Lengthening strategies for Peyronie’s disease
Introduction
Peyronie’s disease (PD) has clinically significant negative effects on patient quality of life and is associated with sexual dysfunction, negative self-image, depressive symptoms, and relationship problems (1). Surgical correction of curvature can restore quality of life and sexual function. However, side effects of surgery may include further loss of penile length, a consequence of PD which is independently and strongly associated with emotional distress and sexual dysfunction (2). In fact, men with greater than 2.5 cm subjective penile length loss due to PD are significantly more likely to report lower satisfaction with their own ability to perform sexual intercourse (3). Therefore, penile length restoration strategies are valuable methods by which a surgeon may help a patient with PD overcome or avoid emotional distress and sexual dysfunction.
In this paper, we review the effect of medical and surgical treatments for PD on length and provide a detailed review of the procedures specifically designed to increase penile length. A summary of the surgical techniques which preserve or increase penile length in men with PD can be found in Table 1. A video detailing the surgical techniques that increase penile length can be found in Figure S1.
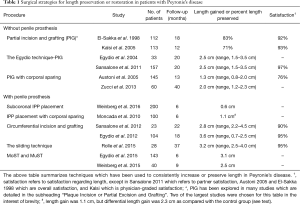
Full table

Effect of medical therapy on penile length
Medical therapies for PD are broadly divided into oral and injectable medications. Little evidence exists for the clinical efficacy of oral medications alone outside of combination therapy with other agents. Oral vitamin E, pentoxifylline, and tadalafil are each associated with decreased plaque size and curvature in men receiving simultaneous verapamil injection therapy (4-6). However, the effect of oral therapy alone on length has not been directly studied.
Common injection therapies for PD include verapamil, interferon-alpha 2b, and collagenase clostridium histolyticum (CCH). The efficacy of CCH has been demonstrated in two large scale clinical trials, IMPRESS I and II, which showed primary efficacy and safety regarding improvement in curvature and symptomatology, but did not demonstrate a change in penile length (7). The efficacy of verapamil injections has been widely studied both alone and in addition to other agents (5,6,8-12) and remains the subject of debate (13). We were not able to identify any studies of verapamil usage in which penile length was included among the outcomes.
Non-surgical therapy for PD is an evolving field with outcomes primarily evaluated on the basis of symptomatology and curvature rather than length. Based on current evidence, these therapies appear unlikely to have a significant effect on increasing or decreasing stretched penile length (SPL).
Surgical management techniques which may shorten penile length
Nesbit, Yachia, and plication procedures
There are several techniques which are typically used in men with minimal to moderate penile curvature that often result in the loss of penile length. These procedures, which include the Nesbit procedure and its modifications as well as penile plication, involve shortening the tunica on the convex side of the curvature directly opposite of the plaque. One review from 2014 identified 21 studies that report outcomes of tunical shortening procedures on post-operative penile length, with the majority reporting a significant percentage of men who lost length (14). The largest study on the Nesbit procedure, consisting of 359 men, found that 86.6% had shortening less than 1 inch, 8.6% between 1 and 2 inches, and 4.7% greater than 2 inches (15). The largest study on plication included 154 men and found that 25 (16%) lost length (mean 0.5 cm; range, 0.2–1.0 cm), but concluded that this loss of length was minimal (16). Therefore, though most patients do not lose substantial length from these techniques, patients who are candidates for these procedures must be counseled to expect a high probability of some penile length loss and should be selected with adequate pre-operative length.
Penile prostheses
Modeling with penile prostheses was first described by Wilson in 1994. Long-term outcomes were reported in 2001 that found that plaque modeling and penile prosthesis insertion is a safe and effective method for reducing curvature and treating erectile dysfunction (ED) associated with PD (17,18). The literature on penile length change in men with PD who are treated with inflatable penile prosthesis (IPP) is limited. A contemporary series of 90 patients who underwent IPP placement for PD reported that patients experienced a subjective penile length loss of 1.6 inches prior to the procedure and an additional 0.25 to 4 inches of subjective loss following the procedure. Overall, though objective measurements were not reported, 48% were dissatisfied with their post-operative length. Unfortunately, considering that loss of length is a common complaint following IPP placement in men regardless of the presence or absence of PD, these data highlight the importance of objective pre and post-operative measurements in studies on length (19).
The literature is conflicted on the relationship between IPP and penile length in the general population of men with ED and no concomitant PD. Several studies have found no difference or small increases in penile length following IPP. Deveci et al. in 2007 assessed the flaccid SPL of 56 men preoperatively and at 1 and 6 months postoperatively. There was no difference in measured SPL despite 71% endorsing subjective length loss. Men with subjective loss were more likely to be status post radical prostatectomy, so perceived length loss may have been secondary to surgically-induced ED prior to intervention with IPP (20). Another study from 2016 observing 45 men treated with the AMS 700 LGX IPP found that SPL increased 1.1±0.3 cm at 12 months (21).
