity to Masculine Norms Inventory (22), Cancer-related Masculine Threat scale (23), and the Masculinity in Chronic Disease Inventory (32). Two studies used un-validated measures (38,42).
Masculinity and sexual function after PC treatment
PC treatment and subsequent ED, loss of libido, and/or potency was consistently described in qualitative studies as having an impact on, or being a threat to, men’s sense of masculinity (43-50). Some men chose to undergo radiation therapy instead of RP because the former offered a better chance of preserving sexual function which in their view was equivalent to masculinity (51,52). In almost every study, the belief that masculinity was lost (‘no longer a man’) or somehow diminished (‘not a whole man’) was described (26,43,44,48,52-71), and this was a source of anxiety, depression, or embarrassment for men; made them question their self-worth; and created feelings of disempowerment and a fear that they may be stigmatised (27,43-46,49,60,61,70,72-74).
Other qualitative studies described masculinity as framing men’s experiences and adjustment after PC treatment (54). In this regard, due to their sexual dysfunction some men believed that they could no longer live a normal life (63) or respond appropriately in everyday interactions with women (72,73). Men also discussed the possibility that their wives would leave them because they could not satisfy them sexually or be an ‘active partner’ (66,70,75). Men limited social activities which had the potential for sex (e.g., parties) (61,67); adopted strategies that maintained the macho façade such as pseudo courtship or laughing at jokes about ED (66,67); or used traditional (hegemonic) masculine coping responses such as emotional restraint (60), stoicism (60,76), acceptance (66,76), optimism (27,67,69), and humour (47).
Many qualitative studies discussed that men rationalised their ED or sexual dysfunction through active attempts to cognitively reframe their experience which in turn allowed them to preserve their sexual identity or sense of masculinity. Men did this in four main ways: used age as a reference point to normalise or accept their experience (ED is an inevitable consequence of aging, ED is worse for younger men) (26,28,43-46,54,60,61,63,66,67,70); viewed ED or sexual dysfunction as a trade-off for prolonged life or health (health more important, small price to pay for being alive) (26,27,43,47,58,60,63,65-67,77); broadened their definition of sex as encompassing more than an erection and penetration (e.g., hugging, kissing, conversation and company) (27,44-46,60,61,63,66,67,75); and looked for other evidence of masculinity (e.g., already had children, sowed a lot of wild oats, being grateful for prior sexual experiences) (27,60,66).
In contrast to the majority of qualitative work, a small number of studies which sampled older men reported that changes in men’s sexual function had minimal impact on masculinity (28,44-46,76). The potential impact of ED on masculinity was also discussed in studies sampling men from a range of ages as something that happened to other men (43,63); ED was viewed as an ill-effect that men could live with (44-46); or ED had minimal impact because men or their partners had already experienced sexual dysfunction due to chronic or co-morbid disease (66,75).
Masculinity as a moderator
Two quantitative studies examined masculinity as a moderator of the relationship between sexual function and psychosocial or QoL outcomes. Together these studies showed that when men who had poor sexual functioning endorsed more traditional (hegemonic) masculine values they had worse social functioning, role functioning, and mental health outcomes (22), including depression (41).
Masculinity as an outcome or correlate
In the remaining 12 quantitative studies, masculinity was described as an outcome (32-36,38-40,42,78), or as a potential correlate or predictor of sexual function or bother (23,36,37,42). Collectively, these studies showed a consistent correlational relationship between poor sexual function and decreased masculinity (32,34-36,39,40,42,78), or increased masculinity and poorer sexual outcomes (23,36,42). However, this relationship did not hold in two studies when sexual function was included with other variables in a multivariate model as predictors of masculinity (33) or when the impact of masculinity on sexual symptoms at different points on the treatment trajectory were considered (37).
Of these quantitative studies, two also described the conditions under which the relationship between sexual function and masculinity may be strengthened (moderated) by interpersonal variables (36,38). Specifically, men who had sexual dysfunction or bother were more likely to interpret this as a threat to their masculinity if they had higher interpersonal sensitivity which can diminish social support and communication (38), or their spouse perceived low marital affection (36).
