Emphysematous pyelonephritis: the impact of urolithiasis on disease severity
Introduction
Emphysematous pyelonephritis is a rare manifestation of a severe upper urinary tract infection marked by gas in the renal parenchyma and/or collecting system. The condition was first described by Kelly and Maccallum in 1898, who noted an association between glycosuria and pneumaturia in the absence of urological instrumentation (1). Further studies have confirmed >90% of patients with emphysematous pyelonephritis have diabetes mellitus (2). Historically the mortality rate has been as high as 71% with medical management alone and 33% if treated with emergent nephrectomy (3,4). Despite advances in antibiotic coverage, imaging, and treatment options, mortality rates have remained high (25% in recent series) (5). Although urolithiasis has been identified in 22% of patient with emphysematous pyelonephritis, the relationship between urolithiasis and disease severity has not been thoroughly investigated (2). In this study, we review the clinical characteristics, risk factors, treatments, and outcomes of patients diagnosed with emphysematous pyelonephritis in two hospitals in the United States between 2003 and 2014 with emphasis on the impact of concomitant urolithiasis.
Methods
After institutional review board approval, a search of all imaging reports from 2003 to 2014 was performed at The University of California San Francisco (UCSF) and San Francisco General Hospital. Imaging reports were queried for all studies containing the words “emphysematous” and “pyelonephritis”. Cases were excluded if there was recent urological manipulation or evidence of urinary fistula. Cases were included if there was evidence of gas in the collecting system, renal parenchyma, and/or the perinephric/paranephric space as well as a clinical diagnosis of pyelonephritis. Patient charts were reviewed and clinical data were abstracted. Clinical variables including age, gender, affected side, duration of symptoms, presence of fever, median length of hospitalization, symptoms, and medical comorbidities were recorded. Laboratory studies, microbiology data, and antibiotic therapy were also evaluated. Imaging studies were reviewed—computerized tomography (CT) had been performed on all patients. The CT scan was interpreted according to the imaging classification established by Huang et al. in which type I emphysematous pyelonephritis is confined to the collecting system, type II is confined to the renal parenchyma, type IIIa extends to the perirenal spaces and type IIIb extends to the pararenal space. Type IV is bilateral emphysematous pyelonephritis (6). The presence or absence of urolithiasis and/or hydronephrosis was also noted. All patients were treated initially with fluid resuscitation and antibiotic therapy. Patients who underwent ureteral stent placement did so in the operating room under general anesthesia with fluoroscopic guidance. Patients who underwent a nephrostomy tube placement did so either with CT guidance or a combination of ultrasound and fluoroscopic guidance with the interventional radiology department. Outcomes of each treatment modality were noted.
Descriptive statistics were calculated using the median for all continuous variables and percentages for all categorical variables. Difference between means of continuous variables was analyzed using two-tailed t-test. Categorical variables were analyzed utilizing the Fisher Exact test. All statistical analysis was performed in the R environment, version 3.0.1.
Results
A total of 14 cases were identified, 9 from UCSF and 5 from San Francisco General Hospital. Demographic and clinical data are summarized in Table 1. The median age was 49 and 11 (79%) patients were female. There were an equal number of left and right sided cases. The median duration of symptoms prior to presentation was 7 days. The most common comorbidity was a history of prior urinary tract infection (71%) followed by diabetes mellitus (57%) and hypertension (43%). The most common presenting symptoms were abdominal pain (50%), fever (36%) and flank pain (21%). A total of 4 patients (29%) had altered mental status and 3 patients (21%) had hypotension at some point during the hospitalization. A total of 8 patients (57%) had concomitant urolithiasis. Median length of hospital stay was 10 days [0–42]. Imaging of the majority of patients (57%) was consistent with Huang Class 1 (gas confined to the collecting system). Three patients had gas in the renal parenchyma (Huang class II) and three patients had gas extending past the renal parenchyma (Huang class III).