Studies which examined erect penile length in men receiving IPP have shown an overall trend toward length loss. The first, published in 2009, included 11 prospectively enrolled patients. Wang and colleagues compared pre-operative erectile penile length achieved via intracavernosal injection (ICI) with post-operative erectile penile length achieved by IPP inflation and found that there were 0.83±0.25, 0.75±0.20 and 0.74±0.15 cm decreases in erect penile length 6 weeks, 6 months, and 1 year postoperatively (22). A similar study from 2014 examining 20 men found that median post-prosthesis penile length (13.5±2.13 cm) was smaller than preoperative pharmacologically induced length (14.25±2 cm) and that the majority of men treated with IPP lost length (23).
Although specific data in men with PD undergoing IPP is limited, subjective loss of length is commonly reported. In the general population of men with ED, objective data suggests that IPP placement results in only modest changes in penile length.
Surgical management techniques which increase or maintain penile length
Surgical techniques that maintain or increase penile length necessarily involve lengthening the tunica, particularly on the concave side of the curvature. In general, they are more involved procedures and therefore are recommended only for patients with a high degree of curvature and significant functional impairment. An important side effect of lengthening procedures is a consequence of the surgical technique itself. The tunical incisions that are necessary to allow for increased length may impair the vaso-occlusive mechanism necessary for erectile function, leading to the potential for difficulty with erections post-operatively. In fact, the procedures that produce the largest length gains are typically done with simultaneous IPP placement. Therefore, patients must be carefully selected according to pre-operative erectile function and counseled regarding risk of post-operative ED (7–46% depending on the technique and surgeon) (24).
Plaque incision (PI) or partial excision and grafting
While there are many variations on the technique, PI and grafting, in general, consists of a tunical incision on the concave aspect of the point of maximum curvature with grafting of the defect (25), and partial excision consists of dissection of the plaque off of the tunica with grafting of what is often a larger defect. Full excision is more likely to cause post-operative erectile dysfunction and is usually reserved for plaques that cause significant narrowing or corporal deformity (24,26,27).
PI and grafting was initially described by El-Sakka et al. The original procedure may be referred to as the Lue technique (25). However, evidence in the literature is conflicted regarding length outcomes for PI and grafting using this technique. In the original series of 112 patients, 83% of the men had stable or increased length following the procedure and 17% of men had decreased length. A subsequent study of 50 patients was notable for stable penile length in 60% of patients and decreased penile length in 40%, with long-term follow-up suggesting that more patients eventually progressed to decreased penile length (28). Another prospective study of 58 patients found that 22.4% had decreased penile length (range, 0.5–1.5 cm) (29). One of the largest studies, looking at 113 men, found that 25% had decreased penile length by >1 cm postoperatively (30). Another group of 58 patients were observed to have decreased penile length in 35% of men (31). Long term outcomes from 30 patients (mean follow-up 13 years) showed high satisfaction with the procedure (73% overall satisfaction), but are notable for high rates of ED (36.7%) and perceived penile shortening (43.3%) (32). Overall, while the majority of patients maintain penile length with this technique, a clinically significant minority are still reported to experience penile shortening (33).
The Egydio technique for PI and grafting was first described in 2002 and consists of a geometrically-based circumferential relaxing incision which is forked at the ends (34). Initial results in 33 patients demonstrated an intraoperative increase in SPL of 2.2 cm (range, 1–4 cm) (35). A total of 157 patients were enrolled in a multi-institutional outcomes study with median follow-up of 20 months in order to evaluate the Egydio technique. These patients had a median 2.5 cm (range, 1.5–3.5 cm) gain in penile length (36). However, this technique has been independently associated with ED and therefore patients must be selected appropriately (24).
Overall, the literature suggests that the Lue technique is likely to maintain or decrease penile length, but the Egydio technique is likely to increase penile length in men with PD while simultaneously elevating the risk of post-operative ED.
Plaque incision (PI) and grafting with corporal sparing silicone prosthesis placement
PI and grafting with silicone prosthesis placement increases penile length while retaining some native erectile function. Austoni et al. [2005] described a technique involving placement of a soft, axially rigid 10 Fr silicone prosthesis, which allows for some residual erectile function. Full thickness incisions were made into the tunica over the area of maximal bending until the penis could be fully elongated and relaxed. The defect was closed with a saphenous venous graft. For the 145 patients enrolled, average penile length increased by 1.3 cm (range, 0.8–2 cm) (37). Zucchi et al. in 2013 modified Austoni’s technique on 60 patients to use an 8 Fr prosthesis and a dovetail incision allowing for further curvature relaxation. This resulted in a larger defect requiring a bovine pericardial patch instead of the smaller venous graft. Mean shaft length increased by 2 cm (range, 1.2–2.3 cm) (38). Significantly, the authors reported that each patient maintained his gains in the 6 months following the procedure.
Surgical management techniques which increase or maintain penile length for men with severe comorbid ED
Innovative approaches to inflatable penile prosthesis (IPP) placement
There are some novel techniques for IPP insertion that may allow for greater length preservation in men with PD compared to traditional approaches. A recently reported series of 200 men (92 with PD) underwent IPP placement by a single surgeon utilizing a novel subcoronal approach (sc-IPP). The procedure begins with a subcoronal, “circumcision” incision and penile degloving. This allows for intraoperative assessment of penile pathology including PD. Then, repairs with relaxing incisions, grafting, and/or plication can be completed as needed. An IPP is inserted via two proximal, ventral corporotomy incisions after other pathology has been addressed. Using this method, patients gained a mean penile length of 0.6 cm. Complications included infection (1.5%) and one impending distal erosion requiring reoperation (39). Overall, since transitioning from the infrapubic to the subcoronal approach, the mean corporal length measurement has increased from 20.4±0.9 to 22.1±2.2 cm (P<0.0001, data is from abstract presented at the American Urological Association 2015 by Weinberg et al.).