Discussion
Based on this review it is clear that for most men masculinity is crucial in their experience of PC treatment and ED in two ways: masculinity frames how men interpret what is happening to them; and men’s sense of themselves and their masculinity suffers harm. While there is evidence that some men manage to cope with this impact and are able to cognitively reframe their experience relative to aging, prolonged life, the definition of sex, and other evidence of their virility or sexual prowess, this is a task that for many men will be challenging. Therefore, the role of clinicians and health practitioners in the field is to help men and their partners broaden their perceptions of sexual relationships and also to facilitate adjustment by assisting men to make meaning of, or seek alternative meaning for, their experience that presents less of a threat to their masculine identity.
While the proliferation of qualitative research in this context offers some key insights, this work has focused on understanding the masculinity phenomena. There are few quantitative studies and of these most confirm a correlational relationship between ED and masculinity and, with few exceptions, do not extend beyond this. Moving forward, three areas of focus for future research are apparent. First, we need empirical studies that establish the role of masculinity as a mediator or moderator of psychosocial and QoL outcomes for men experiencing sexual dysfunction. Two studies in this review (22,41) suggest a moderation effect for masculinity; men who had ED and more strongly endorsed traditional masculine values experienced poorer QoL and mental health outcomes. However, recent work on men’s decisions to seek medical help for their sexual concerns after PC treatment suggests that aspects of masculinity such as emotional self-reliance and placing high value on the importance of sex may be a strength for men to draw upon in promoting help-seeking and ultimately better adjustment (30). The conditions under which masculinity may be a help or a hindrance to PC patient’s adjustment require further exploration.
Second, for men experiencing ED after PC treatment, empirical studies are needed to identify factors that may interact with masculinity with regards to its influence on QoL or psychosocial outcomes, and determine their relative importance. Two studies in this review (36,38) reported that interpersonal factors such as marital affection may moderate the extent to which men interpret ED as a threat to their masculinity. However, there are a range of individual (e.g., age, sexual orientation), psychological (e.g., depression, anxiety, pre-treatment expectations), social (e.g., nature and quality of relationships, support) and medical (e.g., co-morbidities, medication use, pre-treatment erectile function, other treatment side-effects, treatment type) factors that may also be important and these have yet to be explored fully.
Third, to facilitate knowledge advancement about the role and contribution of masculinity, established theory and consistent measurement approaches should be adopted. This review noted a trend toward use of masculinity measures that reflect traditional, hegemonic masculine values and ideals (e.g., Bem Sex Role Inventory, Conformity to Masculine Norms Inventory, Sexual Self-Schema scale for Men) that are not contextualised for men with cancer. Where context-specific scales have been applied, they are ambiguous, single-item measures (e.g., EORTC-QLQ-PR25 question) or capture only one aspect of masculinity (e.g., Masculine Self-Esteem scale). Recent development of two context-specific masculinity scales, the Cancer-related Masculine Threat scale (23) and the Masculinity in Chronic Disease Inventory (32) show promise, however more research is needed to establish the utility of these scales across the diversity of men who have ED after PC treatment, particularly accounting for sexual orientation, ethnic background, and treatment type.
Given the role of masculinity as an influencer of men’s response to ED after PC treatment, our challenge going forward is to develop interventions that are responsive to masculinity, optimally working with masculinity as a potential strength. To do this we need to better unpack masculinity as it relates to ED and PC treatment through context-specific measurement of masculinity; quantitative empirical, prospective studies that consider the experience of men with differing sexual orientations, socio-demographic backgrounds, and PC treatments; assess moderating and mediating factors; and test interventions for ED that incorporate masculinity in a holistic way. In the interim, it is important for clinicians to invite a conversation with men and their partners about their expectations and goals with regards to sexual outcomes after a PC diagnosis and treatment and implement a care plan matched to these. In addition, given the links between a man’s sexual QoL and his psychological outcomes, this care plan needs to also address psychosocial and subjective well-being based on current best practice approaches (79).