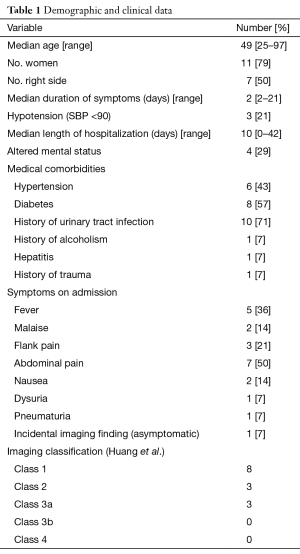
Full table
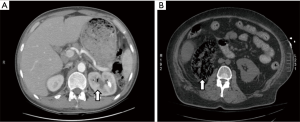
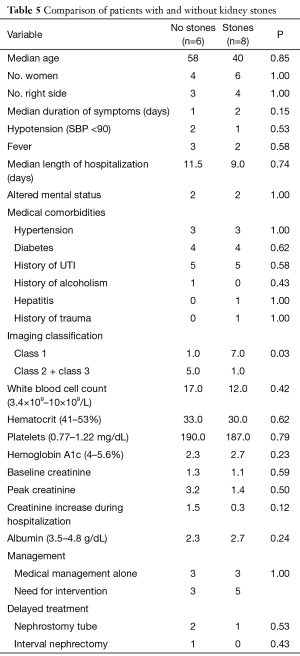
Laboratory data are summarized in Table 2. Median WBC count was 13. The median baseline creatinine was 1.1 and median creatinine increase during hospitalization was 0.5. Microbiology information is summarized in Table 3. Nine patients (64%) had a positive urine culture from a single organism; the remainder had mixed urine cultures. E-coli was the most common organism identified (50%) followed by Klebsiella (21%) and Candida (14%). The most common class of antibiotic therapy was fluoroquinolones (36%) followed by 3rd generation cephalosporins (29%) and extended spectrum penicillin (14%). Antibiotic coverage was changed at least twice in 50% of the patients. Seven patients (50%) were managed with antibiotic therapy alone (Table 4). Five patients (36%) required percutaneous drainage, and of these patients, two patients required placement of a second percutaneous nephrostomy tube due to incomplete drainage with the initial percutaneous drain. Only one patient required an interval nephrectomy. No patients required immediate nephrectomy. There were no deaths in our cohort. When the outcomes of patients with stones (Figure 1A) were compared to outcomes of patients without stones (Figure 1B), emphysematous pyelonephritis with gas confined to the collecting system (Huang class 1) was significantly more common in patients with stones than in patients without stones (P=0.03) (Table 5).
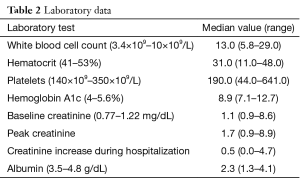
Full table
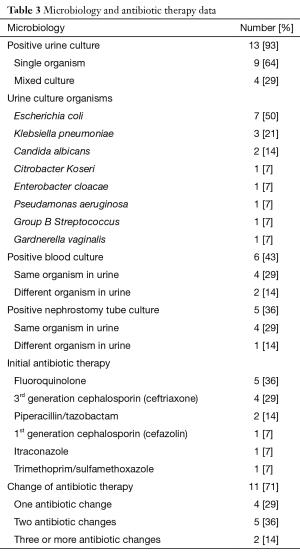
Full table
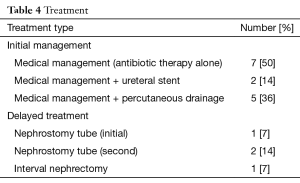
Full table
Full table
Discussion
Emphysematous pyelonephritis is a rare and severe infection of the kidney in which gas is produced in the renal collecting system and/or parenchyma. Since the initial description, dozens of case reports and more than 20 series have been published with >400 patients in total (7-10). The majority of studies were performed in Asia, India, and Africa; our sample is the largest from the USA.
The diagnosis of emphysematous pyelonephritis is made on imaging studies in which gas is detected within or around the kidney. Emphysematous pyelonephritis may be diagnosed with abdominal X-ray, ultrasonography or CT, although CT is now considered the definitive imaging modality given a 30% rate of non-detection diagnosis on plain abdominal X-ray and ultrasonography. Multiple imaging classifications have been developed. The imaging classification used in this study was developed by Huang et al. based on CT scan findings and has been found to be predictive for mortality in a study by Tsu et al. (11). The majority of patients in this series (57%) had emphysematous pyelonephritis confined to the collecting system (Huang class 1), and only 3 patients (21%) detected gas extending beyond the kidney (Huang class 3). Compared with other studies, our cohort has a higher percentage of patients with gas limited to the collecting system (11,12). There were no deaths and no patient required permanent dialysis, which may be related to detection at an earlier stage in the disease process given high utilization of CT scans in the USA (13,14).
The culture results are consistent with other studies of emphysematous pyelonephritis with the most common organisms isolated being E-coli and Klebsiella. Unlike early studies, the most common antibiotics used as initial therapy were fluoroquinolones, although it should be noted that the majority of patients (71%) changed antibiotics at least once and 50% of patient changed antibiotics two more times. In most cases, the patient received one dose of intravenous antibiotics in the Emergency Department, and a different intravenous antibiotic was administered once the patient was admitted to the hospital/intensive care unit. Once, the urine culture and sensitivity results returned, a change to another intravenous antibiotic was occasionally required. Oral antibiotics were started once the patient was afebrile and hemodynamically stable.
Comorbid conditions and presenting symptoms most commonly associated with emphysematous pyelonephritis are similar to those reported in other series with a few exceptions (11). Our series reports a much lower associated rate of diabetes mellitus (57%)—most large series report rates of >90% (5). Our associated rate of urolithiasis (57%) was higher than reported in the literature (22%) (2). When patients without stones and those with stones were compared, it was noted that those with stones had significantly lower classification of disease based on initial imaging. Patients with stones tended to be younger than those without stones and had less of an increase in creatinine during their hospitalization. Emphysematous pyelonephritis associated with urolithiasis is likely the result of bacterial activity in or associated with the stones rather than within the renal parenchyma, leading to a less aggressive form of the disease.