The authors theorize that the dartos fascia may have inherent restrictive properties that prevent maximum relaxation and lengthening of the tunica albuginea, thereby tethering the penis and preventing complete relaxation and lengthening of the tunica albuginea. This effect may be more pronounced in men with longstanding ED and fibrosis of the corporal tissues. Upon degloving of the penis, in most cases they have observed an immediate gain in length when compared to the preoperative SPL. This difference in length may be attributed to the separation of the Dartos fascia from Buck’s fascia and allowing for full relaxation of the tunica albuginea. Furthermore, by having access to the tunica albuginea, there is the ability to perform other additional adjuvant procedures at the time of subcoronal penile prosthesis (scIPP), including relaxing incisions and aggressive modeling. In fact, 24% and 22% of patients had simultaneous plaque plication or relaxing incisions, respectively (39). The authors believe that the ability to routinely perform these adjuvant procedures no doubt adds to the length gains of this approach.
Other innovative approaches to IPP placement include aggressive cylinder sizing, post-operative inflation protocols, and corporal sparing techniques that limit the amount of corporal dilation. Aggressive cylinder sizing and post-operative inflation protocols are discussed in the section entitled “Post-Operative Inflation Protocols” below. With regard to corporal sparing techniques, one randomized study from 2010 included 100 patients, 50 of whom were controls who underwent IPP placement with standard corporal dilation and 50 of whom underwent the modified treatment without full corporal dilation. The control group experienced a 1.2-cm mean decrease in penile length while the treatment group had a 1.1-cm mean penile length increase (40).
Therefore, though IPP placement is traditionally associated with decreased SPL, newer techniques may allow for maintained or increased penile length.
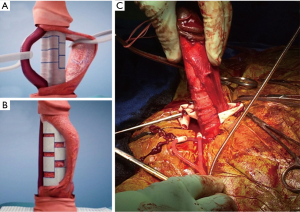
Circumferential incision and grafting
A technique for circumferential incision and grafting was proposed by Sansalone et al. in 2012 and was completed in 23 patients with an average follow-up of 22 months. Sansalone describes degloving the penis through a combined subcoronal and penoscrotal approach followed by dissecting Buck’s fascia [including the neurovascular bundle (NVB)] and the urethra off of the tunica albuginea. An artificial erection is made with saline injection at which point the girth of the tunical shaft is measured and the point of maximal curvature is identified by overlapping longitudinal lines. A circumferential incision is made at the point of maximum curvature in the tunica and the penis is pulled to full stretch as limited by the length of the NVB. A graft is made from InteXen using the previously obtained girth measurement, and the measured tunical defects from the concave and convex aspects of the point of maximum curvature. The graft is placed and the IPP is then inserted through two proximal corporotomy incisions. The average length gain was 2.8 cm (range, 2.2–4.5 cm). A total of 20% of patients reported diminished glans sensitivity and 13% had residual curvature less than 15 degrees. Ultimately, 90% were satisfied with the cosmetic and functional result of the procedure (41,42).
The Egydio technique using circular and longitudinal grafting aims to achieve maximum penile length as defined by the full length of the NVB. A subcoronal incision is made and the penis is degloved. Two longitudinal incisions are made lateral to the NVB to dissect the NVB off of the tunica albuginea. An erection is induced with medical injection therapy in order to determine the point of maximal curvature. A circumferential incision is made at the point of maximum curvature with the penis under tension. Egydio’s technique differs from that of Sansalone et al. (described above) in that the incision is started circularly on the concave side of the point of maximal curvature, but does not need to be completed circumferentially if length is limited by the NVB. Furthermore, instead of performing urethral mobilization in all cases, only the NVB is mobilized initially, and the surgeon may opt to dissect the urethra as well if it is noted to be a limiting factor in length. A penile prostheses (malleable was utilized in the original series) may be placed under direct visualization, and a graft material (bovine pericardium) placed based on the previously measured geometry of the incision. Narrowing can also be corrected in this technique using longitudinal tunical incisions. The initial study on this technique included 104 patients with mean functional penile length gain of 3.6 cm (range, 0.7–2.5 cm). Three patients developed retraction with residual curvature up to 30 degrees and 1 required explant for infection. Overall, 95.2% were satisfied with their post-operative length (42).
