The drug treatment of premature ejaculation
Introduction
International society of sexual medicine (ISSM) published the guideline for premature ejaculation (PE) in 2010 and updated it on 2014. The managements recommended for both acquired PE (APE) and lifelong PE (LPE) are almost same, such as a behavioral/psychotherapy, a pharmacotherapy and combination of these treatments (1). For the pharmacotherapy for PE, gold standard is selective serotonin reuptake inhibitors (SSRIs) including dapoxetine or paroxetine. For some patients, topical therapy with local anesthetics including Lidocaine/Prilocaine might be effective (1).
Off-label SSRIs and tricyclic antidepressants (TCAs)
There is a high level evidence to support the efficacy and safety of off-label daily dosing of the SSRIs and a serotonergic TCA: paroxetine (2), sertraline (3), citalopram (4), fluoxetine (5), and a serotonergic tricyclic, clomipramine (6,7). And as the off-label on-demand dosing, clomipramine (8) and paroxetine (2) are used for the treatment of LPE and APE. A meta-analysis showed that paroxetine was the strongest among several SSRIs in delaying ejaculation, showing 1,492% IELT increase from baseline (9). Delaying ejaculation effect appears from 5 to 10 days after drug administration; however, the maximum effect will take 2–3 weeks of treatment (10).
Adverse effects are mild and not long over two weeks, including mild nausea, diarrhea, fatigue, yawning, or perspiration (11). Systematic analysis of randomized clinical trials (RCT) of SSRIs in patients with depression suggests that youth but not adults have a small risk of suicidal ideation or suicide attempts (12,13). Physicians should be careful, when they prescribe SSRIs to young PE patients aged 18 years or younger and to those with PE and a suicidal ideation (14). Rapid dose reduction or sudden cessation of daily dosed SSRIs should be avoided, which may be associated with an SSRI withdrawal syndrome (15). As the other possible adverse effect, SSRI might affect sperm motility, therefore men who concern their fertility should not take SSRIs (16).
On-demand administration of off-label SSRIs 3–6 hours prior to intercourse is modestly efficacious and well tolerated (8). However On-demand usage of off-label SSRIs is associated with a less effectiveness in delaying ejaculation than daily treatment (2,8,17). Therefore, on-demand off-label SSRIs may be combined with low-dose daily treatment (2). So far, on-demand dosing of dapoxetine seems to be effective and safe; however in unavailable countries with dapoxetine, daily dose of off-label SSRIs (especially paroxetine) seems to be the most effective. In some countries, the government authorities might not allow the off-label prescription of SSRIs. This complicates PE treatment in countries where there is no approved medication and the regulatory authorities advise against off-label prescription.
Dapoxetine
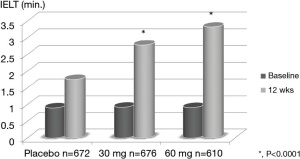
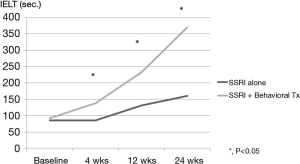
Dapoxetine has been approved for treating PE in over 50 countries. It has a pharmacokinetic profile supporting a role as an on-demand treatment for PE, rapid-acting and short half-life (18-20). Pryor et al. reported the first RCT for dapoxetine (dapoxetine 30 or 60 mg taken 1–2 hours before intercourse) with placebo, which shows significant improvement in dapoxetine group and dose dependency (Figure 1) (18). Dapoxetine is similarly effective both in men with LPE and APE (20-22). Moreover, it is well tolerated in men with PE and comorbid erectile dysfunction (ED) treated with phosphodiesterase type 5 inhibitors (PDE5i) (23). Cormio et al. reported the importance of behavioral management as the combination with dapoxetine, which clearly showed significant improvement in the combination with behavioral treatment group (Figure 2) (24). Adverse-events in on-demand usage of dapoxetine were uncommon, including dizziness, nausea, diarrhea, and headache (18,23). They led to the study discontinuation only in 4% (30 mg) and 10% (60 mg) of subjects.