Acknowledgements
SK Chambers is supported by an Australian Research Council Future Fellowship. Acknowledgement to Lisa Nielsen, Liz Eldridge and Kirstyn Laurie for research assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Center MM, Jemal A, Lortet-Tieulent J, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol 2012;61:1079-92. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.1, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available online: http://globocan.iarc.fr, accessed on 14/11/2015.
- American Cancer Society. Survival rates for prostate cancer. Retrieved 6th November, 2015. Available online: http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-survival-rates
- Australian Institute of Health and Welfare (AIHW). Prostate cancer in Australia. Cancer series no. 79. Retrieved 3rd November, 2015. Available online: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129545133
- Cancer Research UK. Prostate cancer statistics: prostate cancer survival. Retrieved 3rd November, 2015. Available online: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer#heading-Two
- Bernat JK, Wittman DA, Hawley ST, et al. Symptom burden and information needs in prostate cancer survivors: a case for tailored long-term survivorship care. BJU Int 2016;118:372-8. [Crossref] [PubMed]
- Carlsson S, Drevin L, Loeb S, et al. Population-based study of long-term functional outcomes after prostate cancer treatment. BJU Int 2016;117:E36-45. [Crossref] [PubMed]
- Canalichio K, Jaber Y, Wang R. Surgery and hormonal treatment for prostate cancer and sexual function. Transl Androl Urol 2015;4:103-9. [PubMed]
- Watson E, Shinkins B, Frith E, et al. Symptoms, unmet needs, psychological well-being and health status in survivors of prostate cancer: implications for redesigning follow-up. BJU Int 2016;117:E10-9. [Crossref] [PubMed]
- Schover LR, Fouladi RT, Warneke CL, et al. Defining sexual outcomes after treatment for localized prostate carcinoma. Cancer 2002;95:1773-85. [Crossref] [PubMed]
- Chung E, Brock G. Sexual rehabilitation and cancer survivorship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med 2013;10:102-11. [Crossref] [PubMed]
- Chung E, Gillman M. Prostate cancer survivorship: a review of current literature in erectile dysfunction and the concept of penile rehabilitation following prostate cancer therapy. Med J Aust 2014;200:582-5. [Crossref] [PubMed]
- Salonia A, Burnett AL, Graefen M, et al. Prevention and management of postprostatectomy sexual dysfunctions part 1: Choosing the right patient at the right time for the right surgery. Eur Urol 2012;62:261-72. [Crossref] [PubMed]
- Salonia A, Burnett AL, Graefen M, et al. Prevention and management of postprostatectomy sexual dysfunctions part 2: Recovery and preservation of erectile function, sexual desire, and orgasmic function. Eur Urol 2012;62:273-86. [Crossref] [PubMed]
- Tal R, Alphs HH, Krebs P, et al. Erectile function recovery rate after radical prostatectomy: a meta-analysis. J Sex Med 2009;6:2538-46. [Crossref] [PubMed]
- Alemozaffar M, Regan MM, Cooperberg MR, et al. Prediction of erectile function following treatment for prostate cancer. JAMA 2011;306:1205-14. [Crossref] [PubMed]
- Potosky AL, Davis WW, Hoffman RM, et al. Five-year outcomes after radical prostatectomy or radiotherapy for prostate cancer: The prostate cancer outcomes study. J Natl Cancer Inst 2004;96:1358-67. [Crossref] [PubMed]
- Goonewardene SS, Persad R. Psychosexual care in prostate cancer survivorship: a systematic review. Transl Androl Urol 2015;4:413-20. [PubMed]