The sliding technique
The sliding technique was described by Rolle in a small series of 3 patients in 2012 and the results of a larger 28-patient European multicenter study were published in 2015. This technique uses a combined subcoronal and penoscrotal degloving incision followed by mobilization of the NVB and the urethra off of the corpora cavernosa. Next, two >4 cm longitudinal incisions are made in the lateral aspect of the tunica albuginea of each corpus cavernosum and joined by hemi-circumferential incisions (the proximal hemi-circular incision connects dorsally and the distal connects ventrally). This allows for complete transection of the corpora and the ability to stretch the penis to maximum corrected length, leaving two rectangular defects. The overlapping segments of tunica are sutured together under maximum stretch. Penile prostheses are placed and defects grafted with porcine small intestinal submucosa or collagen-fibrin sponge for IPP or malleable PP placement, respectively. Grafts may be placed following malleable penile prosthesis placement, but IPP should be inserted after grafting is complete because of the risk of suture damage to the device. Overall, this technique resulted in mean penile lengthening of 3.2 cm (range, 2.5–4 cm) and 95% of men were satisfied with their increased length. One patient (3.5%) on anticoagulation required a blood transfusion for profuse bleeding and 2 patients (7%) required device removal for infection. Of the 28.5% with penile hematoma, all were managed conservatively (43,44).
The modified sliding technique (MoST) and multiple slice technique (MuST)
MoST is a modification of the sliding technique described by Rolle in 2012, with the most notable differences being the use of a single subcoronal incision for penile degloving, as well as the mobilization and utilization of Buck’s fascia to cover defects in the tunica albuginea, obviating the necessity for graft material (Figure 1). The procedure begins with a circumferential subcoronal incision and degloving of the dartos fascia. Buck’s fascia is then incised just laterally to the urethra and dissected off of the corporal bodies circumferentially to isolate the NVB. An artificial erection is induced before mobilization of the corpus spongiosum off of the corpora cavernosa. The corporal bodies are marked ventrally in a semilunar manner from 3 to 9 o’clock 2–3 cm proximal from the coronal sulcus, dorsally from 9 to 3 o’clock 1.5 cm distal to the penoscrotal junction, and bilaterally via longitudinal markings that connect the prior dorsal/ventral markings. If an IPP is to be placed rather than malleable PP, two separate corporotomy incisions are made proximal to the penoscrotal junction for insertion of the IPP. The proximal semi-circular incision is then created and the corpora are dilated. Finally, the longitudinal and distal semi-circular incisions are completed. The penis can then be straightened and lengthened by sliding along the longitudinal incisions. The longitudinal tunical incisions are then sutured together at the point of overlap with the penis on stretch (45). The majority of patients in the initial series received malleable prostheses with insertion through the existing defect. However, some patients did receive an IPP which was placed via separate proximal corporotomy incisions. This technique is notable in that no graft material is used, allowing for a rectangular tunical defect in the proximal dorsal shaft. The distal ventral corpora defect is covered by the compressed cavernosum and the corpus spongiosum. Buck’s fascia is re-approximated to cover the proximal dorsal defect (45).
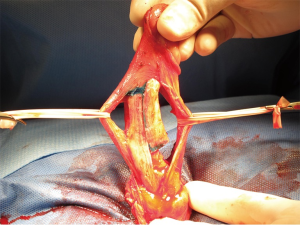
MuST is a modification of the MoST technique. Instead of a single set of longitudinal incisions and two hemi-circumferential tunical incisions as seen in the MoST technique, this procedure uses multiple pairs of hemi-circumferential incisions allowing for multiple sliding sections (Figure 2). The incisions are detailed in Figure 2. Further modification of the tunical incisions consists of multiple forked transverse incisions on the side of the curvature rather than using the sliding technique (Figure 3).
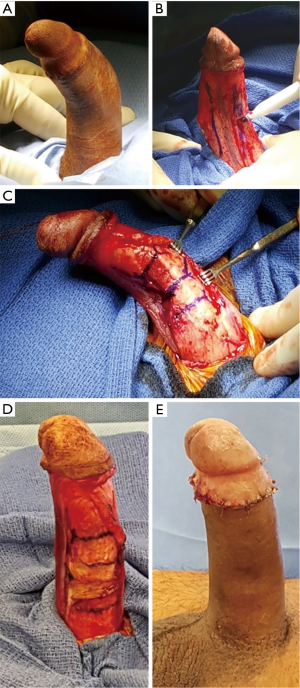
The MoST and MuST results were first described in abstract form at the 2014 Sexual Medicine Society of North America (SMSNA) and the 2015 AUA Annual Meetings, with outcomes first reported in the literature by Egydio et al. in 2015. In this series, 143 patients with ED had mean pre-operative subjective length loss of 3.4 cm, baseline IIEF of 24, and comorbid PD in 53.8%. All men underwent MoST or MuST procedures. Average length gain was 3.1 cm and IIEF increased to 60 at 6 months. Penile curvature was resolved in all patients and all patients were able to participate in sexual intercourse and achieve orgasm following the procedure. Complications included spontaneously resolving hematomas (24.5%), self-limited glans numbness (4.9%), and concerns about girth (9.8%) in a subgroup of patients receiving malleable prostheses (46). A multi-institutional study of 40 patients presenting to Columbia University Medical Center (CUMC) and New York University-Langone Medical Center (NYU), mean age 65, were treated with MoST (Data is from abstract presented at the Sexual Medicine Society of North America 2015 by Weinberg et al.). This study found that men treated with this procedures had a significant increase in SPL (mean 2.4 cm at CUMC and 2.6 cm at NYU; maintained at 9 months follow-up) and 100% maintained a postoperative ability to have sexual intercourse. Three patients had partial necrosis of a suture line and 1 had a hyper-mobile glans.