Topical anesthetics
The use of topical anesthetics to reduce the sensitivity of the glans penis is probably the oldest known form of treating PE (1). There is a high evidence to support the efficacy and safety of off-label on-demand topical anesthetics in the treatment of LPE (1). The use of topical anesthetics such as lidocaine and/or prilocaine as a cream, a gel, or a spray is well established and is moderately effective in delaying ejaculation (25-28). Diminishing the glans sensitivity is thought to inhibit the spinal reflex arc responsible for ejaculation (29). Dinsmore et al. reported that PSD502, a lidocaine-prilocaine spray, which is applied to glans penis 5 minutes before sexual intercourse, showed a 6.3-fold increase in IELT (25). However, topical anesthetics are related with significant penile hypoanesthesia and possible transvaginal absorption, resulting in vaginal numbness and resultant female anorgasmia unless a condom is used (27).
PDE5i
PDE5is are effective treatments for ED, and some authors have suggested that PDE5is alone or in combination with SSRIs as a treatment for PE (30-33). Systematic reviews of multiple studies suggested the supportive role of PDE5i in men with PE and comorbid ED (34,35). The treatment of LPE with PDE5i in men with “normal” erectile function is not recommended and further evidence-based research is encouraged to understand conflicting data (11). Recently Sun et al. reported the meta-analysis of PDE5i for PE with concomitant ED, which showed a significant improvement with PDE5i alone compared with both of placebo and SSRI alone (36). It also suggested that the combination of PDE5i with SSRI showed a clear improvement compared with SSRI alone in PE with ED patients. However, PDE5i use showed the relatively significant increase of adverse event compared with placebo; moreover, combination with SSRI showed an increase of adverse event compared with SSRI alone (36).
Tramadol
Tramadol has been investigated as a potential off-label therapy for PE, with several studies demonstrating efficacy improving IELTs with varying doses of daily or on-demand tramadol therapy (11). Although the mechanism of action is not completely understood, the efficacy of tramadol may be secondary to anti-nociceptive and anesthetic-like effects, as well as via central nervous system modulation through inhibitions of serotonin and noradrenaline reuptake (37,38). Recent meta-analysis showed the efficacy of tramadol for PE, showing the significant improvement in several settings such as compared with placebo, paroxetine daily and on demand, PDE5i, topical anesthetics, and a behavioral management (39). Tramadol may be an effective option for the treatment of PE. However, the risk of addiction should be noted. It should not be combined with an SSRI because of the risk of serotonin syndrome, a potentially fatal outcome (40). Further well-controlled studies are required to assess the efficacy and safety of tramadol.
Alpha-1 adrenoceptor antagonist (alpha-1 blocker)
Recently Lee et al. reported that PE in Korean policemen is associated with ED and lower urinary tract symptoms (LUTS) including prostatic disease, which might be the important disease background for the PE (41). Alpha-1 adrenoceptor antagonist (alpha-1 blocker) is widely accepted as the first-line treatment for LUTS caused by benign prostatic hyperplasia. One of adverse events of alpha-1 blocker is ejaculatory disorder, and we previously demonstrated that alpha-1A blocker, tamsulosin, showed significant decrease of seminal emission compared with alpha-1A/D blocker, naftopidil (42).
For the treatment of PE, Beretta reported the first study with non-selective alpha-blocker, which showed that IELT in PE patients was significantly increased after phenoxybenzamine administration (43). Selective alpha-1 blocker, terazosin, showed the significant improvement of PE compared with placebo, in the patients’ reported outcome (44).