- Helgason AR, Adolfsson J, Dickman P, et al. Waning sexual function--the most important disease-specific distress for patients with prostate cancer. Br J Cancer 1996;73:1417-21. [Crossref] [PubMed]
- McCabe MP, Althof SE. A systematic review of the psychosocial outcomes associated with erectile dysfunction: does the impact of erectile dysfunction extend beyond a man’s inability to have sex? J Sex Med 2014;11:347-63. [Crossref] [PubMed]
- Weber BA, Sherwill-Navarro P. Psychosocial consequences of prostate cancer: 30 years of research. Geriatric Nursing 2005;26:166-75. [Crossref] [PubMed]
- Burns SM, Mahalik JR. Sexual functioning as a moderator of the relationship between masculinity and men’s adjustment following treatment for prostate cancer. Am J Mens Health 2008;2:6-16. [Crossref] [PubMed]
- Hoyt MA, Stanton AL, Irwin MR, et al. Cancer-related masculine threat, emotional approach coping, and physical functioning following treatment for prostate cancer. Health Psychol 2013;32:66. [Crossref] [PubMed]
- Wall D, Kristjanson L. Men, culture and hegemonic masculinity: understanding the experience of prostate cancer. Nurs Inq 2005;12:87-97. [Crossref] [PubMed]
- Wittmann D, Northouse L, Foley S, et al. The psychosocial aspects of sexual recovery after prostate cancer treatment. Int J Impot Res 2009;21:99-106. [Crossref] [PubMed]
- Chapple A, Ziebland S. Prostate cancer: embodied experience and perceptions of masculinity. Sociology of Health & Illness 2002;24:820-41. [Crossref]
- Oliffe J. Constructions of masculinity following prostatectomy-induced impotence. Soc Sci Med 2005;60:2249-59. [Crossref] [PubMed]
- Oliffe J. Embodied masculinity and androgen deprivation therapy. Sociol Health Illn 2006;28:410-32. [Crossref] [PubMed]
- Chambers SK, Schover L, Nielsen L, et al. Couple distress after localised prostate cancer. Support Care Cancer 2013;21:2967-76. [Crossref] [PubMed]
- Hyde MK, Zajdlewicz L, Wootten AC, et al. Medical help-seeking for sexual concerns in prostate cancer survivors. Sex Med 2016;4:e7-e17. [Crossref] [PubMed]
- Oliffe J. Positioning prostate cancer as the problematic third testicle. In: Broom A, Tovey P. editors. Men’s health: Body, identity and social context. London: Wiley Ltd.; 2009:33-62.
- Chambers SK, Hyde MK, Oliffe JL, et al. Measuring masculinity in the context of chronic disease. Psychology of Men & Masculinity 2016;17:228-42. [Crossref]
- Allensworth-Davies D, Talcott JA, Heeren T, et al. The health effects of masculine self-esteem following treatment for localized prostate cancer among gay men. LGBT Health 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Clark JA, Wray N, Brody B, et al. Dimensions of quality of life expressed by men treated for metastatic prostate cancer. Soc Sci Med 1997;45:1299-309. [Crossref] [PubMed]
- Clark JA, Inui TS, Silliman RA, et al. Patients' perceptions of quality of life after treatment for early prostate cancer. J Clin Oncol 2003;21:3777-84. [Crossref] [PubMed]
- Zaider T, Manne S, Nelson C, Mulhall J, Kissane D. Loss of masculine identity, marital affection, and sexual bother in men with localized prostate cancer. J Sex Med 2012;9:2724-32. [Crossref] [PubMed]
- Galbraith ME, Ramirez JM, Pedro LW. Quality of life, health outcomes, and identity for patients with prostate cancer in five different treatment groups. Oncol Nurs Forum 2001;28:551-60. [PubMed]
- Molton IR, Siegel SD, Penedo FJ, et al. Promoting recovery of sexual functioning after radical prostatectomy with group-based stress management: the role of interpersonal sensitivity. J Psychosom Res 2008;64:527-36. [Crossref] [PubMed]
- Davison BJ, So AI, Goldenberg SL. Quality of life, sexual function and decisional regret at 1 year after surgical treatment for localized prostate cancer. BJU Int 2007;100:780-5. [Crossref] [PubMed]