Adjuvant therapies to increase penile length
Penile traction therapy (PTT)
There is evidence that PTT can improve penile length in men with PD. A nonrandomized, prospective controlled trial of 96 men with acute phase PD receiving either PTT or no therapy found a decreased SPL in the group without therapy at 6 months (47). In addition, PTT has been shown to increase SPL 1.3±0.4 cm over 6 months in men complaining of small penile length (48). In addition, duration of PTT or PTT greater than 3 hours per day may improve SPL in men receiving verapamil injection therapy or interferon alpha-2b injection therapy, respectively (49,50). In fact, verapamil injection therapy in combination with oral L-arginine and pentoxifylline was associated with a 0.38-cm SPL gain for every hour of daily traction completed (49). A study of 10 men (2 with PD) who received PTT pre-operatively found that 70% had increased SPL following IPP placement, with mean increase in SPL postoperatively of 0.9 cm (range, 0–1.5 cm). Of the two patients with PD, one had no change in length and one gained 1.5 cm (51). Furthermore, PTT may help to preserve length post-operatively following partial incision and grafting. One non-randomized, retrospective study of 59 men who received partial excision and grafting found that men with PTT saw an increased SPL of 1.48 cm (range, 0–6 cm) vs. 0.24 cm (range, −1–2.5 cm) in the cohort without PTT. Notably, none of the men in the PTT cohort experienced subjective loss of SPL (52).
Post-operative inflation protocols
A multicenter, 40-patient study by Henry et al. from 2015, though notably excluding men with PD, examined men who received aggressive cylinder sizing with the Coloplast Titan IPP, including 6–12 months of daily post-operative inflation for 1–2 h daily. A total of 29% of men had increased size at 1 year compared to the pre-operative length. On average, men had increased length and girth (1.14±1.94 and 1.08±0.82 cm, respectively) at final 12-month follow-up (53). Despite the fact that this study did not report complications, the potential risks of aggressive sizing include erosion and other complications. Although specific data on aggressive sizing and inflation protocols are lacking among specific cohorts of men with PD, it is reasonable to extrapolate this data and apply techniques of sizing, molding, and inflation among men with PD.
Medical therapy for glans engorgement
Some of the complaints concerning decreased penile length in men with PD and comorbid ED following intervention may be explained by decreased glans engorgement or a “cold” glans. For these men, medical therapies may help patients achieve satisfaction with their penile length.
Intraurethral alprostadil has been demonstrated to be an effective adjuvant therapy for patients who can tolerate the discomfort associated with intraurethral placement (54,55). The largest study examined 17 men with “cold” glans following IPP placement. Of these men, 10 were satisfied with the therapy, 11 continued with treatment after the initial dose, and 7 discontinued or were dissatisfied because of prohibitive penile pain (54).
Sildenafil citrate has also been used in men with decreased glans engorgement following placement of IPP. For men who responded to therapy with increased glans engorgement, patient satisfaction with the procedures increased (56).
Adjuvant surgical therapy
There are several surgical techniques which can be used in an adjuvant manner to increase subjective and/or objective penile length in a patient who is already receiving surgical intervention for PD. These include suspensory ligament release, suprapubic lipectomy, and ventral phalloplasty.
Suspensory ligament release has been examined in several series. One series of 42 patients of whom 27 (64%) had PD primarily examined men with suspensory ligament release, but also examined men with simultaneous suprapubic lipectomy and silicone buffer placement. These men experienced an increased SPL of 1.3 cm (±0.9 cm). Notably, insertion of a silicone buffer was significantly associated with increased SPL, likely because this prevented suspensory ligament reattachment, a complication which can cause contractures (57). The largest English language series we identified, from Borges et al. in 2006, examined 303 men who had suspensory ligament release at the time of IPP placement. 93% were satisfied with the procedure and only 1.3% reported subjective loss of penile length. Of the 18 patients enrolled in a subset of this study which directly measured penile length, flaccid SPL increased 2.4 cm (range, 1.4–3.2 cm) and erect penile length increased 1.7 cm (range, 1.1–2.3 cm) (58). As the primary post-operative concern with this procedure is suspensory ligament reattachment causing contracture, surgical techniques that may prevent this are an ongoing area of discovery in the literature (59,60).
Suprapubic lipectomy involves removing the adipose tissue surrounding the base of the penis and often occurs with simultaneous release of the suspensory ligaments or dartos fascia (61). It was first described by Horton et al. in 1987 in boys with congenital buried penis (62). Suprapubic adiposity can bury the proximal portion of the shaft, leading to a perception of decreased penile length. This technique can be combined with abdominoplasty in overweight individuals, often with the assistance of a plastic surgeon (63).