Treatment of emphysematous pyelonephritis has long been controversial. Spangola et al. reviewed all reported cases from varied locations around the world from 1898 to 1978 (total 31 patients) prior to the availability of routine CT, routine utilization of percutaneous nephrostomy drainage and double J stents, and contemporary antibiotic therapy. He found patients who underwent immediate nephrectomy had a lower mortality rate (33%) than patients undergoing medical management alone (71%) (3). Percutaneous drainage in the setting of emphysematous pyelonephritis was introduced by Hudson in 1986 and was subsequently found to be an effective initial form of treatment (10,15). Authors of other studies have advocated for early diagnosis and aggressive medical management (12,16). Based on the results from our contemporary series, medical management alone appears to be the best initial option for stable patients with relatively limited disease (Huang class I). For patients with more extensive disease on imaging or hemodynamic instability, double J stents and/or percutaneous renal drainage provided optimal drainage of the source of the infection. In some cases more than one percutaneous drain was necessary. No patients in this study required immediate nephrectomy and only one patient required subsequent nephrectomy due to a minimally functional kidney and a potential nidus for subsequent infection.
This study is limited by a small sample size and retrospective design. Also, the study relied on queries of radiology reports for identification of emphysematous pyelonephritis cases; it is possible cases may have been missed if the correct terminology was not included in radiology reports.
Conclusions
Emphysematous pyelonephritis is a severe infection associated with a high mortality rate. The lack of mortality in this study is associated with relatively limited disease severity in our cohort. Antibiotics alone were successfully utilized in the majority of patients; percutaneous renal drainage and/or double J stents were successful in controlling the source of infection in patients with more advanced disease. No patients required emergent nephrectomy. Emphysematous pyelonephritis with concomitant urolithiasis was associated with less extensive disease, suggesting these patients may have a unique mechanism for gas production causing a less aggressive form of the disease.
Acknowledgements
We would like to thank Gabriela E. M. Beug for assistance with manuscript editing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by IRB of CHR at UCSF (No. 14-14533).
References
- Kelly HA, Maccallum WG. Pneumaturia. JAMA 1898;31:375-81. [Crossref]
- Somani BK, Nabi G, Thorpe P, et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol 2008;179:1844-9. [Crossref] [PubMed]
- Spagnola AM. Emphysematous pyelonephritis. A report of two cases. Am J Med 1978;64:840-4. [Crossref] [PubMed]
- Michaeli J, Mogle P, Perlberg S, et al. Emphysematous pyelonephritis. J Urol 1984;131:203-8. [PubMed]
- Falagas ME, Alexiou VG, Giannopoulou KP, et al. Risk factors for mortality in patients with emphysematous pyelonephritis: a meta-analysis. J Urol 2007;178:880-5. [Crossref] [PubMed]
- Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 2000;160:797-805. [Crossref] [PubMed]
- Wan YL, Lee TY, Bullard MJ, et al. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome. Radiology 1996;198:433-8. [Crossref] [PubMed]
- Chen MT, Huang CN, Chou YH, et al. Percutaneous drainage in the treatment of emphysematous pyelonephritis: 10-year experience. J Urol 1997;157:1569-73. [Crossref] [PubMed]
- Chan PH, Kho VK, Lai SK, et al. Treatment of emphysematous pyelonephritis with broad-spectrum antibacterials and percutaneous renal drainage: an analysis of 10 patients. J Chin Med Assoc 2005;68:29-32. [Crossref] [PubMed]
- Lin WR, Chen M, Hsu JM, et al. Emphysematous pyelonephritis: patient characteristics and management approach. Urol Int 2014;93:29-33. [PubMed]
- Tsu JH, Chan CK, Chu RW, et al. Emphysematous pyelonephritis: an 8-year retrospective review across four acute hospitals. Asian J Surg 2013;36:121-5. [Crossref] [PubMed]
- Lin YC, Lin YC, Lin HD, et al. Risk factors of renal failure and severe complications in patients with emphysematous pyelonephritis-a single-center 15-year experience. Am J Med Sci 2012;343:186-91. [Crossref] [PubMed]
- Kocher KE, Meurer WJ, Fazel R, et al. National trends in use of computed tomography in the emergency department. Ann Emerg Med 2011;58:452-62.e3. [Crossref] [PubMed]
- Zhou JC, Zheng SW, Yu YX, et al. Trends in computed tomography utilization and association with hospital outcomes in a Chinese emergency department. PLoS One 2012;7:e40403. [Crossref] [PubMed]
- Hudson MA, Weyman PJ, van der Vliet AH, et al. Emphysematous pyelonephritis: successful management by percutaneous drainage. J Urol 1986;136:884-6. [PubMed]
- Kolla PK, Madhav D, Reddy S, et al. Clinical profile and outcome of conservatively managed emphysematous pyelonephritis. ISRN Urol 2012;2012:931982.