- Sharpley CF, Birsika V, Denham JW. Factors associated with feelings of loss of masculinity in men with prostate cancer in the RADAR trial. Psychooncology 2014;23:524-30. [Crossref] [PubMed]
- Hoyt MA, Carpenter KM. Sexual self-schema and depressive symptoms after prostate cancer. Psychooncology 2015;24:395-401. [Crossref] [PubMed]
- O'Shaughnessy PK, Ireland C, Pelentsov L, et al. Impaired sexual function and prostate cancer: a mixed method investigation into the experiences of men and their partners. J Clin Nurs 2013;22:3492-502. [Crossref] [PubMed]
- Appleton L, Wyatt D, Perkins E, et al. The impact of prostate cancer on men's everyday life. Eur J Cancer Care (Engl) 2015;24:71-84. [Crossref] [PubMed]
- Arrington MI. "I don't want to be an artificial man": Narrative reconstruction of sexuality among prostate cancer survivors. Sexuality and Culture 2003;7:30-58. [Crossref]
- Arrington MI. Theorizing about social support and health communication in a prostate cancer support group. J Psychosoc Oncol 2010;28:260-8. [Crossref] [PubMed]
- Arrington MI. Uncertainty and stigma in the experiences of prostate cancer survivors: A thematic analysis of narrative elements. Illness, Crisis, & Loss 2015;23:242-60. [Crossref]
- Hagen B, Grant-Kalischuk R, Sanders J. Disappearing floors and second chances: men's journeys of prostate cancer. Int J Mens Health 2007;6:201-23. [Crossref]
- Lavery JF, Clarke VA. Prostate cancer: patients' and spouses' coping and marital adjustment. Psychology, Health & Medicine 1999;4:289-302. [Crossref]
- Rivers BM, August EM, Gwede CK, et al. Psychosocial issues related to sexual functioning among African-American prostate cancer survivors and their spouses. Psychooncology 2011;20:106-10. [Crossref] [PubMed]
- Wittmann D, Carolan M, Given B, et al. What couples say about their recovery of sexual intimacy after prostatectomy: Toward the development of a conceptual model of couples' sexual recovery after surgery for prostate cancer. J Sex Med 2015;12:494-504. [Crossref] [PubMed]
- Arrington MI. Prostate cancer and the social construction of masculine sexual identity. Int J Mens Health 2008;7:299-306. [Crossref]
- Broom A. Prostate cancer and masculinity in Australian society: a case of stolen identity? Int J Mens Health 2004;3:73-91. [Crossref]
- Chambers SK, Lowe A, Hyde MK, et al. Defining young in the context of prostate cancer. Am J Mens Health 2015;9:103-14. [Crossref] [PubMed]
- Berterö C. Altered sexual patterns after treatment for prostate cancer. Cancer Practice 2001;9:245-51. [Crossref] [PubMed]
- de Moraes Lopes MH, Higa R, et al. Life experiences of Brazilian men with urinary incontinence and erectile dysfunction following radical prostatectomy. J Wound Ostomy Continence Nurs 2012;39:90-4. [Crossref] [PubMed]
- Dieperink KB, Wagner L, Hansen S, et al. Embracing life after prostate cancer. A male perspective on treatment and rehabilitation. Eur J Cancer Care (Engl) 2013;22:549-58. [Crossref] [PubMed]
- Ervik B, Nordøy T, Asplund K. Hit by waves---living with local advanced or localized prostate cancer treated with endocrine therapy or under active surveillance. Cancer Nursing 2010;33:382-9. [Crossref] [PubMed]
- Ervik B, Asplund K. Dealing with a troublesome body: a qualitative interview study of men's experiences living with prostate cancer treated with endocrine therapy. Eur J Oncol Nurs 2012;16:103-8. [Crossref] [PubMed]
- Evans J, Butler L, Etowa J, et al. Gendered and cultured relations: exploring African Nova Scotians' perceptions and experiences of breast and prostate cancer. Res Theory Nurs Pract 2005;19:257-73. [Crossref] [PubMed]