Hsieh et al. reported that alpha-1 blockers (phenoxybenzamine, prazosin, WB-4101, chloroethylclomidine and yohimbine) all inhibit the contractile response of the rat seminal vesicle to electrical nerve stimulation. As phenoxybenzamine is effective in treating PE, the comparable in vivo potencies of WB-4101 (alpha-1A blocker) and yohimbine (alpha-2 blocker) strongly suggest that they have clinical therapeutic potential for PE (45). In our study, although the volunteers with naftopidil (high affinity with alpha-1D as well as alpha-1A) showed no decrease of ejaculatory volume, those with tamsulosin (high affinity with alpha-1A) showed significant ejaculatory volume decrease (42). This study clearly showed that the mechanism of ejaculatory disorder induced by alpha-1 blocker is the relaxation of seminal tract including seminal vesicle and ejaculatory through subtype A of alpha-1 adrenoceptor. Therefore, subtype A of alpha-1 adrenoceptor plays an important role in an ejaculatory event evoked by sympathetic nerve stimulation. Another recent publication also showed the efficacy of tamsulosin for PE in the patients with LUTS and PE (46).
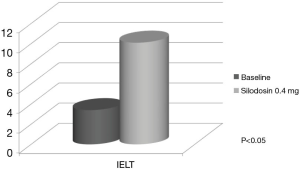
Silodosin is a new alpha-1 blocker that has more powerful affinity with the alpha-1A adrenoceptor. In another study, we demonstrated that silodosin showed a surprising reduction of ejaculatory volume to 0ml, a complete dry ejaculation (47). Sato et al. reported an interesting study suggesting that silodosin prolonged IELT with 3-fold longer than baseline in APE patients, although it is a preliminary outcome in small number of patients (n=8) (Figure 3) (48).
Conclusions
The drug treatment for PE is still developing and some new promising therapeutic options have been proposed. Tramadol maybe stronger than SSRIs; however, it has a problem in the safety issue including addiction, which preventing this as the first-line treatment. Super selective alpha-1A blocker might be the next therapeutic strategy, although it leads to the dry-ejaculation. The large-scale RCT will be needed for these new options.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Althof SE, Abdo CH, Dean J, et al. International Society for Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med 2010;7:2947-69. [Crossref] [PubMed]
- McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride as needed: 2 single-blind placebo controlled crossover studies. J Urol 1999;161:1826-30. [Crossref] [PubMed]
- McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. J Urol 1998;159:1935-8. [Crossref] [PubMed]
- Atmaca M, Kuloglu M, Tezcan E, et al. The efficacy of citalopram in the treatment of premature ejaculation: a placebo-controlled study. Int J Impot Res 2002;14:502-5. [Crossref] [PubMed]
- Kara H, Aydin S, Yücel M, et al. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. J Urol 1996;156:1631-2. [Crossref] [PubMed]
- Althof SE, Levine SB, Corty EW, et al. A double-blind crossover trial of clomipramine for rapid ejaculation in 15 couples. J Clin Psychiatry 1995;56:402-7. [PubMed]
- Goodman RE. An assessment of clomipramine (Anafranil) in the treatment of premature ejaculation. J Int Med Res 1980;8 Suppl 3:53-9. [PubMed]
- Waldinger MD, Zwinderman AH, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol 2004;46:510-5; discussion 516. [Crossref] [PubMed]
- Waldinger MD, Zwinderman AH, Schweitzer DH, et al. Relevance of methodological design for the interpretation of efficacy of drug treatment of premature ejaculation: a systematic review and meta-analysis. Int J Impot Res 2004;16:369-81. [Crossref] [PubMed]