Vental phalloplasty, a procedure based on the common pediatric procedure to correct a webbed penis, involves surgical release of the ventral penoscrotal web. First described in 2007 as an adjuvant designed to increase patient satisfaction with IPP placement, several studies have shown that ventral phalloplasty increases perceived penile length in the majority of patients (61,64-66). However, patients who receive ventral phalloplasty are at high risk for wound dehiscence, especially if there are diabetic. Of the 102 men who underwent ventral phalloplasty, 15 were found of have wound dehiscence (1 of which required reoperation). The odds ratio for dehiscence was 9.8 in men with diabetes (67).
These techniques may be used to increased perceived or objective penile length in order to improve patient satisfaction and cosmetic outcomes for men undergoing surgical intervention for PD.
Discussion and conclusions
There are several techniques for maintaining or lengthening the penis in men with PD. For men without ED or significant curvature, plication is likely to conserve length or minimize length loss. For men with a high degree of curvature and good erectile function, partial incision and grafting is likely to maintain penile length and may gain length in some men, though risk of post-operative ED is significant. For men with comorbid PD and ED, sc-IPP, circumferential incision and grafting, the sliding technique, MoST, and MuST all appear to be safe and effective ways to gain penile length with concomitant prosthesis placement. Carefully selected adjuvant therapies are likely to help men with PD maintain or increase perceived and/or objective penile length. Importantly, the penile lengthening strategies performed simultaneously with penile prosthesis insertion have only been studied in the hands of high-volume implanters. Therefore, in order to avoid unnecessary and debilitating complications, these procedures should be reserved for implanters with extensive experience.
Acknowledgements
We would like to thank Gary Crumpler for creating animations used in Figure S1.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rosen R, Catania J, Lue T, et al. Impact of Peyronie's disease on sexual and psychosocial functioning: qualitative findings in patients and controls. J Sex Med 2008;5:1977-84. [Crossref] [PubMed]
- Smith JF, Walsh TJ, Conti SL, et al. Risk factors for emotional and relationship problems in Peyronie's disease. J Sex Med 2008;5:2179-84. [Crossref] [PubMed]
- Kueronya V, Miernik A, Stupar S, et al. International multicentre psychometric evaluation of patient-reported outcome data for the treatment of Peyronie's disease. BJU Int 2015;115:822-8. [Crossref] [PubMed]
- Paulis G, Brancato T, D'Ascenzo R, et al. Efficacy of vitamin E in the conservative treatment of Peyronie's disease: legend or reality? A controlled study of 70 cases. Andrology 2013;1:120-8. [Crossref] [PubMed]
- Alizadeh M, Karimi F, Fallah MR. Evaluation of verapamil efficacy in Peyronie's disease comparing with pentoxifylline. Glob J Health Sci 2014;6:23-30. [Crossref] [PubMed]
- Dell'Atti L. Tadalafil once daily and intralesional verapamil injection: A new therapeutic direction in Peyronie's disease. Urol Ann 2015;7:345-9. [PubMed]
- Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol 2013;190:199-207. [Crossref] [PubMed]
- Favilla V, Russo GI, Privitera S, et al. Combination of intralesional verapamil and oral antioxidants for Peyronie's disease: a prospective, randomised controlled study. Andrologia 2014;46:936-42. [Crossref] [PubMed]
- Garrido Abad P, Coloma A, Herranz LM, et al. Transdermal iontophoresis with verapamil and dexamethasone in the acute phase of peyronie's disease. Our experience. Arch Esp Urol 2012;65:745-51. [PubMed]
- Mehrsai AR, Namdari F, Salavati A, et al. Comparison of transdermal electromotive administration of verapamil and dexamethasone versus intra-lesional injection for Peyronie's disease. Andrology 2013;1:129-32. [Crossref] [PubMed]
- Moskovic DJ, Alex B, Choi JM, et al. Defining predictors of response to intralesional verapamil injection therapy for Peyronie's disease. BJU Int 2011;108:1485-9. [Crossref] [PubMed]
- Paulis G, Cavallini G, Giorgio GD, et al. Long-term multimodal therapy (verapamil associated with propolis, blueberry, vitamin E and local diclofenac) on patients with Peyronie's disease (chronic inflammation of the tunica albuginea). Results of a controlled study. Inflamm Allergy Drug Targets 2013;12:403-9. [Crossref] [PubMed]
- Levine LA, Costabile RA. Is intralesional verapamil effective therapy for Peyronie's disease? J Urol 2012;188:704-6. [Crossref] [PubMed]
- Zaid UB, Alwaal A, Zhang X, et al. Surgical management of Peyronie's disease. Curr Urol Rep 2014;15:446. [Crossref] [PubMed]
- Ralph DJ, al-Akraa M, Pryor JP. The Nesbit operation for Peyronie's disease: 16-year experience. J Urol 1995;154:1362-3. [Crossref] [PubMed]