- Fergus KD, Gray RE, Fitch MI. Sexual dysfunction and the preservation of manhood: experiences of men with prostate cancer. J Health Psychol 2002;7:303-16. [Crossref] [PubMed]
- Gannon K, Guerro-Blanco M, Patel A, et al. Re-constructing masculinity following radical prostatectomy for prostate cancer. Aging Male 2010;13:258-64. [Crossref] [PubMed]
- Gilbert E, Ussher JM, Perz J. Embodying sexual subjectivity after cancer: a qualitative study of people with cancer and intimate partners. Psychol Health 2013;28:603-19. [Crossref] [PubMed]
- Hamilton K, Chambers SK, Legg M, et al. Sexuality and exercise in men undergoing androgen deprivation therapy for prostate cancer. Support Care Cancer 2015;23:133-42. [Crossref] [PubMed]
- Harden J, Schafenacker A, Northouse L, et al. Couples' experiences with prostate cancer: focus group research. Oncol Nurs Forum 2002;29:701-9. [Crossref] [PubMed]
- Klaeson K, Sandell K, Bertero CM. Sexuality in the context of prostate cancer narratives. Qual Health Res 2012;22:1184-94. [Crossref] [PubMed]
- Maliski SL, Rivera S, Connor S, et al. Renegotiating masculine identity after prostate cancer treatment. Qual Health Res 2008;18:1609-20. [Crossref] [PubMed]
- Navon L, Morag A. Advanced prostate cancer patients' ways of coping with the hormonal therapy's effect on body, sexuality, and spousal ties. Qual Health Res 2003;13:1378-92. [Crossref] [PubMed]
- O'Brien R, Hart GJ, Hunt K. "Standing out from the herd": men renegotiating masculinity in relation to their experience of illness. Int J Mens Health 2007;6:178-200. [Crossref]
- Phillips C, Gray RE, Fitch MI, et al. Early postsurgery experience of prostate cancer patients and spouses. Cancer Practice 2000;8:165-71. [Crossref] [PubMed]
- Powel LL, Clark JA. The value of the marginalia as an adjunct to structured questionnaires: experiences of men after prostate cancer surgery. Qual Life Res 2005;14:827-35. [Crossref] [PubMed]
- Seidler ZE, Lawsin CR, Hoyt MA, et al. Let's talk about sex after cancer: exploring barriers and facilitators to sexual communication in male cancer survivors. Psychooncology 2016;25:670-6. [Crossref] [PubMed]
- Bokhour BG, Clark JA, Inui TS, et al. Sexuality after treatment for early prostate cancer: exploring the meanings of "erectile dysfunction". J Gen Intern Med 2001;16:649-55. [Crossref] [PubMed]
- Clark JA, Bokhour BG, Inui TS, et al. Measuring patients' perceptions of the outcomes of treatment for early prostate cancer. Med Care 2003;41:923-36. [Crossref] [PubMed]
- Martin E, Bulsara C, Battaglini C, et al. Breast and prostate cancer survivor responses to group exercise and supportive group psychotherapy. J Psychosoc Oncol 2015;33:620-34. [Crossref] [PubMed]
- Gray RE, Fitch MI, Fergus KD, et al. Hegemonic masculinity and the experience of prostate cancer: a narrative approach. Journal of Aging & Identity 2002;7:43-62. [Crossref]
- Letts C, Tamlyn K, Byers ES. Exploring the impact of prostate cancer on men's sexual well-being. J Psychosoc Oncol 2010;28:490-510. [Crossref] [PubMed]
- Ng C, Kristjanson LJ, Medigovich K. Hormone ablation for the treatment of prostate cancer: the lived experience. Urologic Nursing 2006;26:204-12. [PubMed]
- Lucas MD, Strijdom SC, Berk M, et al. Quality of life, sexual functioning and sex role identity after surgical orchidectomy in patients with prostatic cancer. Scand J Urol Nephrol 1995;29:497-500. [Crossref] [PubMed]
- Chambers SK, Dunn J, Lazenby M, et al. ProsCare: a psychological care model for men with prostate cancer. Available online: http://www.prostate.org.au/media/195765/proscare_monograph_final_2013.pdf