- McMahon CG. Premature ejaculation. Indian J Urol 2007;23:97-108. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An Update of the International Society of Sexual Medicine's Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex Med 2014;2:60-90. [Crossref] [PubMed]
- Meltzer HY, Ryan ND, Shaffer D, et al. ACNP Task Force report on SSRIs and suicidal behavior in youth. Neuropsychopharmacology 2006;31:473-92. [Crossref] [PubMed]
- Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ 2009;339:b2880. [Crossref] [PubMed]
- Khan A, Khan S, Kolts R, et al. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003;160:790-2. [Crossref] [PubMed]
- Black K, Shea C, Dursun S, et al. Selective serotonin reuptake inhibitor discontinuation syndrome: proposed diagnostic criteria. J Psychiatry Neurosci 2000;25:255-61. [PubMed]
- Tanrikut C, Feldman AS, Altemus M, et al. Adverse effect of paroxetine on sperm. Fertil Steril 2010;94:1021-6. [Crossref] [PubMed]
- Kim SW, Paick JS. Short-term analysis of the effects of as needed use of sertraline at 5 PM for the treatment of premature ejaculation. Urology 1999;54:544-7. [Crossref] [PubMed]
- Pryor JL, Althof SE, Steidle C, et al. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: an integrated analysis of two double-blind, randomised controlled trials. Lancet 2006;368:929-37. [Crossref] [PubMed]
- McMahon C, Kim SW, Park NC, et al. Treatment of premature ejaculation in the Asia-Pacific region: results from a phase III double-blind, parallel-group study of dapoxetine. J Sex Med 2010;7:256-68. [Crossref] [PubMed]
- Buvat J, Tesfaye F, Rothman M, et al. Dapoxetine for the treatment of premature ejaculation: results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. Eur Urol 2009;55:957-67. [Crossref] [PubMed]
- Porst H, McMahon CG, Althof SE, et al. Baseline characteristics and treatment outcomes for men with acquired or lifelong premature ejaculation with mild or no erectile dysfunction: integrated analyses of two phase 3 dapoxetine trials. J Sex Med 2010;7:2231-42. [Crossref] [PubMed]
- McMahon CG, Althof SE, Kaufman JM, et al. Efficacy and safety of dapoxetine for the treatment of premature ejaculation: integrated analysis of results from five phase 3 trials. J Sex Med 2011;8:524-39. [Crossref] [PubMed]
- McMahon CG, Giuliano F, Dean J, et al. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: randomized, placebo-controlled, phase III study. J Sex Med 2013;10:2312-25. [Crossref] [PubMed]
- Cormio L, Massenio P, La Rocca R, et al. The Combination of Dapoxetine and Behavioral Treatment Provides Better Results than Dapoxetine Alone in the Management of Patients with Lifelong Premature Ejaculation. J Sex Med 2015;12:1609-15. [Crossref] [PubMed]
- Dinsmore WW, Wyllie MG. PSD502 improves ejaculatory latency, control and sexual satisfaction when applied topically 5 min before intercourse in men with premature ejaculation: results of a phase III, multicentre, double-blind, placebo-controlled study. BJU Int 2009;103:940-9. [Crossref] [PubMed]
- Berkovitch M, Keresteci AG, Koren G. Efficacy of prilocaine-lidocaine cream in the treatment of premature ejaculation. J Urol 1995;154:1360-1. [Crossref] [PubMed]
- Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: a double-blind, randomized, placebo-controlled study. BJU Int 2004;93:1018-21. [Crossref] [PubMed]
- Pu C, Yang L, Liu L, et al. Topical anesthetic agents for premature ejaculation: a systematic review and meta-analysis. Urology 2013;81:799-804. [Crossref] [PubMed]
- Wieder JA, Brackett NL, Lynne CM, et al. Anesthetic block of the dorsal penile nerve inhibits vibratory-induced ejaculation in men with spinal cord injuries. Urology 2000;55:915-7. [Crossref] [PubMed]