- Hudak SJ, Morey AF, Adibi M, et al. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol 2013;189:1019-24. [Crossref] [PubMed]
- Wilson SK, Cleves MA, Delk JR 2nd. Long-term followup of treatment for Peyronie's disease: modeling the penis over an inflatable penile prosthesis. J Urol 2001;165:825-9. [Crossref] [PubMed]
- Wilson SK, Delk JR 2nd. A new treatment for Peyronie's disease: modeling the penis over an inflatable penile prosthesis. J Urol 1994;152:1121-3. [PubMed]
- Levine LA, Benson J, Hoover C. Inflatable penile prosthesis placement in men with Peyronie's disease and drug-resistant erectile dysfunction: A single-center study. J Sex Med 2010;7:3775-83. [Crossref] [PubMed]
- Deveci S, Martin D, Parker M, et al. Penile length alterations following penile prosthesis surgery. Eur Urol 2007;51:1128-31. [Crossref] [PubMed]
- Negro CL, Paradiso M, Rocca A, et al. Implantation of AMS 700 LGX penile prosthesis preserves penile length without the need for penile lengthening procedures. Asian J Androl 2016;18:114-7. [Crossref] [PubMed]
- Wang R, Howard GE, Hoang A, et al. Prospective and long-term evaluation of erect penile length obtained with inflatable penile prosthesis to that induced by intracavernosal injection. Asian J Androl 2009;11:411-5. [Crossref] [PubMed]
- Osterberg EC, Maganty A, Ramasamy R, et al. Pharmacologically induced erect penile length and stretched penile length are both good predictors of post-inflatable prosthesis penile length. Int J Impot Res 2014;26:128-31. [Crossref] [PubMed]
- Flores S, Choi J, Alex B, et al. Erectile dysfunction after plaque incision and grafting: short-term assessment of incidence and predictors. J Sex Med. 2011;8:2031-7. [Crossref] [PubMed]
- El-Sakka AI, Rashwan HM, Lue TF. Venous patch graft for Peyronie's disease. Part II: outcome analysis. J Urol 1998;160:2050-3. [Crossref] [PubMed]
- Levine LA. Partial plaque excision and grafting (PEG) for Peyronie's disease. J Sex Med 2011;8:1842-5. [Crossref] [PubMed]
- Levine LA, Estrada CR. Human cadaveric pericardial graft for the surgical correction of Peyronie's disease. J Urol 2003;170:2359-62. [Crossref] [PubMed]
- Montorsi F, Salonia A, Maga T, et al. Evidence based assessment of long-term results of plaque incision and vein grafting for Peyronie's disease. J Urol 2000;163:1704-8. [Crossref] [PubMed]
- Akkus E, Ozkara H, Alici B, et al. Incision and venous patch graft in the surgical treatment of penile curvature in Peyronie's disease. Eur Urol 2001;40:531-6; discussion 537. [Crossref] [PubMed]
- Kalsi J, Minhas S, Christopher N, et al. The results of plaque incision and venous grafting (Lue procedure) to correct the penile deformity of Peyronie's disease. BJU Int 2005;95:1029-33. [Crossref] [PubMed]
- Adeniyi AA, Goorney SR, Pryor JP, et al. The Lue procedure: an analysis of the outcome in Peyronie's disease. BJU Int 2002;89:404-8. [Crossref] [PubMed]
- Wimpissinger F, Parnham A, Gutjahr G, et al. 10 years' plaque incision and vein grafting for Peyronie's disease: does time matter? J Sex Med 2016;13:120-8. [Crossref] [PubMed]
- Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med 2008;5:2221-8; discussion 2229-30. [Crossref] [PubMed]
- Egydio PH, Lucon AM, Arap S. A single relaxing incision to correct different types of penile curvature: surgical technique based on geometrical principles. BJU Int 2004;94:1147-57. [Crossref] [PubMed]
- Egydio PH, Lucon AM, Arap S. Treatment of Peyronie's disease by incomplete circumferential incision of the tunica albuginea and plaque with bovine pericardium graft. Urology 2002;59:570-4. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Long-term results of the surgical treatment of Peyronie's disease with Egydio's technique: a European multicentre study. Asian J Androl 2011;13:842-5. [Crossref] [PubMed]
- Austoni E, Colombo F, Romanò AL, et al. Soft prosthesis implant and relaxing albugineal incision with saphenous grafting for surgical therapy of Peyronie's disease: a 5-year experience and long-term follow-up on 145 operated patients. Eur Urol 2005;47:223-9; discussion 229. [Crossref] [PubMed]
- Zucchi A, Silvani M, Pecoraro S. Corporoplasty with small soft axial prostheses (VIRILIS I®) and bovine pericardial graft (HYDRIX®) in Peyronie's disease. Asian J Androl 2013;15:275-9. [Crossref] [PubMed]
- Weinberg AC, Pagano MJ, Deibert CM, et al. Sub-coronal inflatable penile prosthesis placement with modified no-touch technique: a step-by-step approach with outcomes. J Sex Med 2016;13:270-6. [Crossref] [PubMed]
- Moncada I, Martínez-Salamanca JI, Jara J, et al. Inflatable penile prosthesis implantation without corporeal dilation: a cavernous tissue sparing technique. J Urol 2010;183:1123-6. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie's disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316-21. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE, Sansalone S. Penile length and girth restoration in severe Peyronie's disease using circular and longitudinal grafting. BJU Int 2013;111:E213-9. [Crossref] [PubMed]
- Rolle L, Falcone M, Ceruti C, et al. A prospective multicentric international study on the surgical outcomes and patients' satisfaction rates of the 'sliding' technique for end-stage Peyronie's disease with severe shortening of the penis and erectile dysfunction. BJU Int 2016;117:814-20. [Crossref] [PubMed]
- Rolle L, Ceruti C, Timpano M, et al. A new, innovative, lengthening surgical procedure for Peyronie's disease by penile prosthesis implantation with double dorsal-ventral patch graft: the "sliding technique". J Sex Med 2012;9:2389-95. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE, Valenzuela RJ. Modified sliding technique (MoST) for penile lengthening with Insertion of Inflatable Penile Prosthesis. J Sex Med 2015;12:1100-4. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified 'sliding' technique. BJU Int 2015;116:965-72. [Crossref] [PubMed]
- Martínez-Salamanca JI, Egui A, Moncada I, et al. Acute phase Peyronie's disease management with traction device: a nonrandomized prospective controlled trial with ultrasound correlation. J Sex Med 2014;11:506-15. [Crossref] [PubMed]
- Nowroozi MR, Amini E, Ayati M, et al. Applying extender devices in patients with penile dysmorphophobia: assessment of tolerability, efficacy, and impact on erectile function. J Sex Med 2015;12:1242-7. [Crossref] [PubMed]
- Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie's disease. J Sex Med 2012;9:288-95. [Crossref] [PubMed]
- Yafi FA, Pinsky MR, Stewart C, et al. The effect of duration of penile traction therapy in patients undergoing intralesional injection therapy for Peyronie's disease. J Urol 2015;194:754-8. [Crossref] [PubMed]
- Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. [Crossref] [PubMed]
- Rybak J, Papagiannopoulos D, Levine L. A retrospective comparative study of traction therapy vs. no traction following tunica albuginea plication or partial excision and grafting for Peyronie's disease: measured lengths and patient perceptions. J Sex Med 2012;9:2396-403. [Crossref] [PubMed]
- Henry GD, Carrion R, Jennermann C, et al. Prospective evaluation of postoperative penile rehabilitation: penile length/girth maintenance 1 year following Coloplast Titan inflatable penile prosthesis. J Sex Med 2015;12:1298-304. [Crossref] [PubMed]
- Benevides MD, Carson CC. Intraurethral application of alprostadil in patients with failed inflatable penile prosthesis. J Urol 2000;163:785-7. [Crossref] [PubMed]
- Chew KK, Stuckey BG. Use of transurethral alprostadil (MUSE) (prostaglandin E1) for glans tumescence in a patient with penile prosthesis. Int J Impot Res 2000;12:195-6. [Crossref] [PubMed]
- Mulhall JP, Jahoda A, Aviv N, et al. The impact of sildenafil citrate on sexual satisfaction profiles in men with a penile prosthesis in situ. BJU Int 2004;93:97-9. [Crossref] [PubMed]
- Li CY, Kayes O, Kell PD, et al. Penile suspensory ligament division for penile augmentation: indications and results. Eur Urol 2006;49:729-33. [Crossref] [PubMed]
- Borges F, Hakim L, Kline C. Surgical technique to maintain penile length after insertion of an inflatable penile prosthesis via infrapubic approach. J Sex Med 2006;3:550-3. [Crossref] [PubMed]
- Mokhless IA, Abdeldaeim HM, Rahman A, et al. Penile advancement and lengthening for the management of post-circumcision traumatic short penis in adolescents. Urology 2010;76:1483-7. [Crossref] [PubMed]
- Srinivas BV, Vasan SS, Mohammed S. Penile lengthening procedure with V-Y advancement flap and an interposing silicone sheath: a novel methodology. Indian J Urol 2012;28:340-2. [Crossref] [PubMed]
- Hakky TS, Suber J, Henry G, et al. Penile enhancement procedures with simultaneous penile prosthesis placement. Adv Urol 2012;2012:314612.
- Horton CE, Vorstman B, Teasley D, et al. Hidden penis release: adjunctive suprapubic lipectomy. Ann Plast Surg 1987;19:131-4. [Crossref] [PubMed]
- Adham MN, Teimourian B, Mosca P. Buried penis release in adults with suction lipectomy and abdominoplasty. Plast Reconstr Surg 2000;106:840-4. [Crossref] [PubMed]
- Caso J, Keating M, Miranda-Sousa A, et al. Ventral phalloplasty. Asian J Androl 2008;10:155-7. [Crossref] [PubMed]
- Miranda-Sousa A, Keating M, Moreira S, et al. Concomitant ventral phalloplasty during penile implant surgery: a novel procedure that optimizes patient satisfaction and their perception of phallic length after penile implant surgery. J Sex Med 2007;4:1494-9. [Crossref] [PubMed]
- Hakky TS, Rodriguez AR, Parker J, et al. Ventral phalloplasty. Int Braz J Urol 2012;38:565-6. [Crossref] [PubMed]
- Sulaver R II, Welliver R, Kottwitz M, et al. PD26-08 scrotoplasty at time of penile implant is at high risk for dehiscence in diabetics. J Urol 2015;193:e569. [Crossref]
- Gaffney CD, Pagano MJ, Weinberg AC, et al. Surgical techniques that increase penile length. Asvide 2016;3:228. Available online: http://www.asvide.com/articles/987