- Aversa A, Pili M, Francomano D, et al. Effects of vardenafil administration on intravaginal ejaculatory latency time in men with lifelong premature ejaculation. Int J Impot Res 2009;21:221-7. [Crossref] [PubMed]
- Jannini EA, McMahon C, Chen J, et al. The controversial role of phosphodiesterase type 5 inhibitors in the treatment of premature ejaculation. J Sex Med 2011;8:2135-43. [Crossref] [PubMed]
- McMahon CG, Stuckey BG, Andersen M, et al. Efficacy of sildenafil citrate (Viagra) in men with premature ejaculation. J Sex Med 2005;2:368-75. [Crossref] [PubMed]
- Salonia A, Maga T, Colombo R, et al. A prospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J Urol 2002;168:2486-9. [Crossref] [PubMed]
- Asimakopoulos AD, Miano R, Finazzi Agrò E, et al. Does current scientific and clinical evidence support the use of phosphodiesterase type 5 inhibitors for the treatment of premature ejaculation? a systematic review and meta-analysis. J Sex Med 2012;9:2404-16. [Crossref] [PubMed]
- McMahon CG, McMahon CN, Leow LJ, et al. Efficacy of type-5 phosphodiesterase inhibitors in the drug treatment of premature ejaculation: a systematic review. BJU Int 2006;98:259-72. [Crossref] [PubMed]
- Sun Y, Luo D, Yang L, et al. Efficacy of Phosphodiesterase-5 Inhibitor in Men With Premature Ejaculation: A New Systematic Review and Meta-analysis. Urology 2015;86:947-54. [Crossref] [PubMed]
- Frink MC, Hennies HH, Englberger W, et al. Influence of tramadol on neurotransmitter systems of the rat brain. Arzneimittelforschung 1996;46:1029-36. [PubMed]
- Szkutnik-Fiedler D, Kus K, Balcerkiewicz M, et al. Concomitant use of tramadol and venlafaxine - evaluation of antidepressant-like activity and other behavioral effects in rats. Pharmacol Rep 2012;64:1350-8. [Crossref] [PubMed]
- Martyn-St James M, Cooper K, Kaltenthaler E, et al. Tramadol for premature ejaculation: a systematic review and meta-analysis. BMC Urol 2015;15:6. [Crossref] [PubMed]
- Takeshita J, Litzinger MH. Serotonin syndrome associated with tramadol. Prim Care Companion J Clin Psychiatry 2009;11:273. [Crossref] [PubMed]
- Lee JH. Associations between premature ejaculation, lower urinary tract symptoms, and erectile dysfunction in middle-aged Korean policemen. J Sex Med 2014;11:1512-8. [Crossref] [PubMed]
- Hisasue S, Furuya R, Itoh N, et al. Ejaculatory disorder caused by alpha-1 adrenoceptor antagonists is not retrograde ejaculation but a loss of seminal emission. Int J Urol 2006;13:1311-6. [Crossref] [PubMed]
- Beretta G, Chelo E, Fanciullacci F, et al. Effect of an alpha-blocking agent (phenoxybenzamine) in the management of premature ejaculation. Acta Eur Fertil 1986;17:43-5. [PubMed]
- Başar MM, Yilmaz E, Ferhat M, et al. Terazosin in the treatment of premature ejaculation: a short-term follow-up. Int Urol Nephrol 2005;37:773-7. [Crossref] [PubMed]
- Hsieh JT, Liu SP, Hsieh CH, et al. An in vivo evaluation of the therapeutic potential of sympatholytic agents on premature ejaculation. BJU Int 1999;84:503-6. [Crossref] [PubMed]
- Choi JH, Hwa JS, Kam SC, et al. Effects of tamsulosin on premature ejaculation in men with benign prostatic hyperplasia. World J Mens Health 2014;32:99-104. [Crossref] [PubMed]
- Kobayashi K, Masumori N, Hisasue S, et al. Inhibition of Seminal emission is the main cause of anejaculation induced by a new highly selective alpha1A-blocker in normal volunteers. J Sex Med 2008;5:2185-90. [Crossref] [PubMed]
- Sato Y, Tanda H, Nakajima H, et al. Silodosin and its potential for treating premature ejaculation: a preliminary report. Int J Urol 2012;19:268-72. [Crossref] [PubMed]


